Abstract
In China, esophageal cancer has remained a large burden, and endoscopic screening is expected to reduce esophageal cancer mortality. Therefore, a population-based case-control study was conducted to evaluate the effect of screening. Cases were defined as individuals who had died of esophageal cancer, and controls were residents from the same area (three per case) who had not died of esophageal cancer, matched by gender and birth year. The exposure status (whether cases and controls had ever attended the screening or not) was acquired by inspecting the well documented screening records. A conditional logistic regression model was used to estimate the odds ratios (OR) and their 95% confidence intervals (95% CI). There were 253 cases and 759 controls. The reduction in risk of esophageal cancer mortality in individuals who had ever attended screening was 47% (OR: 0.53, 95% CI: 0.37–0.77). Compared with never-screened subjects, the ORs for screened subjects within 36 and 48 months before the reference date were 0.59(0.39–0.89) and 0.59(0.40–0.87); the ORs for 50–59 year old subjects were 0.48(0.28–0.85). The results suggest a 47% reduction in esophageal cancer mortality risk due to endoscopic screening, which may have significant implications for esophageal cancer screening in China, especially in rural areas.
Similar content being viewed by others
Introduction
There is a large regional variation in incidence of esophageal cancer worldwide. Although the incidence and mortality rates have shown a decreasing trend during the past decades in many parts of the world1,2, the incidence rate has slightly increased and the mortality rate has remained stable in China3,4. China falls within the high esophageal cancer incidence region, which is called the esophageal cancer belt5. The estimated world age-standardized incidence and mortality rates in 2012 were 12.6 per 100,000 and 10.9 per 100,000, respectively1.
Esophageal squamous cell carcinoma (SCC) is the most common esophageal cancer in Linzhou6, while adenocarcinoma is more common in Western countries, and the risk factors and natural history of these two subtypes of cancer appear to be different7,8. The development of esophageal SCC is a gradual progression from the early to the advanced stage9,10. However, because early stage esophageal cancer patients are often asymptomatic, the majority of patients in China have been diagnosed with advanced stage esophageal cancer11. The prognosis of esophageal cancer was closely related with the cancer stage. The five year survival rate for esophageal SCC was 70% for early stage patients according to the 7th edition of Cancer Staging Manual updated by the American Joint Committee on Cancer(AJCC7), while only 15% for advanced stage12. In China, the five year, ten year, and twenty year survival rates for patients discovered by screening were 86%, 75%, and 64% respectively13. Although the disease prognosis has improved over the past decades due to advances in diagnosis and treatment, esophageal cancer is still among the most lethal cancers. Cost benefit analysis was conducted in previous studies and it was found that screening, early diagnosis, and treatment for esophageal cancer could provide great cost savings in high-risk areas of China14,15,16. Early detection and diagnoses should be taken to improve esophageal cancer patients’ prognoses17.
Squamous dysplasia and carcinoma in situ have been suggested as potential targets for early detection screening because both lesions have shown high predictive power for the development of esophageal SCC in high risk populations18. Studies have also indicated that endoscopy with iodine staining and indicative biopsy can increase the sensitivity and specificity of esophageal cancer screening19,20. These findings have provided a potential tool for detecting esophageal cancer precursor lesions and for diagnosing early stage cases, especially in high risk populations21.
A national esophageal cancer screening and early treatment program has been initiated since 2005 in rural and high esophageal cancer incidence areas in China22. Linzhou city (the former Linxian County) lies in the east side of the Taihang Mountains with a population of 1.05 million and has been known worldwide for high esophageal cancer incidence. A population-based Cancer Registry had been established in Linzhou for decades; therefore, Linzhou city was selected as a pilot area to conduct the population based screening program. Endoscopy with iodine staining and indicative biopsy for residents aged 40–69 years old was used to identify precursor lesions and early cancer. By 2015, more than 30 thousand individuals aged 40–69 were screened in this project. We analyzed the data to investigate the effectiveness of the screening program in Linzhou, China.
Material and Methods
The study was approved by the Institutional Review Boards at Henan Cancer Hospital and Linzhou Cancer Hospital. All methods were carried out in accordance with the approved guidelines.
