Abstract
Accumulating evidence supported an association between diabetes and fibroblast growth factor 23 (FGF23). The goal of the present study was to explore alteration in serum FGF23 levels and to assess its value for identifying subclinical atherosclerosis in normoglycemic individuals with a first-degree family history of diabetes (FHD). The study enrolled 312 subjects with a first-degree FHD and 1407 subjects without an FHD. Serum FGF23 levels were detected by a sandwich enzyme-linked immunosorbent assay. Serum FGF23 levels were much higher in subjects with a first-degree FHD than in those without an FHD (P = 0.006). A first-degree FHD was positively associated with serum FGF23 levels, independent of C-IMT and cardiovascular factors (both P < 0.05). In subjects with a first-degree FHD, only those with serum FGF23 levels in the upper quartile were more likely to have an increased C-IMT (odds ratio = 2.263, P < 0.05). As conclusions, a first-degree FHD contributes to the increased serum FGF23 levels independently. Subjects with a first-degree FHD need higher serum FGF23 levels to indicate subclinical atherosclerosis. The influence of a first-degree FHD on serum FGF23 levels should be considered to avoid overestimating the risk of cardiovascular disease in normoglycemic individuals with a first-degree FHD.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is an etiologically heterogeneous disease, and its pathogenesis is strongly correlated to both genetic and environmental factors, as well as their interactions1. On the basis of genetic susceptibility, the prevalence of T2DM has increased rapidly with changes in environment and lifestyle, and then is propagated by genetic susceptibility. The lifetime risk of diabetes is 40% for first-degree relatives of patients with diabetes who have one parent with T2DM, and this risk is nearly 70% if both parents have T2DM2. A family history of diabetes (FHD) also was proposed as a significant cardiovascular risk factor by the Multi-Ethnic Study of Atherosclerosis3. Endothelial dysfunction predisposes first-degree relatives of patients with diabetes to developing atherosclerosis4. The normoglycemic individuals with a first-degree FHD are preferable for studies investigating metabolic abnormalities in the early stage of disease development, because they share the same genetic background as diabetes patients and are known to experience metabolic alterations preceding the onset of hyperglycemia5.
Fibroblast growth factor 23 (FGF23) belongs to the subfamily of endocrine fibroblast growth factors, and its physiological role is to maintain the balance of mineral metabolism6. FGF23 is believed to be a bone-derived hormone, and primary defects in bone mineralization and turnover affect FGF23 production6. Additionally, 1,25-dihydroxyvitamin D, kidney, fat mass, and adipocytokines are suggested to be systemic regulators of FGF236. Recently, a basic research study revealed that insulin action contributes to FGF23 production7, as evidenced by elevated levels of circulating FGF23 in the individuals with T2DM in most clinical studies8,9,10,11. However, some studies with small sample sizes have failed to find an association between the presence of diabetes and circulating FGF23 levels12,13. Furthermore, FGF23 is involved in the onset and progression of atherosclerosis via its effects on endothelial cell function14 and has been proposed as a predictor of cardiovascular disease (CVD) risk by prospective studies15.
Given the inconsistent findings regarding serum FGF23 levels in diabetes patients and the lack of data for serum FGF23 levels in the first-degree relatives of patients with diabetes, the present study investigated alteration in serum FGF23 levels in normoglycemic individuals with a first-degree FHD.
In addition, the carotid intima-media thickness (C-IMT) assessed by ultrasonography, which visualize the pathological characteristics of the carotid wall and lumen surfaces, is believed to be a quantitative and reproducible index to reflect the severity of systemic atherosclerosis16,17. As a non-invasive, reliable, convenient, and economical tool, carotid ultrasonography was widely used in clinical practice and epidemiological investigations18,19. Similarly, in the present study, C-IMT was applied to detection of subclinical atherosclerosis20 in order to evaluate whether serum FGF23 levels can be used to identify subclinical atherosclerosis in the first-degree relatives of patients with diabetes.
