Abstract
Due to distinct biological behavior of mucinous adenocarcinoma (MAC) and signet ring cell cancer (SRC), the efficacy of radiotherapy on long-term outcome for rectal cancer (RC) patients with mucinous tumors is still unclear. Here, we identified 1808 RC patients with MAC/SRC from Surveillance, Epidemiology, and End-Results (SEER) database from 2004 to 2013. Patients were divided into two subgroups according to different therapeutic strategies, including surgery alone and surgery combined with radiotherapy. Kaplan–Meier methods and Cox regression models were used to access the influence of therapeutic strategy on long-term survival outcomes. The 5-year and 10-year cancer specific survival (CSS) were improved in stage II and III patients who underwent surgery and radiotherapy compared with patients who underwent surgery alone. These results were further confirmed following propensity score matching. In addition, radiotherapy was deemed as independent good prognostic factor in patient with MAC/SRC. In subgroup analysis, the result also demonstrated that long-term survival was improved following radiotherapy. However, there was no prognostic difference between preoperative and postoperative radiotherapy. In conclusion, radiotherapy could improve survival for RC patients with MAC and SRC, but only for patients in stage II and III. This finding supported the application of radiotherapy in clinical practice.
Similar content being viewed by others
Introduction
Accumulating studies have shown that the administration of surgery combined with radiotherapy has significantly improved local control and decreased the incidence of local recurrences for patients with rectal cancer (RC)1,2,3,4. This combined treatment modality has been considered as standard therapy for patients with locally advanced RC. Despite the recommendation of radiotherapy to RC patients, the tumor response and prognostic outcome are variable to radiotherapy5. The histological type of RC may play a vital role for this variation6.
Most commonly studied subtypes of RC include mucinous adenocarcinoma (MAC) and signet ring cell cancer (SRC). Both histologies are differentiated from standard adenocarcinoma by levels of mucin within the tumor. MAC is defined as a tumor possessing more than 50% of the lesion being composed of extracellular mucin produced by tumor acinar cells. SRC is another variant subtype that contains a large amount of intracytoplasmic mucin, which pushes the nucleus to the cell periphery. The pool of mucin in a signet ring cell mimics the appearance of a finger hole and thereby gives the characteristic appearance of a signet ring cell, these tumors presented with even worse prognosis in the category of mucin secreting tumor7,8.
It is well known that MAC and SRC represent distinct clinicopathological features and molecular pathways, which may contribute them to have a more advanced stage of disease, a worse prognosis and different therapeutic response compared with adenocarcinoma8,9,10,11,12. The purpose of this study is to estimate the long-term survival benefit of adjuvant radiotherapy in RC patients with MAC and SRC.
Results
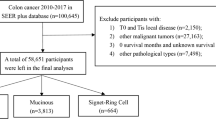
Patient characteristics
A total of 1808 eligible RC patients with MAC/SRC were collected from the Surveillance, Epidemiology, and End-Results (SEER) database during the 10-year study period, including 1607 patients with MAC and 201 patients with SRC. Of the cohort, 452 patients (25.0%) received surgery alone, and 1356 patients (75.0%) underwent surgery combined with radiotherapy. The proportion of white was 80.9%, accounting for the majority of patients collected. For patients aged <70 years, they were more likely to receive radiotherapy compared with patients aged ≥70 years. In surgery combined with radiotherapy group, 62.4% of patients were in stage III, the proportion of patients in stage III was decreased to 40.9% in surgery alone group. Furthermore, 75.7% of patients obtained sphincter preserving surgery in surgery alone group; the counterpart decreased to 66.8% for patients who underwent radiotherapy. The detailed information was listed in Table 1.
Here, we also observed the trend about different treatment strategies including surgery alone, radiation prior to surgery and radiation after surgery. The results showed that the increasing trend of radiation prior to surgery was observed as a whole from 2004 to 2013. The proportion of patients treated with radiation after surgery were gradually decreasing from 2004 to 2013 (Fig. 1). However, there was no obvious change of proportion in patients who underwent surgery alone.
Survival comparisons between surgery alone group and surgery combined with radiotherapy group.
With the aim of estimating whether RC patients with MAC/SRC could obtain survival benefit from radiotherapy, we compared 5-year and 10-year cancer specific survival (CSS) between patients receiving surgery alone and patients receiving surgery combined with radiotherapy. The results showed that 5-year CSS and 10-year CSS for patients treated with radiotherapy were 61.4% and 46.7%, which were significantly higher than patients received surgery alone (5-year CSS: 46.7%, 10-year CSS: 36.8%) (P < 0.001) (Fig. 2A). Furthermore, we separately analyzed the effects of radiotherapy on long-term survival in stage I, stage II and stage III. The results showed that patient in stage II and stage III could gain survival benefits from radiotherapy compared with patient who underwent surgery alone (Fig. 2C and D). However, there was no survival difference for patients in stage I between two groups (Fig. 2B).
