Abstract
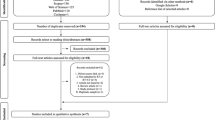
Photobiomodulation (PBM) therapy is an effective method for preventing and managing oral mucositis (OM) in head and neck squamous cell carcinoma (HNSCC) patients undergoing radiotherapy alone or in combination with chemotherapy. However, the potential effects of PBM therapy on premalignant and malignant cells eventually present in the treatment site are yet unknown. The aim of this systematic review was to analyze the effects of PBM therapy on HNSCC. A literature search was conducted in four indexed databases as follows: MEDLINE/PubMed, EMBASE, Web of Science, and Scopus. The databases were reviewed for papers published up to and including in October 2018. In vitro and in vivo studies that investigated the effects of PBM therapy on HNSCC were selected. From the 852 initially gathered studies, 15 met the inclusion criteria (13 in vitro and 2 in vivo). Only three in vitro studies were noted to have a low risk of bias. The included data demonstrated wide variations of study designs, PBM therapy protocols, and study outcomes. Cell proliferation and viability were the primary evaluation outcome in the in vitro studies. Of the 13 in vitro studies, seven noted a positive effect of PBM therapy on inhibiting or preventing an effect on HNSCC tumor cells, while six studies saw increased proliferation. One in vivo study reported increased oral SCC (OSCC) progression, while the other observed reduced tumor progression. Overall, the data from the studies included in the present systematic review do not support a clear conclusion about the effects of PBM therapy on HNSCC cells.
Similar content being viewed by others
References
P. J. Thomson, Perspectives on oral squamous cell carcinoma prevention-proliferation, position, progression and prediction, J. Oral Pathol. Med., 2018, 47, 803–807.
S. Chen, H. Hu, S. Miao, J. Zheng, Z. Xie and H. Zhao, Antitumor effect of cisplatin in human oral squamous cell carcinoma was enhanced by andrographolide via upregulation of phospho-p53 in vitro and in vivo, Tumour Biol., 2017, 39(5), 1010428317705330.
S. T. Sonis, Oral mucositis in head and neck cancer: risk, biology, and management, Am. Soc. Clin. Oncol. Educ. Book, 2013, DOI: 10.1200/EdBook_AM.2013.33.e236.
S. Minhas, et al., Concomitant-chemoradiotherapy-associated oral lesions in patients with oral squamouscell carcinoma, Cancer Biol. Med., 2017, 14, 176–182.
F. Amadori, et al., Low-level laser therapy for treatment of chemotherapy-induced oral mucositis in childhood: a randomized double-blind controlled study, Lasers Med. Sci., 2016, 31, 1231–1236.
H. S. Antunes, et al., Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis, Oral Oncol., 2017, 71, 11–15.
L. M. Bezinelli, et al., Cost-effectiveness of the introduction of specialized oral care with laser therapy in hematopoietic stem cell transplantation, Hematol. Oncol., 2014, 32, 31–39.
R. V. Lalla, et al., MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy, Cancer, 2014, 120, 1453–1461.
J. A. Zecha, et al., Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer. Part 1: mechanisms of action, dosimetric, and safety considerations, Support Care Cancer, 2016, 24, 2781–2792.
J. J. Anders, et al., Low-level light/laser therapy versus photobiomodulation therapy, Photomed. Laser Surg., 2015, 33, 183–184.
P. R. Arany, Craniofacial Wound Healing with Photobiomodulation Therapy: New Insights and Current Challenges, J. Dent. Res., 2016, 95, 977–984.
N. N. Lopes, et al., Cyclooxygenase-2 and vascular endothelial growth factor expression in 5-fluorouracil-induced oral mucositis in hamsters: evaluation of two low-intensity laser protocols, Support Care Cancer, 2009, 17, 1409–1415.
N. N. Lopes, et al., Effects of low-level laser therapy on collagen expression and neutrophil infiltrate in 5-fluorouracilinduced oral mucositis in hamsters, Lasers Surg. Med., 2010, 42, 546–552.
T. C. Lopez, et al., Effect of laser phototherapy in the prevention and treatment of chemo-induced mucositis in hamsters, Braz. Oral Res., 2013, 27, 342–348.
M. Curra, et al., Photobiomodulation reduces oral mucositis by modulating NF-kB, J. Biomed. Opt., 2015, 20, 125008.
A. F. Oton-Leite, et al., Effect of low-level laser therapy on chemoradiotherapy-induced oral mucositis and salivary inflammatory mediators in head and neck cancer patients, Lasers Surg. Med., 2015, 47, 296–305.
M. M. Schubert, et al., A phase III randomized doubleblind placebo-controlled clinical trial to determine the efficacy of low level laser therapy for the prevention of oral mucositis in patients undergoing hematopoietic cell transplantation, Support Care Cancer, 2007, 15, 1145–1154.
B. Ferreira, F. M. da Motta Silveira and F. A. de Orange, Low-level laser therapy prevents severe oral mucositis in patients submitted to hematopoietic stem cell transplantation: a randomized clinical trial, Support Care Cancer, 2016, 24(3), 1035–1042.
M. Schaffer, et al., Biomodulative effects induced by 805 nm laser light irradiation of normal and tumor cells, J. Photochem. Photobiol., B, 1997, 40, 253–257.
R. Sroka, et al., Effects on the mitosis of normal and tumor cells induced by light treatment of different wavelengths, Lasers Surg. Med., 1999, 25, 263–271.
V. H. Schartinger, et al., Differential responses of fibroblasts, non-neoplastic epithelial cells, and oral carcinoma cells to low-level laser therapy, Support Care Cancer, 2012, 20, 523–529.