Results
Clinical characteristics of the study participants
The total study population of 1719 participants (age range: 20–78 years, median 52.82 [46.25–57.73] years) included 312 subjects with a first-degree FHD and 1407 subjects without an FHD. The proportion of women and levels of fasting plasma glucose level (FPG), glycated hemoglobin (HbA1c), fasting serum insulin (FINS), homeostasis model assessment for insulin resistance (HOMA-IR), total cholesterol (TC), and low-density lipoprotein cholesterol (LDL-c) were greater among subjects with a first-degree FHD than those without an FHD (all P < 0.05). No differences in the other variables were observed between the groups (all P > 0.05; Table 1).
Comparison of serum FGF23 levels
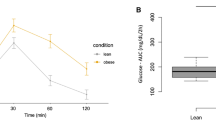
Serum FGF23 levels were much higher in subjects with a first-degree FHD than in those without an FHD (29.20 [25.00–35.99] pg/mL versus 28.30 [22.90–35.00] pg/mL, P = 0.006). The study population was divided into four subgroups on the basis of having a first-degree FHD and the measured C-IMT. The results showed whether in the presence or absence of an increased C-IMT, subjects with a first-degree FHD exhibited higher levels of serum FGF23 than those without an FHD (both P < 0.05). Additionally, among both participants with and without an FHD, serum FGF23 levels were much higher in individuals with an increased C-IMT (both P < 0.05; Fig. 1). Furthermore, serum FGF23 levels did not differ between the subjects with a first-degree FHD but without an increased C-IMT and the subjects with an increased C-IMT instead of a first-degree FHD (29.20 [24.20–35.00] pg/mL versus 30.00 [24.20–35.93] pg/mL; P = 0.977).
Comparison of serum FGF23 levels.
Subjects with a first-degree FHD have higher serum FGF23 levels than those without an FHD both in subgroup of normal and increased C-IMT (both P < 0.05). Subjects with an increased C-IMT have higher serum FGF23 levels than those with a normal C-IMT whether in presence or absence of a first-degree FHD (both P < 0.05).
Relationship between a first-degree FHD and the serum FGF23 levels
Logistic regression analysis revealed an independent and positive relationship between a first-degree FHD and the serum FGF23 levels (odds ratio [OR] = 1.023, P = 0.001). After adjustment for gender, age, and estimated glomerular filtration rate (eGFR), the positive association between the first-degree FHD and the serum FGF23 levels remained significantly (OR = 1.025, P = 0.001). Furthermore, this relationship remained significant after additional adjustment for C-IMT and cardiovascular risk factors (OR = 1.024, P = 0.001 and OR = 1.022, P = 0.003, respectively; Table 2).
Logistic regression analysis of the presence of an increased C-IMT
Defining the presence of an increased C-IMT as a dependent variable, logistic regression analysis showed that the OR for an increased C-IMT increased with increasing serum FGF23 levels both in subjects with and without an FHD (both P < 0.05). The FGF23 quartiles were defined according to the median and interquartile values of serum FGF23 levels for the entire study population, as follows: quartile 1: ≤ 23.80 pg/mL; quartile 2: 23.81–29.19 pg/mL; quartile 3: 29.20–34.99 pg/mL; and quartile 4: ≥ 35.00 pg/mL. In those without an FHD, individuals with serum FGF23 levels in quartiles 3 and 4 were more likely to have an increased C-IMT (OR = 1.415 and 1.439, respectively, both P < 0.05). Among subjects with a first-degree FHD, only those with serum FGF23 levels in quartile 4 showed a significantly increased OR for an increased C-IMT (OR = 2.263, P < 0.05; Table 3).
Discussion
In the present study, individuals with a first-degree FHD exhibited elevated serum FGF23 levels no matter in the presence or absence of an increased C-IMT, and a first-degree FHD was positively associated with the serum FGF23 levels independent of the C-IMT and other cardiovascular risk factors. For individuals with a first-degree FHD, higher serum FGF23 levels were necessary to indicate the presence of an increased C-IMT.