Screening Programs
The esophageal cancer screening program in Linzhou was organized and conducted by the Linzhou Cancer Hospital. Residents living in 124 villages of five towns (Hejian, Heshun, Dongyao, Hengshui and Linqi) participated in the screening program from one of the following years: 2005, 2008, 2011, 2012, or 2013. Subjects aged between 40 and 69 years old without a history of diagnosed cancer were eligible for the screening program, and about 51.2% of the target population in these villages participated in the screening program.
The endoscopic screening was carried out according to the guidelines for esophageal and gastric cancer screening, early diagnosis, and treatment program23. Written informed consent was acquired from all participants who participated in endoscopic screening according to the Declaration of Helsinki prior to the study. The participants were placed in the left lateral position, and the entire esophagus and stomach were visually examined by trained doctors. 1.2–1.5% iodine solution was used to stain the full length of the esophagus, and then unstained foci were targeted for biopsy. Biopsy specimens were fixed in 10% buffered formalin, embedded in paraffin, cut into 5-μm sections, and stained with hematoxylin and eosin. The biopsy slides were read by two pathologists. Participants were recalled to the clinic when early lesions were histologically diagnosed, and intervention methods appropriate to the lesions’ severity were used. For severe dysplasia/carcinoma in situ or intramucosal carcinomas, endoscopic mucosal resection and/or argon plasma coagulation treatments were used as local therapies. For submucosal cancers and advanced esophageal cancers, therapies included esophagectomy, radiotherapy, and other conventional treatments.
Information on participants’ demographic characteristics, life style factors, and disease history were collected using a standardized questionnaire by trained doctors in Linzhou Cancer Hospital. The individual records of participants’ information, endoscopy and pathology reports were well documented and managed by the department of cancer epidemiology of Linzhou Cancer Hospital.
Study population
All residents aged 40–69 years in these 124 villages who did not express dissent to their records being used for evaluation purposes were targeted as the study population.
Case selection
All of the 124 villages have been covered by a population-based cancer registry and the active and passive follow-up procedures have been routinely performed by the registry’s staff and village doctors in Linzhou. Cases were selected from the database of the Linzhou Cancer Registry, the data of which had been used in previous studies11,24. According to Morrison’s method25, cases were defined as individuals who had died of esophageal cancer in the 124 villages from September 2005 to December 2015. Cases were also required to meet the following criteria: 1) they must have been recorded as esophageal cancer cases during the period of September 2005 to December 2015 in the tumor registry database of the Linzhou Cancer Registry, 2) the age at diagnosis with esophageal cancer must be between 40 and 69 years old, 3) the diagnosis date must be later than the date of the screening program conducted, 4) they must have been residents in the screening area.
A total of 1609 esophageal cancer cases were identified. Among them, 710 were excluded because their ages were either less than 40 years old or over 69 years old when the screening started in their village. An additional 646 cases were excluded because the diagnosis date was earlier than the date when the screening started in their residential village. Finally, 253 cases were included in our final analysis.
Control selection
Control subjects were selected from the resident roster which was generated from the well-documented records of the resident health documents program and the New Rural Cooperative Medical Systems operated by the local government.
Deaths were excluded from the resident roster before the control selection procedure. Three controls for each case were randomly selected from the resident roster and were matched by birth year (±2 years), gender, and residence village. The controls must be alive at the death time of their matched cases. Even if the subjects were matched, individuals under 40 years of age were excluded because they had no opportunity to be screened. A “pseudodiagnosis date” was assigned to each matched control, which was the date when that control’s matched case was diagnosed with esophageal cancer. Finally, 759 control subjects were matched with the 253 case subjects.
Exposure measurement
The screening exposure was defined as those screens which took place before the date of cancer diagnosis in cases or the “pseudodiagnosis date” in controls. The dates of screening starting and ending in each village were extracted from the screening records. The status of whether cases and controls had ever attended the screenings or not was acquired by inspecting the screening records. The date of screening was also investigated, and age when screened was calculated, if they ever attended.