To further determine the prognostic consistency between two different treatment strategies, we divided patients into 18 subgroups based on each of different demographic and clinicopathological characteristics, and Cox’s regression model was separately used to estimate hazard rate (HR) and 95% confidence interval (CI) in each subgroup (Fig. 3). The results indicated that patients who underwent radiotherapy could obtain much more survival benefits than patients treated with surgery alone. The influence of treatment strategy with respect to CSS was homogeneous in 15 subgroups with HR more than 1.0, except for patients in stage I and patient in T1/T2. Therefore, this finding sufficiently established that patients treated with radiotherapy could obtain more survival benefit than patients receiving surgery alone.
Survival comparisons following propensity score matching (PSM)
After PSM, there were totally 546 patients left, with 1:1 ratio in surgery alone group and surgery combined with radiotherapy group. The characteristics between two groups were well balance in the aspect of gender, race, TNM stage and surgical approach, with P > 0.05. All changes of characteristics after PSM were showed in Table 2. Then, the long-term survivals were compared between surgery alone group and surgery combined with radiotherapy group. The results showed that the 5-year CSS and 10-year CSS for patients who underwent surgery combined with radiotherapy were 66.4% and 54.5%, which were significantly higher than those who received surgery alone (5-year CSS: 46.2%; 10-year CSS: 33.1%) (P < 0.001) (Fig. 4A). In addition, we also compared the long-term survival in stage I, stage II and stage III, respectively (Fig. 4B–D). The results were similar to primary survival comparisons before PSM.
(A) Comparisons of CSS in patients with MAC/SRC after propensity score matching. (B) Comparisons of CSS in stage I patients with MAC/SRC after propensity score matching. (C) Comparisons of CSS in stage II patients with MAC/SRC after propensity score matching. (D) Comparisons of CSS in stage III patients with MAC/SRC after propensity score matching.
Identifying adverse prognosis factors for RC patients with MAC/SRC
To further explore the factors that influenced long-term survival of patient with MAC/SRC, univariate and multivariate Cox regression analyses were performed to determine prognostic factors (Table 3). The results suggested that receiving surgery alone was considered as independent adverse prognostic factor for CSS in RC patients with MAC/SRC. In addition, other characteristics including stage II/III, stage N1/N2 and abdominoperineal resection were all identified as independent poor prognostic factors.
Comparisons of long-term survival between patients receiving preoperative radiotherapy and patients receiving postoperative radiotherapy
With the aim of estimating the effect of therapy sequence on long-term survival, we compared the 5-year CSS and 10-year CSS between patients receiving preoperative radiotherapy and patients receiving postoperative radiotherapy. For patients in stage II and stage III, no survival differences were observed between two groups of patients (Fig. 5A and B).
Discussion
Although MAC was first described in 1923, its clinicopathological and prognostic features remains a controversial entity currently. Some series have suggested that MAC and SRC were associated with worse prognosis of colorectal cancer13,14, but others have failed to find any difference of survival outcome compared with adenocarcinoma.
The American Joint Committee considered that MAC subtype was not one prognostic factor when matched with adenocarcinoma for similar stage and grade. The National Comprehensive Cancer Network (NCCN) guideline have not attributed to mucinous histology as a risk factor that affect the therapeutic decision. In addition, current clinical practice considered them similar to the non-mucinous tumors and histology does not influence therapeutic strategy making. However, lots of studies have suggested that the differences about treatment response and survival outcome were observed between MAC/SRC and adenocarcinoma. Previous studies have shown that long-term survival outcome was better in patients with non-mucinous tumors than patients with mucinous tumors, and the histology of MAC was considered as an independent prognostic factor for prognosis in RC patients13. Mucinous tumors presented with different oncogenic and molecular pathways which may make them respond differently compared to non-mucinous tumors14.
Recently, Simha et al. found that MAC of rectum presented with a poor response to preoperative chemo-radiotherapy in the consideration of higher incidence of positive resection margin, greater residual nodal disease and larger residual tumor. Furthermore, they found that MAC had more chance of peritoneal dissemination and distant metastasis during the preoperative treatment7. Sengul et al. have found MAC was associated with a poor response to preoperative chemo-radiotherapy for RC patients with MAC. Although the short-term effect of radiotherapy for MAC and SRC were important influential factors for treatment decision making, long-term survival outcomes after radiotherapy should be paid close attention. To our best knowledge, there was no related study evaluating the efficacy of radiotherapy on long-term outcome for RC patients with mucinous tumors based on the large population. In this study, we found that the long-term survival of patients treated with radiotherapy were obviously better than patients treated with surgery alone. Although preoperative radiotherapy could effectively decreased local recurrence rate and increased sphincter preservation rate compared with postoperative radiotherapy15,16,17, no differences of long-term survival were observed between patients who underwent preoperative radiotherapy and patients who underwent postoperative radiotherapy.