A previous multicenter study in the USA8 involving 3756 participants with mild to moderate chronic kidney disease (CKD) reported that diabetes patients had higher serum FGF23 levels and experienced an earlier onset of FGF23 excess. After adjustment for demographic, clinical, and laboratory variables, diabetes remained a significant factor associated with serum FGF23 levels in their study. Their findings also held true for study participants with an eGFR >60 mL/min/1.73 m2. Another study conducted in population with CKD stages 2–4 provided evidence for a positive association between the presence of diabetes and serum FGF23 levels9. Similarly, Schoppet et al.10 reported the association of diabetes with elevated serum FGF23 levels in healthy older men (>60 years). A community-based study proposed that an elevated FGF23 concentration is a subclinical marker of metabolic perturbations (diabetes, dyslipidemia, and obesity) in individuals with normal kidney function11. Therefore, the population included in the present study was restricted to those with normal glucose tolerance to eliminate the effects of hyperglycemia.
Winther et al.12 performed a euglycemic-hyperinsulinemic clamp in a small study population consisting of obese individuals with T2DM, glucose-tolerant obese healthy individuals, and lean individuals. Only in diabetes subjects did they observe a significant increase in serum FGF23 levels after clamp, which was correlated with the increase in insulin levels. Mirza et al.21 found that a 1-standard deviation increase in log FGF23 was associated with 8–12% increases in insulin levels and HOMA index values in two independent cohorts of elderly individuals. These findings suggested that hyperinsulinemia and insulin resistance might contribute to the increase in serum FGF23 levels in diabetes population.
The first-degree relatives of patients with diabetes are considered to have an increased risk of diabetes, and they often exhibit hyperinsulinemia even in absence of obesity5. Stadler et al.22 conducted 75 g oral glucose tolerance test and hyperinsulinaemic–isoglycaemic clamps on 706 participants without diabetes. Their findings indicated the presence of insulin resistance and β cell dysfunction in the individuals with a first-degree FHD. Another prospective cohort study23 of non-diabetes individuals with a first-degree FHD also demonstrated that, genetically predisposed for diabetes, individuals with deteriorating glucose tolerance exhibited insulin resistance and β cell dysfunction. Contrary to the great amount of evidence supporting the impaired insulin activity in the individuals with a first-degree FHD, no previous studies have reported the variation in serum FGF23 levels in this population. The present study revealed a significant increase in serum FGF23 levels in normoglycemic individuals with a first-degree FHD, accompanied by increases in serum insulin levels and HOMA-IR values, and these findings are consistent with those of most studies of diabetes populations. Based on these results, the heritability of diabetes could be responsible for the elevation in serum FGF23 levels, even when blood glucose levels are in the normal range. The abnormality of insulin action may be an explanatory factor for the alteration in serum FGF23 levels in the first-degree relatives of patients with diabetes.
Clinical studies have revealed that endothelium-dependent vasodilation decreases by 38%4, whereas the C-IMT increases by 18% in first-degree relatives of patients with diabetes24. Moreover, first-degree relatives of patients with diabetes were found to be more likely to develop atherosclerotic CVD25. Therefore, early assessment of CVD risk is particularly important for individuals with a first-degree FHD to prevent the onset and progression of CVD. A prospective study proposed that the serum FGF23 levels can predict major cardiovascular events in the community population, even in consideration of the established cardiovascular risk factors, mineral metabolism abnormalities, and subclinical cardiovascular damage15. An increased C-IMT represents an intermediate phenotype for early-stage atherosclerosis. Due to its association with various cardiovascular risk factors and its predictive value for CVD-related death, the C-IMT serves as a reliable index applied to detecting and monitoring atherosclerosis clinically20. By using the C-IMT to represent subclinical atherosclerosis, as well as evaluate the CVD risk, the present study found that an elevated serum FGF23 levels could indicate the presence of subclinical atherosclerosis in normoglycemic individuals with a first-degree FHD.