Statistical analysis
All statistical analysis was conducted using SAS software (SAS Institute, Cary, NC). A chi-squared test was conducted to compare the difference of each characteristic between cases and controls. The odds ratios (ORs) and their 95% confidence intervals (95% CIs) were estimated using the conditional logistic regression models. The ORs were calculated to evaluate the associations between esophageal cancer mortality and endoscopic screening. Reference dates were the diagnosis dates for case subjects or “pseudodiagnosis dates” for controls. The ORs were calculated for those who had participated in endoscopic screening within 12, 24, 36, or 48 months before the reference date when the case subjects were diagnosed with esophageal cancer, compared with individuals who had never participated in any screening. The ORs were also calculated when the screened subjects were stratified by age (40–49 years, 50–59 years, 60 years or older). Stratified analyses were also performed by gender.
Results
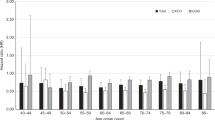
A total of 253 deceased esophageal cancer cases (156 men, 97 women) and 759 matched controls (468 men, and 291 women) were included in this study. The mean age of subjects being diagnosed with esophageal cancer was 61.8 ± 7.0 years. There were no significant differences in diagnosis age between men (61.6 ± 6.9) and women (62.1 ± 7.2). As shown in Table 1, approximately 50% of the cases were over 60 years of age. A total of 71 (28.1%) cases and 293 (38.6%) controls had ever participated in an esophageal cancer screening. Among the individuals who had ever participated in the screening, a majority of them were aged 50 years or older. The proportion of those who had participated in a screening was higher in controls than in cases for each age group.
Compared with individuals who had never participated in a screening, individuals who had ever participated in a screening program had a 47% reduced risk of dying from esophageal cancer (OR = 0.53 (0.37–0.77), Table 2). The ORs within 36 months and 48 months from the date of diagnosis were 0.59 (0.39–0.89) and 0.59 (0.40–0.87), compared with those who had never been screened before the date of diagnosis of esophageal cancer in case subjects. When examining the association by age of participating in a screening program, the ORs and 95% CI for those aged less than 50 years, 50–59 years, and 60 years or older were 1.09 (0.32–3.68), 0.48 (0.28–0.85), 0.52 (0.32–0.83) respectively.
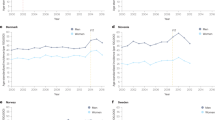
Stratified analysis by gender was shown in Table 3. The reduction in risk of esophageal cancer mortality associated with the screening program was observed to be similar for men (OR: 0.54, 95% CI: 0.35–0.86) and women (OR: 0.51, 95% CI: 0.29–0.92). When examining the association by time before reference date and age at participating screenings, a statistically significantly reduced risk of esophageal cancer mortality was only seen in men within 36 months and 48 months before reference date (OR 0.55 (95% CI: 0.32–0.93); OR 0.56 (95% CI: 0.34–0.94) and in men who were aged 50 years and over (OR (95% CI): 0.46 (0.23–0.92) for 50–59 years and 0.52 (0.29–0.95) for 60 years or older).
Discussion
Although a randomized controlled trial (RCT) is regarded as the preferred approach for evaluating cancer screening, enormous costs and huge amounts of time are required, and contamination confuses the result. Furthermore, RCT cannot be applied when screening has been widespread. The case-control study design has been regarded as an appropriate method to evaluate the efficacy of widespread cancer screening programs26. Several studies have evaluated the efficacy of screening programs for breast cancer, colorectal cancer, gastric cancer, and lung cancer27,28,29,30,31, and case control study design has been particularly effective in cervical cancer screening evaluation32. Few studies have evaluated the efficacy of an esophageal cancer screening program at population level. Our study reported a 47% reduction in risk of esophageal cancer mortality in subjects who participated in endoscopic screening compared with individuals who never participated in any screening. The result was consistent with a previous prospective study which showed a 55% reduction in risk of esophageal cancer mortality in an intervention group in which the subjects, screened by a one-time endoscopy examination, were compared with a control group33.
Endoscopy with indicative biopsy was used to screen for esophageal cancer in our study. It was also used to screen for gastric cancer in Japan and South Korea34,35,36. Case control studies had been conducted to evaluate the endoscopic screening effect for gastric cancer30. A 47% reduction in risk of esophageal cancer mortality was observed in our study; however, a smaller 30% risk reduction in gastric cancer also by endoscopic screening was found in another study30. The magnitude of the risk reduction of mortality due to endoscopy screening was lower in gastric cancer than in esophageal cancer. Although the screening in both gastric and esophageal cancer was conducted by endoscopy, esophagus screenings were considered to be more sensitive and specific because iodine staining could be used to identify precursor lesions19,20. The use of iodine staining and indicative biopsy could obviously increase the proportion of early diagnosed esophageal cancers and improve the subsequent treatment effect19,20.
