Abstract
Allergic conjunctivitis is a common problem that significantly impairs patients’ quality of life. Whether air pollution serves as a risk factor for the development of allergic conjunctivitis remains elusive. In this paper, we assess the relationship between air pollutants and weather conditions with outpatient visits for allergic conjunctivitis. By using a time-series analysis based on the largest dataset ever assembled to date, we found that the number of outpatient visits for allergic conjunctivitis was significantly correlated with the levels of NO2, O3 and temperature, while its association with humidity was statistically marginal. No associations between PM10, PM2.5, SO2, or wind velocity and outpatient visits were seen. Subgroup analyses showed that sex seemed to modify the effects of humidity on outpatient visits for allergic conjunctivitis, but not for NO2, O3, or temperature. People younger than 40 were found to be susceptible to changes of all four parameters, while those older than 40 were only consistently affected by NO2 levels. Our findings revealed that higher levels of ambient NO2, O3 and temperature increase the chances of outpatient visits for allergic conjunctivitis. Ambient air pollution and weather changes may contribute to the worsening of allergic conjunctivitis.
Similar content being viewed by others
Introduction
With the rapid industrialization and urbanization, air quality problems and other environmental health troubles are particularly becoming major sources of morbidity and mortality in human1. Allergic conjunctivitis is one of the most common ocular surface diseases; it damages the ocular surface and causes debilitating symptoms of redness and itching, resulting in impaired quality of life for patients and limited physical activity2. More importantly, allergic conjunctivitis affects up to 40 percent of the population of the United States3.
Pollen, animal dander and other environmental antigens are the main causes of allergic conjunctivitis, yet a recent (2014) hospital-based study showed that exposure to ambient air pollution—especially particulate air pollution—possibly increases the risk of allergic conjunctivitis4. The effects of exposure to other well-defined pollutants such as ozone (O3), sulfur dioxide (SO2) and nitrogen dioxide (NO2) on this disease remain inconclusive. Although several studies have evaluated this issue, with limited success4,5, we still lack a long-term study with a large sample size to make statistically significant statements. Furthermore, human health is being adversely affected by climate change6. This change in weather patterns has been proven to affect the timing, distribution, quantity and quality of aeroallergens and has changed the distribution and severity of asthma and allergic disease7; its role in the development of allergic conjunctivitis, however, remains unknown.
The effect of ambient air pollution and weather pattern changes on allergic conjunctivitis may differ from asthma and other allergic diseases due to anatomical differences between the eyes and lungs. For example, unlike the lungs, where air pollutants tend to penetrate deeply and stay, the cleansing system of the ocular surface (i.e. tears) may be capable of alleviating the cellular damage induced by air pollutants. On the other hand, the ocular surface is directly exposed to the environment, which means that it may be more susceptible to weather changes.
Taken together, we hypothesize that ambient air pollution as well as weather changes, are both associated with risk for allergic conjunctivitis. To address this issue, population-wide data is crucial. The current study exemplifies a unique situation whereby population-wide outpatient attendance for allergic conjunctivitis in Shanghai was recorded systemically from 2008 to 2012, as well as the information on ambient air pollutants and weather conditions. The availability of such a large dataset allowed us to assess the effects of ambient air pollutants and weather conditions on the prevalence of allergic conjunctivitis with statistical rigor.
Results
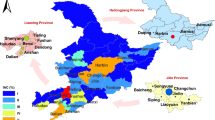
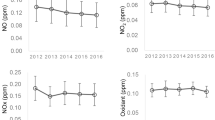
The current study included 3,211,820 outpatient visits by 15,938,870 subjects enrolled in SHIS for allergic conjunctivitis. Table 1 and Fig. 1 show the baseline characteristics and the number of outpatient visits for the five-year period. More than three million outpatient visits occurred during the time period examined. The mean age of the patients’ onset was 54 years and 62 percent were women; the number of outpatient visits was highest in people older than 60 years (Fig. 2). Table 2 lists the concentration of air pollutants and weather conditions, while Figs 3 and 4 further demonstrate the changes in these parameters with time.
We decided to convert the outpatient visits from a daily to a weekly measure, as we noticed that the outpatient visits showed strong periodicity by week due to the working hours of the local population. After the conversion, the average weekly outpatient visits ranged from 423 to 2,927 per week (Fig. 5). Although the outpatient visits may be mostly described as a Poisson event, the large mean of the weekly visit can be approximated by a Gaussian distribution (Supplemental file 1).