Notably, the relationship between the presence of diabetes and altered serum FGF23 levels was reported to be independent of cardiovascular risk factors in previous studies9. Consistently, the present study found that first-degree relatives of patients with diabetes exhibited higher levels of serum FGF23 at an equivalent degree of subclinical atherosclerosis as assessed by the C-IMT. The association of a first-degree FHD with an elevated serum FGF23 levels was independent of the C-IMT and other cardiovascular factors. For individuals with a first-degree FHD, additionally, the serum FGF23 levels increased even in absence of an increased C-IMT, reaching the same levels observed in participants with an increased C-IMT and without an FHD. Compared to those without an FHD, participants with a first-degree FHD need higher levels of serum FGF23 to indicate the subclinical atherosclerosis. Thus, the influence of a first-degree FHD on the serum FGF23 levels should be taken into consideration in the clinical setting. If not, the use of serum FGF23 as a biomarker in first-degree relatives of patients with diabetes may result in overestimation of the CVD risk.
Although the relationship between the presence of a first-degree FHD and serum FGF23 levels was demonstrated in the present study, the potential mechanism for the findings remains unclear. Insulin activation induces stimulation of Akt/PKB and serum- and glucocorticoid-inducible kinase isoforms, further resulting in the inhibition of glycogen synthase kinase (GSK)-3. Experiments in transgenic mice revealed that GSK3 was involved in the regulation of FGF23 release via the promotion of sympathetic nervous system activity7. Therefore, it is possible that serum FGF23 levels increase upon alteration of insulin activity in individuals with a first-degree FHD. Moreover, human studies on diabetes population provided evidence supporting the contribution of insulin resistance to the alteration in microarchitecture, osteoblast differentiation, and bone turnover, which consequently results in the poorer quality of the skeleton26. Although the current animal models of T2DM are limited by their ability to recapitulate the impact of diabetes on bone metabolism, the data available are largely consistent with those obtained in human studies27, suggesting that insulin-induced bone impairment may play a role in the elevated serum FGF23 levels in the first-degree relatives of patients with diabetes.
The cross-sectional design of this study limited the ability to assess the directionality of the association between elevated serum FGF23 levels and an increased C-IMT. A further prospective study is needed to evaluate the predictive value of serum FGF23 levels for the CVD risk in first-degree relatives of patients.
In conclusions, a first-degree FHD contributes to an increase in serum FGF23 levels, independent of the presence of subclinical atherosclerosis and cardiovascular factors. In individuals with a first-degree FHD, serum FGF23 levels need to be higher to indicate the presence of subclinical atherosclerosis. For use of serum FGF23 levels in the clinical evaluation of first-degree relatives of patients with diabetes, the influence of a first-degree FHD should be considered to avoid overestimation of the CVD risk in this population.
Methods
Subjects
The study population comprised a subgroup of participants with normal kidney function (eGFR ≥ 60 mL/min/1.73 m2) of the Shanghai Obesity Study28. Based on the 1999 World Health Organization criteria29, individuals displaying impaired glucose regulation or diabetes were excluded. Individuals with the following conditions also were excluded: established cardiovascular and cerebrovascular disease, carotid plaque, hepatic dysfunction, hyperthyroidism or hypothyroidism, hypercalcemia, acute infection, tumors, psychiatric disease, current lipid-lowering therapy, and current replacement therapy with systemic corticosteroids or thyroxine. The participants provided complete clinical data and finished a standardized questionnaire to gather information on their disease history, medication usage, family history, and smoking status. A first-degree FHD was defined as having one or more first-degree relatives of patients with diabetes (parent, sibling, or offspring)30.
The study was carried out in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. All participants provided written informed consent prior to participation to the study.