Although the strengths of this study including large sample size, PSM test and subgroup analysis, many limitations should be explained. First of all, local recurrence would also be one primary endpoint in this study, but the SEER lack recurrence data, which contribute to the local control benefit of radiotherapy couldn’t be analyzed18. Secondly, the SEER has no information regarding adjuvant chemotherapy for RC patients as well as detailed information associated with treatment compliance, toxicity and histopathologic features, such as angiolymphatic invasion and margin of resection. All these factors are presented with prognostic value in RC patients19. Thirdly, the regimen of radiotherapy for RC includes two fractionation schedules: short-course and long-course radiation. However, the SEER database is short of detailed information about this regimen. We therefore could not perform further analysis with respect to the effect of short-course and long-course radiation on RC patients with MAC and SRC.
In conclusion, although MAC and SRC are distinct subtypes of RC with different biological behavior, pathological feature and treatment response compared to adenocarcinoma, RC patients with MAC/SRC could obtain more survival benefit from surgery combined with radiotherapy than surgery alone. Therefore, this finding further strengthened that this combined treatment strategy could also be considered as standard approach for RC patient with MAC and SRC.
Materials and Methods
Data source
We identified the cancer cases from the SEER database. The SEER is an openly accessed database, which covers approximately 28% of the US population20. It includes the demographic, incidence and survival data from 17 population-based cancer registries. The authors could extract cancer cases and population data from SEER database. Data in the SEER database do not require informed patient consent, because they were anonymized and de-identified prior to release.
We have got permission to acquire the research data file in the SEER program by National Cancer Institute, USA and the reference number was 10249-Nov2015. All methods were performed in accordance with the relevant guidelines and regulations of SEER database. The study design was approved by the Ethics Committee of the Second Affiliated Hospital of Harbin Medical University.
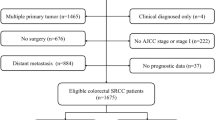
Study population
We obtained RC patients with MAC/SRC in stage I to stage III according to Site Recode classification. The collected patients were diagnosed from 2004 to 2013, because the seventh edition of AJCC TNM stage system was available in SEER database since 2004. All patients were pathologically diagnosed with the histology of MAC or SRC. The therapeutic strategies for RC patients included surgery alone and surgery combined with radiotherapy. Radiotherapy was further composed of radiotherapy prior to surgery and radiotherapy after surgery. Other clinical characteristics extracted from SEER database included age, gender, race, year of diagnosis, AJCC TNM stage, grade and surgical approaches. The surgical approaches included sphincter preserving surgery and abdominoperineal resection. The exclusion criteria were as follows: alive with no survival time and dead due to other causes.
Statistical analysis
Firstly, we evaluated the differences in patient characteristics between surgery alone group and surgery combined with radiotherapy group using the χ2 test. The CSS was estimated, which was defined as the time from the RC diagnosis until cancer recurrence or metastasis, cancer-associated death and the end of follow up. The CSS was estimated with Kaplan-Meier method, and log-rank tests were used to compare the differences of CSS curves. Univariate and multivariate Cox’s regression model were performed to estimate HR and exact 95% CIs. Furthermore, patients were classified into different subgroups based on different characteristics. These subgroup analyses of CSS were separately performed using Cox regression model to determine the prognostic consistency between surgery alone group and surgery combined with radiotherapy group. All statistical tests were two sided, P < 0.05 was considered to be statistical significance. All statistical analyses were estimated using the statistical software package SPSS 20.0 (IBM Corp, Armonk, NY, USA) and R version 2.12.0 (www.r-project.org).
PSM
A propensity 1:1 matched analysis was done to reduce possible bias to a minimum in this retrospective analysis. Propensity scores were calculated using logistic regression model for each patient in both surgery alone group and surgery combined with radiotherapy group. The covariates included in the regression were age, gender, race, AJCC TNM stage, AJCC T stage, AJCC N stage, grade and surgical approach. Patients in two groups were matched based on the propensity score. Covariates balance between two groups was examined by χ2 test. The survival comparisons were then performed for the propensity score-matched patients using the same methods as those in the primary analysis.
Additional Information
How to cite this article: Guan, X. et al. Long-term Effect of Radiotherapy in Rectal Cancer Patients with Mucinous Tumor: A Large Population Based Study. Sci. Rep. 7, 43821; doi: 10.1038/srep43821 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
van Gijn, W. et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12, 575–582 (2011).