When examining the association between screening time before the reference date and death from esophageal cancer, significant results were found within 36 months and 48 months before the reference date. The subjects of a case control study to evaluate the effect of cancer screening should be asymptomatic25,26. However, the symptomatic subjects could not be excluded in our study. The ORs within 12 or 24 months were higher than ORs within 36 or 48 months. The increased risk associated with screening within 12 months prior to the reference date is not surprising, and is likely to be a phenomenon of screen detection, which is related to lead time bias27,37. The results suggest that symptomatic subjects might be screened more often within 12 and 24 months before diagnosis because of their symptoms.
Endoscopic screening was found to benefit 50 years or older individuals in our study population, but found no difference between men and women. We didn’t find statistically significant association with screening in the 40–49 year old group, partly because almost 90% of the case subjects were aged 50 years or older, which was consistent with the incidence of esophageal cancer in Linzhou6.
In our study, the screening histories for cases and controls were acquired by investigating the well-documented records of the screening program. Recall bias was believed to be eliminated. However, certain limitations should also be considered when interpreting the study results.
Firstly, in studies of screening efficacy, lead-time bias occurs when the asymptomatic period in the natural history of the disease is not taken into account38. The only way to avoid lead-time bias is to compare actual mortality rates in the screened and unscreened populations38. Although a randomized controlled trial (RCT) is regarded as the preferred approach for evaluating cancer screening, enormous costs and huge amounts of time are required, and contamination confuses the result. Furthermore, the screening program in Linzhou has already been widespread for ten years, so RCT cannot be applied. Therefore, the case control study design was used to evaluate the effect for esophageal cancer screening in our study, in which case eligibility should be based on disease manifestations that develop only after lead-time intervals25. Cases were defined as deaths from esophageal cancer, which obviously meet this criterion.
Secondly, information on socioeconomic status, education, and income were not obtained in our study, which were known to be related with self-selection bias. Although Duffy et al. suggest a method correcting for non-compliance bias in case-control studies to evaluate cancer screening programs39, we could not adjust this bias due to a lack of previously published randomized data as an adjusting factor for esophageal cancer. Although, the screening program was conducted in rural areas of Linzhou, in which there was little difference in socioeconomic status between residents, and was freely provided to participants. These could reduce the possibility of selection bias, but it could not completely exclude confounding from risk factors correlated with socioeconomic factors. It’s one of the limitations in our study.
Thirdly, differences in the screening effect in subgroups were not observed due to the small number of cases. The screening program was also conducted in several other cities in Henan Province; however, these cities were not included in our study because the lag time after the screening program initiated in these cities was too short to observe the effect. Lastly, subjects who died of esophageal cancer within 2 years after the screening was initiated in the village were also included in the final analysis. There is a potential bias that this may magnify the screening effect.
To the best of our knowledge, this is the first population based case-control study to evaluate the effectiveness of endoscopic screening on the mortality of esophageal cancer. Our results suggested a 47% reduction in risk of esophageal cancer mortality by endoscopic screening with iodic staining and indicative biopsy. Although effectiveness in endoscopic screening for esophageal cancer was suggested, prudent interpretation is needed due to potential limitations, and future well-designed studies with larger sample sizes are needed to confirm our study results.
Additional Information
How to cite this article: Chen, Q. et al. Effectiveness evaluation of organized screening for esophageal cancer: a case-control study in Linzhou city, China. Sci. Rep. 6, 35707; doi: 10.1038/srep35707 (2016).
References
J, F. et al. In IARC CancerBase No. 11 Vol. 2016 (International Agency for Research on Cancer, Lyon, France, 2013).
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J Clin 65, 87–108, 10.3322/caac.21262 (2015).
Chen, W. Q. et al. [Trend analysis and projection of cancer incidence in China between 1989 and 2008]. Zhonghua Zhong Liu Za Zhi 34, 517–524, 10.3760/cma.j.issn.0253-3766.2012.07.010 (2012).
Zeng, H. M. et al. [Trend analysis of cancer mortality in China between 1989 and 2008]. Zhonghua Zhong Liu Za Zhi 34, 525–531, 10.3760/cma.j.issn.0253-3766.2012.07.011 (2012).