Anthropometric and biochemical assessments
All participants were examined after an overnight fast lasting at least 10 hours. Anthropometric assessments included height, weight, waist circumference (W), and resting blood pressure. Body mass index (BMI) was calculated as follows: BMI = weight (kg)/height2 (m2). Biochemical variables were detected according to methods previously reported28, including: FPG, 2-hour plasma glucose (2 hPG; determined after a 75 g oral glucose tolerance test), HbA1c, FINS, TC, triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), LDL-c, C-reactive protein (CRP), serum creatinine (Scr), and serum calcium (Ca) levels. A Kainos sandwich enzyme-linked immunosorbent assay kit (Kainos Laboratories Inc., Tokyo, Japan) was used to detect serum FGF23 levels. The intra- and inter-assay coefficients of variations were 5.6% and 8.2%, respectively. Insulin resistance was assessed using the insulin resistance index (HOMA-IR), calculated as previously described28. The eGFR was calculated according to the Chronic Kidney Disease Epidemiology Collaboration equation31: eGFR = [141 × min (Scr (mg/dL)/k, 1)α × max (Scr/k, 1)−1.209 × 0.993age × 1.018 (if women)]; where k is 0.7 for women and 0.9 for men, and α is −0.329 for women and −0.411 for men.
Carotid ultrasonography
A single trained sonographer unaware of the study design scanned the carotid arteries using a Voluson 730 Expert B-mode ultrasonogram equipped with a 10-MHz probe (GE Healthcare). The right and left common carotid arteries were scanned from the proximal to the distal position, to the point of bifurcation. At the far wall of the right and left common carotid arteries, approximately 1 cm proximal to the carotid bulb, C-IMT was shown by two parallel lines that delineate the leading edges of the lumen-intima and media-adventitia interfaces. The mean value of the maximal thickness of each carotid artery was calculated to determine the C-IMT, as previously described32. C-IMT values above the 75th percentile cutoff point for the study population (≥0.65 mm) were considered increased33.
Cardiovascular risk factors
The Framingham risk score was recommended by Adult Treatment Panel III as a standard risk assessment of CVD risk34. The indexes (gender, age, systolic blood pressure [SBP], LDL-c, HDL-c, and smoking status) used to generate the Framingham risk score were considered as the cardiovascular risk factors in the present study34.
Statistical analysis
All statistical analyses were carried out with the SPSS 16.0 statistical software package (SPSS Inc., Chicago, IL, USA). The normality of data distribution was determined by the one-sample Kolmogorov-Smirnov test. Continuous variables are expressed as mean ± standard deviation or median with interquartile range. Categorical variables are expressed as number with percent. Comparisons between the two groups were conducted with the unpaired Student’s t-test, Mann-Whitney U-test and Chi-squared test for continuous data with a normal distribution, continuous data with a skewed distribution, and categorical variables, respectively. Multivariate logistic regression models were established to analyze the associations of a first-degree FHD with serum FGF23 levels and the OR of an increased C-IMT across serum FGF23 quartiles. All reported P values were two-tailed, and P < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Hu, X. et al. Elevation in fibroblast growth factor 23 and its value for identifying subclinical atherosclerosis in first-degree relatives of patients with diabetes. Sci. Rep. 6, 34696; doi: 10.1038/srep34696 (2016).
References
Alberti, G. et al. Type 2 diabetes in the young: the evolving epidemic: the international diabetes federation consensus workshop. Diabetes Care. 27, 1798–1811 (2004).
Stančáková, A. & Laakso, M. Genetics of Type 2 Diabetes. Endocr. Dev. 31, 203–220 (2016).
Scheuner, M. T., Setodji, C. M., Pankow, J. S., Blumenthal, R. S. & Keeler, E. Relation of familial patterns of coronary heart disease, stroke, and diabetes to subclinical atherosclerosis: the multi-ethnic study of atherosclerosis. Genet. Med. 10, 879–887 (2008).
Goldfine, A. B. et al. Family history of diabetes is a major determinant of endothelial function. J. Am. Coll. Cardiol. 47, 2456–2461 (2006).