Camma, C. et al. Preoperative radiotherapy for resectable rectal cancer: A meta-analysis. JAMA 284, 1008–1015 (2000).
Glimelius, B. Neo-adjuvant radiotherapy in rectal cancer. World J Gastroenterol 19, 8489–8501 (2013).
Allal, A. S. et al. Sphincter-sparing surgery after preoperative radiotherapy for low rectal cancers: feasibility, oncologic results and quality of life outcomes. Br J Cancer 82, 1131–1137 (2000).
Janjan, N. A. et al. Prospective trial of preoperative concomitant boost radiotherapy with continuous infusion 5-fluorouracil for locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 47, 713–718 (2000).
Sengul, N. et al. Effects of radiotherapy on different histopathological types of rectal carcinoma. Colorectal Dis 8, 283–288 (2006).
Simha, V., Kapoor, R., Gupta, R., Bahl, A. & Nada, R. Mucinous adenocarcinoma of the rectum: a poor candidate for neo-adjuvant chemoradiation? J Gastrointest Oncol 5, 276–279 (2014).
Kang, H., O’Connell, J. B., Maggard, M. A., Sack, J. & Ko, C. Y. A 10-year outcomes evaluation of mucinous and signet-ring cell carcinoma of the colon and rectum. Dis Colon Rectum 48, 1161–1168 (2005).
Naves, A. E., Mortera, M. & Biso, T. Mucinous carcinoma of the colon and rectum and its relation with adenomas. Medicina (B Aires) 45, 252–256 (1985).
Wu, C. S., Tung, S. Y., Chen, P. C. & Kuo, Y. C. Clinicopathological study of colorectal mucinous carcinoma in Taiwan: a multivariate analysis. J Gastroenterol Hepatol 11, 77–81 (1996).
Leopoldo, S. et al. Two subtypes of mucinous adenocarcinoma of the colorectum: clinicopathological and genetic features. Ann Surg Oncol 15, 1429–1439 (2008).
Safaee, A. et al. Characteristics of colorectal mucinous adenocarcinoma in Iran. Asian Pac J Cancer Prev 11, 1373–1375 (2010).
Consorti, F., Lorenzotti, A., Midiri, G. & Di Paola, M. Prognostic significance of mucinous carcinoma of colon and rectum: a prospective case-control study. J Surg Oncol 73, 70–74 (2000).
Zhang, H., Evertsson, S. & Sun, X. Clinicopathological and genetic characteristics of mucinous carcinomas in the colorectum. Int J Oncol 14, 1057–1061 (1999).
Garcia, M. et al. Phase II study of preoperative bevacizumab, capecitabine and radiotherapy for resectable locally-advanced rectal cancer. BMC Cancer 15, 59 (2015).
Radiation therapy and fluorouracil with or without semustine for the treatment of patients with surgical adjuvant adenocarcinoma of the rectum. Gastrointestinal Tumor Study Group. J Clin Oncol 10, 549–557 (1992).
Glynne-Jones, R. & Hall, M. Radiotherapy and locally advanced rectal cancer. Br J Surg 102, 1443–1445 (2015).
Guan, X. et al. Radiotherapy dose lead to a substantial prolongation of survival in patients with locally advanced rectosigmoid junction cancer: a large population based study. Oncotarget 7, 28408–28419 (2016).
Guan, X. et al. Exploration of the optimal minimum lymph node count after colon cancer resection for patients aged 80 years and older. Sci Rep 6, 38901 (2016).
Hankey, B. F., Ries, L. A. & Edwards, B. K. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev 8, 1117–1121 (1999).
Acknowledgements
The authors acknowledge the efforts of the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER database. The interpretation of these data is the sole responsibility of the authors.
Author information
Authors and Affiliations
Contributions
X.G., W.C., and X.W. designed the research; X.G., Z.J., Z.L. and G.W. performed the research; X.G., S.J., W.C., Z.J., Z.L., G.W., Y.C. and X.W. analyzed data and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Guan, X., Jia, S., Chen, W. et al. Long-term Effect of Radiotherapy in Rectal Cancer Patients with Mucinous Tumor: A Large Population Based Study. Sci Rep 7, 43821 (2017). https://doi.org/10.1038/srep43821
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43821
This article is cited by
-
The prognostic ability of radiotherapy of different colorectal cancer histological subtypes and tumor sites
Scientific Reports (2023)
-
Adjuvant Radiotherapy Is Not Necessary for Stage III Mucinous Rectal Cancer: Evidence Based on Long Survival Analysis from SEER Data
Journal of Gastrointestinal Surgery (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.