J. S. Monteiro, et al., Influence of laser phototherapy (λ660 nm) on the outcome of oral chemical carcinogenesis on the hamster cheek pouch model: histological study, Photomed. Laser Surg., 2011, 29, 741–745.
W. Z. Liang, et al., Selective cytotoxic effects of low-power laser irradiation on human oral cancer cells, Lasers Surg. Med., 2015, 47, 756–764.
Y. H. Rhee, et al., Low-Level Laser Therapy Promoted Aggressive Proliferation and Angiogenesis through decreasing Transforming Growth Factor-β1 and Increasing of Akt/Hypoxia Inducible Factor-1α in Anaplastic Thyroid Cancer, Photomed. Laser Surg., 2016, 34, 229–235.
M. Myakishev-Rempel, et al., A preliminary study of the safety of red light phototherapy of tissues harboring cancer, Photomed. Laser Surg., 2012, 30, 551–558.
S. T. Sonis, et al., Could the biological robustness of low level laser therapy (Photobiomodulation) impact its use in the management of mucositis in head and neck cancer patients, Oral Oncol., 2016, 54, 7–14.
D. Moher, et al., Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, Ann. Intern. Med., 2009, 151, 264–269.
M. M. Marques, et al., Photobiomodulation of Dental Derived Mesenchymal Stem Cells: A Systematic Review, Photomed. Laser Surg., 2016, 34, 500–508.
C. R. Hooijmans, et al., SYRCLE’s risk of bias tool for animal studies, BMC Med. Res. Methodol., 2014, 26(14), 43.
A. L. Pinheiro, et al., Does LLLT stimulate laryngeal carcinoma cells? An in vitro study, Braz. Dent. J., 2002a, 13, 109–112.
A. L. Pinheiro, et al., Effects of low-level laser therapy on malignant cells: in vitro study, J. Clin. Laser Med. Surg., 2002b, 20, 23–26.
M. Kreisler, et al., Low-level 809 nm GaAlAs laser irradiation increases the proliferation rate of human laryngeal carcinoma cells in vitro, Lasers Med. Sci., 2003, 18, 100–103.
J. L. Castro, et al., The effect of laser therapy on the proliferation of oral KB carcinoma cells: an in vitro study, Photomed. Laser Surg., 2005, 23, 586–589.
C. E. Werneck, et al., Laser light is capable of inducing proliferation of carcinoma cells in culture: a spectroscopic in vitro study, Photomed. Laser Surg., 2005, 23, 300–303.
F. F. Sperandio, et al., Low-level laser therapy can produce increased aggressiveness of dysplastic and oral cancer cell lines by modulation of Akt/mTOR signaling pathway, J. Biophotonics, 2013, 6, 839–847.
A. C. Henriques, et al., Low-level laser therapy promotes proliferation and invasion of oral squamous cell carcinoma cells, Lasers Med. Sci., 2014, 29, 1385–1395.
T. Schalch, et al., Photomodulation of the osteoclastogenic potential of oral squamous carcinoma cells, J. Biophotonics, 2016, 9, 1136–1147.
G. Ottaviani, et al., Laser Therapy Inhibits Tumor Growth in Mice by Promoting Immune Surveillance and Vessel Normalization, EBioMedicine, 2016, 11, 165–172.
T. D. Schalch, et al., Photobiomodulation is associated with a decrease in cell viability and migration in oral squamous cell carcinoma, Lasers Med. Sci., 2018, 34, 629–636.
J. M. Bjordal, et al., A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis, Support Care Cancer, 2011, 19, 1069–1077.
R. J. Bensadoun, Photobiomodulation or low-level laser therapy in the management of cancer therapy-induced mucositis, dermatitis and lymphedema, Curr. Opin. Oncol., 2018, 30, 226–232.
K. M. AlGhamdi, et al., Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells, Lasers Med. Sci., 2012, 27, 237–249.
Τ. B. Brandão, et al., Locally advanced oral squamous cell carcinoma patients treated with photobiomodulation for prevention of oral mucositis: retrospective outcomes and safety analyses, Support Care Cancer, 2018, 26, 2417–2423.
P. R. Arany, Healing Tumors with Light: Science Fiction or the Future of Medicine?, Photomed. Laser Surg., 2018, 36, 227–229.
M. R. Hamblin, Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation, Photochem. Photobiol., 2018, 94, 199–212.
M. R. Hamblin, et al., Photobiomodulation and Cancer: What Is the Truth?, Photomed. Laser Surg., 2018, 36, 241–245.
J. P. Gillet, et al., The clinical relevance of cancer cell lines, J. Natl. Cancer Inst., 2013, 105, 452–458.
I. Khan and P. R. Arany, Dosimetery for Photobiomodulation therapy: Response to Sommers, et al., Ann. Transl. Med., 2016, 4, 208.
P. A. Jenkins and J. D. Carroll, How to report low-level laser therapy (LLLT)/photomedicine dose and beam parameters in clinical and laboratory studies, Photomed. Laser Surg., 2011, 29, 785–787.
J. Tuner and P. A. Jenkins, Parameter Reproducibility in Photobiomodulation, Photomed. Laser Surg., 2016, 34, 91–92.
K. W. Engel, et al., Cell lineage responses to photobiomodulation therapy, J. Biophotonics, 2016, 9, 1148–1156.
S. Elad, et al., Photobiomodulation therapy in the management of oral mucositis: search for the optimal clinical treatment parameters, Support Care Cancer, 2018, 26, 3319–3321.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silveira, F.M., de Paglioni, M.P., Marques, M.M. et al. Examining tumor modulating effects of photobiomodulation therapy on head and neck squamous cell carcinomas. Photochem Photobiol Sci 18, 1621–1637 (2019). https://doi.org/10.1039/c9pp00120d
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1039/c9pp00120d