Ishikawa, M., Pruneda, M. L., Adams-Huet, B. & Raskin, P. Obesity-independent hyperinsulinemia in nondiabetic first-degree relatives of individuals with type 2 diabetes. Diabetes. 47, 788–792 (1998).
Martin, A., David, V. & Quarles, L. D. Regulation and function of the FGF23/klotho endocrine pathways. Physiol. Rev. 92, 131–155 (2012).
Fajol, A., Chen, H., Umbach, A. T., Quarles, L. D., Lang, F. & Föller, M. Enhanced FGF23 production in mice expressing PI3K-insensitive GSK3 is normalized by β-blocker treatment. FASEB. J. 30, 994–1001 (2016).
Wahl, P. et al. Earlier onset and greater severity of disordered mineral metabolism in diabetic patients with chronic kidney disease. Diabetes Care. 35, 994–1001 (2012).
Vervloet, M. G. et al. Fibroblast growth factor 23 is associated with proteinuria and smoking in chronic kidney disease: an analysis of the MASTERPLAN cohort. BMC. Nephrol. 13, 20 (2012).
Schoppet, M. et al. Serum level of the phosphaturic factor FGF23 is associated with abdominal aortic calcification in men: the STRAMBO study. J. Clin. Endocrinol. Metab. 97, E575–E583 (2012).
Hanks, L. J., Casazza, K., Judd, S. E., Jenny, N. & Gutiérrez, O. M. Associations of fibroblast growth factor-23 with markers of inflammation, insulin resistance and obesity in adults. PLoS. One. 10, e0122885 (2015).
Winther, K., Nybo, M., Vind, B., Pedersen, S. M., Højlund, K. & Rasmussen, L. M. Acute hyperinsulinemia is followed by increased serum concentrations of fibroblast growth factor 23 in type 2 diabetes patients. Scand. J. Clin. Lab. Invest. 72, 108–113 (2012).
Reyes-Garcia, R., Garcia-Martín, A., García-Fontana, B., Morales-Santana, S., Rozas-Moreno, P. & Muñoz-Torres, M. F. FGF23 in Type 2 Diabetic Patients: Relationship With Bone Metabolism and Vascular Disease. Diabetes Care. 37, e89–e90 (2014).
Silswal, N. et al. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am. J. Physiol. Endocrinol. Metab. 307, E426–E436 (2014).
Ärnlöv, J. et al. Serum FGF23 and risk of cardiovascular events in relation to mineral metabolism and cardiovascular pathology. Clin. J. Am. Soc. Nephrol. 8, 781–786 (2013).
Greenland, P. et al. Prevention Conference V: Beyond secondary prevention: identifying the high-risk patient for primary prevention: noninvasive tests of atherosclerotic burden: Writing Group III. Circulation. 101, E16–E22 (2000).
Pignoli, P., Tremoli, E., Poli, A., Oreste, P. & Paoletti, R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 74, 1399–1406 (1986).
Zheng, T. P., Liu, Y. H., Yang, L. X., Qin, S. H. & Liu, H. B. Increased plasma dipeptidyl peptidase-4 activities are associated with high prevalence of subclinical atherosclerosis in Chinese patients with newly diagnosed type 2 diabetes: a cross-sectional study. Atherosclerosis. 242, 580–588 (2015).
Dalmas. E. et al. Intima-media thickness in severe obesity: links with BMI and metabolic status but not with systemic or adipose tissue inflammation. Diabetes Care. 36, 3793–3802 (2013).
Zhang, F., Feng, L., Chen, Y., Geng, Z. & Xu, X. Relationship between carotid artery intima-media thickness and cardiovascular risk factors in Chinese Uygur population. Int. J. Clin. Exp. Med. 7, 5412–5420 (2014).
Mirza, M. A. et al. Circulating Fibroblast Growth Factor-23 Is Associated With Fat Mass and Dyslipidemia in Two Independent Cohorts of Elderly Individuals. Arterioscler. Thromb. Vasc. Biol. 31, 219–227 (2011).