Wheeler, J. B. & Reed, C. E. Epidemiology of esophageal cancer. The Surgical clinics of North America 92, 1077–1087, 10.1016/j.suc.2012.07.008 (2012).
Liu, S. Z. et al. Incidence, survival and prevalence of esophageal and gastric cancer in Linzhou city from 2003 to 2009. Asian Pac J Cancer Prev 14, 6031–6034 (2013).
Zhang, H. Z., Jin, G. F. & Shen, H. B. Epidemiologic differences in esophageal cancer between Asian and Western populations. Chin J Cancer 31, 281–286, 10.5732/cjc.011.10390 (2012).
Jemal, A., Center, M. M., DeSantis, C. & Ward, E. M. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev 19, 1893–1907, 10.1158/1055-9965.EPI-10-0437 (2010).
Wang, G. Q., Wei, W. Q., Hao, C. Q., Zhang, J. H. & Lu, N. [Natural progression of early esophageal squamous cell carcinoma]. Zhonghua Zhong Liu Za Zhi 32, 600–602 (2010).
Dawsey, S. M. et al. Squamous esophageal histology and subsequent risk of squamous cell carcinoma of the esophagus. A prospective follow-up study from Linxian, China. Cancer 74, 1686–1692 (1994).
Zeng, H. et al. Cancer survival in China, 2003–2005: a population-based study. Int J Cancer 136, 1921–1930, 10.1002/ijc.29227 (2015).
Rice, T. W., Rusch, V. W., Ishwaran, H., Blackstone, E. H. & Worldwide Esophageal Cancer, C. Cancer of the esophagus and esophagogastric junction: data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union Against Cancer Cancer Staging Manuals. Cancer 116, 3763–3773, 10.1002/cncr.25146 (2010).
Wang, G. Q. et al. Long-term results of operation for 420 patients with early squamous cell esophageal carcinoma discovered by screening. Ann Thorac Surg 77, 1740–1744, 10.1016/j.athoracsur.2003.10.098 (2004).
Yang, J. et al. Estimating the costs of esophageal cancer screening, early diagnosis and treatment in three high risk areas in China. Asian Pac J Cancer Prev 12, 1245–1250 (2011).
Wei, W. Q. et al. Cost-benefit analysis of screening for esophageal and gastric cardiac cancer. Chin J Cancer 30, 213–218 (2011).
Yang, J. et al. Cost-benefit analysis of esophageal cancer endoscopic screening in high-risk areas of China. World J Gastroenterol 18, 2493–2501, 10.3748/wjg.v18.i20.2493 (2012).
Zheng, X. et al. Massive Endoscopic Screening for Esophageal and Gastric Cancers in a High-Risk Area of China. PLoS One 10, e0145097, 10.1371/journal.pone.0145097 (2015).
Wang, G. Q. et al. Histological precursors of oesophageal squamous cell carcinoma: results from a 13 year prospective follow up study in a high risk population. Gut 54, 187–192, 10.1136/gut.2004.046631 (2005).
Dawsey, S. M. et al. Squamous dysplasia and early esophageal cancer in the Linxian region of China: distinctive endoscopic lesions. Gastroenterology 105, 1333–1340 (1993).
Dawsey, S. M. et al. Mucosal iodine staining improves endoscopic visualization of squamous dysplasia and squamous cell carcinoma of the esophagus in Linxian, China. Cancer 83, 220–231 (1998).
Mansour-Ghanaei, F. et al. Endoscopic findings in a mass screening program for gastric cancer in a high risk region - Guilan province of Iran. Asian Pac J Cancer Prev 13, 1407–1412 (2012).
Bureau of Disease Prevention and Control, N. H. a. F. P. C. Cancer Early Detection and Treatment Program Report 2012/2013. Beijing, China, Bureau of Disease Prevention and Control, National Health and Family Planning Commission (2013).
Wang, G., Qiao, Y. & Wei, W. Guideline for esophageal and gastric cancer screening and early diagnose and treatment program. [In Chinese] 46–48 (People’s Medical Publishing House, 2009).
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J Clin, 10.3322/caac.21338 (2016).