Stadler, M., Pacini, G., Petrie, J., Luger, A. & Anderwald, C. RISC Investigators. Beta cell (dys)function in non-diabetic offspring of diabetic patients. Diabetologia. 52, 2435–2444 (2009).
Henninger, J., Hammarstedt, A., Rawshani, A. & Eliasson, B. Metabolic predictors of impaired glucose tolerance and type 2 diabetes in a predisposed population - A prospective cohort study. BMC Endocr. Disord. 25, 15–51 (2015).
Anderwald, C. et al. Glucose turnover and intima media thickness of internal carotid artery in type 2 diabetes offspring. Eur. J. Clin. Invest. 38, 227–237 (2008).
Park, J. W. et al. Family history of diabetes and risk of atherosclerotic cardiovascular disease in Korean men and women. Atherosclerosis. 197, 224–231 (2008).
Carnevale, V., Romagnoli, E., D’Erasmo, L. & D’Erasmo, E. Bone damage in type 2 diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 24, 1151–1157 (2014).
Fajardo, R. J., Karim, L., Calley, V. I. & Bouxsein, M. L. A review of rodent models of type 2 diabetic skeletal fragility. J. Bone. Miner. Res. 29, 1025–1040 (2014).
Bao, Y. et al. Inverse relationship between serum osteocalcin levels and visceral fat area in Chinese men. J. Clin. Endocrinol. Metab. 98, 345–351 (2013).
World Health Organization. Department of Noncommunicable Disease Surveillance. Definition, diagnosis and classification of diabetes mellitus and its complication. Report of a WHO consultation. Part 1: Diagnosis and classification of diabetes mellitus. World Health Organization, Geneva (1999).
Cederberg, H., Stančáková, A., Kuusisto, J., Laakso, M. & Smith, U. Family history of type 2 diabetes increases the risk of both obesity and its complications: is type 2 diabetes a disease of inappropriate lipid storage? J. Intern. Med. 277, 540–551 (2015).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Wang, Y. et al. Contribution of visceral fat accumulation to carotid intima-media thickness in a Chinese population. Int. J. Obes. (Lond). 36, 1203–1208 (2012).
Huang, Y. et al. Glycated hemoglobin A1c, fasting plasma glucose, and two-hour postchallenge plasma glucose levels in relation to carotid intima-media thickness in Chinese with normal glucose tolerance. J. Clin. Endocrinol. Metab. 96, E1461–E1465 (2011).
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 106, 3143–3421 (2002).
Acknowledgements
This work was funded by 973 Program of China (2013CB530606), Grant from Shanghai Health and Family Planning Commission (2013ZYJB1001), Project of National Natural Science Foundation of China (81100563), and Translational Medicine Innovation Foundation of School of Medicine Shanghai Jiao Tong University (15ZH2010 and 15ZH4006).
Author information
Authors and Affiliations
Contributions
Y.B. and W.J. designed the study. X.M., X.H., Y.L., Y.X. and Q.X. collected the data. X.H. performed statistical analysis and wrote the paper. X.P. performed the FGF23 measurements. Y.B., X.M., X.H. and W.J. revised the paper and contributed to discussion. X.H. was the guarantor.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hu, X., Ma, X., Luo, Y. et al. Elevation in fibroblast growth factor 23 and its value for identifying subclinical atherosclerosis in first-degree relatives of patients with diabetes. Sci Rep 6, 34696 (2016). https://doi.org/10.1038/srep34696
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep34696
This article is cited by
-
Elevated serum fibroblast growth factor 23 levels as an indicator of lower extremity atherosclerotic disease in Chinese patients with type 2 diabetes mellitus
Cardiovascular Diabetology (2017)
-
The production of fibroblast growth factor 23 is controlled by TGF-β2
Scientific Reports (2017)
-
The Role and Potential Therapeutic Implications of the Fibroblast Growth Factors in Energy Balance and Type 2 Diabetes
Current Diabetes Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.