Morrison, A. S. Case definition in case-control studies of the efficacy of screening. American journal of epidemiology 115, 6–8 (1982).
Cronin, K. A., Weed, D. L., Connor, R. J. & Prorok, P. C. Case-control studies of cancer screening: theory and practice. J Natl Cancer Inst 90, 498–504 (1998).
Massat, N. J., Sasieni, P. D., Parmar, D. & Duffy, S. W. An ongoing case-control study to evaluate the NHS breast screening programme. BMC cancer 13, 596, 10.1186/1471-2407-13-596 (2013).
Nakajima, M. et al. Prevention of advanced colorectal cancer by screening using the immunochemical faecal occult blood test: a case-control study. Br J Cancer 89, 23–28, 10.1038/sj.bjc.6601002 (2003).
Massat, N. J. et al. Impact of screening on breast cancer mortality: the UK programme 20 years on. Cancer Epidemiol Biomarkers Prev, 10.1158/1055-9965.EPI-15-0803 (2015).
Hamashima, C. et al. A community-based, case-control study evaluating mortality reduction from gastric cancer by endoscopic screening in Japan. PLoS One 8, e79088, 10.1371/journal.pone.0079088 (2013).
Sagawa, M. et al. A case-control study for evaluating the efficacy of mass screening program for lung cancer in Miyagi Prefecture, Japan. Cancer 92, 588–594 (2001).
Landy, R., Pesola, F., Castanon, A. & Sasieni, P. Impact of cervical screening on cervical cancer mortality: estimation using stage-specific results from a nested case-control study. Br J Cancer, 10.1038/bjc.2016.290 (2016).
Wei, W.-Q. et al. Long-Term Follow-Up of a Community Assignment, One-Time Endoscopic Screening Study of Esophageal Cancer in China. Journal of Clinical Oncology 33, 1951–1957, 10.1200/JCO.2014.58.0423 (2015).
Leung, W. K. et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol 9, 279–287, 10.1016/S1470-2045(08)70072-X (2008).
Kim, Y., Jun, J. K., Choi, K. S., Lee, H. Y. & Park, E. C. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev 12, 725–730 (2011).
Matsumoto, S., Yamasaki, K., Tsuji, K. & Shirahama, S. Results of mass endoscopic examination for gastric cancer in Kamigoto Hospital, Nagasaki Prefecture. World J Gastroenterol 13, 4316–4320 (2007).
Duffy, S. W. Case-Control Studies to Evaluate the Effect of Mammographic Service Screening on Mortality from Breast Cancer. Seminars in Breast Disease 10, 61–63, 10.1053/j.sembd.2007.09.001 (2007).
Gates, T. J. Screening for cancer: evaluating the evidence. Am Fam Physician 63, 513–522 (2001).
Duffy, S. W. et al. Correcting for non-compliance bias in case-control studies to evaluate cancer screening programmes. Journal of the Royal Statistical Society. Series C: Applied Statistics 51, 235–243, 10.1111/1467-9876.00266 (2002).
Acknowledgements
We would like to thank the Linzhou Cancer Registry for providing the data for this study and to thank all the staff in the Registry and village doctors for their work for the follow up. We are also grateful to all the staff who work for the esophageal cancer screening program. This work was supported by National Finance Transfer Payment Program of China (2006BA102A15).
Author information
Authors and Affiliations
Contributions
X.S. and Q.C. conceived the idea and designed the study. Q.C. wrote the manuscript. L.Y., C.H., J.W., S.L., M.Z., S.Z., L.G., P.Q., Y.Z. and X.S. interpreted the results and reviewed and edited the manuscript. P.G. edited the manuscript. Q.C. and X.S. had primary responsibility for final content. All authors provided intellectual input into the paper, and all authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chen, Q., Yu, L., Hao, C. et al. Effectiveness evaluation of organized screening for esophageal cancer: a case-control study in Linzhou city, China. Sci Rep 6, 35707 (2016). https://doi.org/10.1038/srep35707
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35707
This article is cited by
-
Subjective factors affecting prognosis of 469 patients with esophageal squamous cell carcinoma: a retrospective cohort study of endoscopic screening
BMC Gastroenterology (2022)
-
Global burden and epidemiology of Barrett oesophagus and oesophageal cancer
Nature Reviews Gastroenterology & Hepatology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.