The outpatient visits for allergic conjunctivitis were significantly correlated with the levels of NO2, O3 and temperature (Table 3). Among the pollutants we evaluated, every 10 μg/m3 increased exposure to NO2 resulted in 61 more outpatient visits per week, whereas 10 μg/m3 higher O3 exposure increased the weekly outpatient visits by 21 per week. As for the weather conditions, temperature was the only factor that was significantly associated with outpatient visits. The association between outpatient visits and humidity was statistically marginal. In spite of these factors, our results show no significant association for PM10 (particles smaller than 10 μm in aerodynamic diameter), PM2.5 (particles smaller than 2.5 μm in aerodynamic diameter), SO2, or wind velocity.
In order to further investigate the interactions among the pollutants and weather conditions, we tested the interactions between each pollutant and the weather condition and filtered the interactive factors using the stepwise method (Supplemental file 2). As a result, we found significant interactive effects from NO2 and humidity, which suggests that changes in the weather may also affect outpatient visits. Table 4 shows that a one-unit increment in exposure to NO2, O3, temperature and humidity elevated the number of outpatient visits from different subgroups. Subgroup analyses showed that humidity—but not NO2, O3, or temperature—influenced the number of outpatient visits for allergic conjunctivitis, in a sex-dependent manner. People younger than 40 years showed susceptibility to changes in all four parameters, while those older than 40 were only consistently correlated with NO2. When the data were stratified according to season, the number of outpatient visits for allergic conjunctivitis was more frequent in the spring and summer than in the winter (Fig. 6 and Table 5). Sex and age did not modify this effect.
Discussion
During the earliest period of China’s economic reforms, lasting from the late 1970 s to 1985, automobiles were scarce and energy consumption was quite low, which greatly limited emissions of ambient air pollutants and greenhouse gases8. From 1985 to 2008, however, the Chinese economy expanded rapidly. Although economic growth associated with industrialization has improved health and various quality of life indicators, environmental issues associated with this process are of increasing concern to the country’s citizens and its government. Our study has demonstrated the relationship between allergic conjunctivitis and air pollution and weather changes. We showed that the number of outpatient visits with allergic conjunctivitis increased as the levels of NO2, O3, temperature and humidity changed.
Currently, there are controversies around the association between respiratory allergic disorders and outdoor NO2 levels. Hwang et al. found that long-term exposure to outdoor NO2 increased the subjects’ risks of persistent cough and phlegm, as well as “current asthma” (i.e. people who confirm that they have been told by a health practitioner that they have asthma and who confirm that they still have it)9,10. Another earlier study, however, reported that the risk of childhood asthma was not associated with levels of NO2 among 32,672 Taiwanese schoolchildren11. Information on the association of air pollution with the prevalence of allergic conjunctivitis is limited. Chang et al. reported that the air pollutants NO2, SO2, O3 and fine particulate matter can increase the chances of outpatient visits for nonspecific conjunctivitis5. Riediker et al. found that the rhinoconjunctival tissue is sensitive to irritant stimuli during an ongoing allergic inflammation and that symptoms of allergic rhinoconjunctivitis might be exacerbated in areas with increased levels of air pollutants12. A Japanese hospital-based study also showed that outpatient visits for allergic conjunctivitis had a positive association with air pollutants during a three-month investigation period, although such associations were not statistically significant4. Interestingly, among several air pollutants investigated in our study, NO2 and O3 were the only potent triggers for allergic conjunctivitis exacerbation.
The mechanisms underlying the effects of air pollutants on allergic conjunctivitis are not well understood. The study by Lin et al. showed that PM10 significantly affects the respiratory system13. In the present study, however, no association was found for PM10 with allergic conjunctivitis. We assume that PM10 and PM2.5 do not cause a change in pH (as do other aerosol pollutants after they reach the ocular surface) because they can be cleared out of the ocular surface by the cleansing system of tears14, whereas in the respiratory system, fine particulate matter penetrates deeply and stays in the lungs. Furthermore, changes in the lacrimal pH—caused by the acidification of tears exposed to a high-oxidant concentration (NO2 and SO2)—could irritate the ocular surface15,16. NO2 and O3 pose high oxidative potential and are able to cause damage to the human nasal mucosa17; the effects are also apparent in ocular mucosa18,19. NO2 and O3 thus may have a higher capacity to provoke conjunctival inflammation than SO2 via direct oxidative damage to the ocular surface and acidification of the tears in patients with allergic conjunctivitis. In addition, diesel exhaust pollutants, including NO2 and O3, have been reported to enhance the allergic sensitization20. Furthermore, NO2 and O3 may induce conjunctival inflammation indirectly via chemical modifications of aeroallergens and subsequent enhanced allergic response.
Human health will likely be adversely affected by accelerating changes in weather patterns7. Particularly, allergic diseases may be induced and worsened by weather conditions, because of changes in the type, quantity, distribution and exposure time of pollens and because of the interaction between pollens and air pollutants7. In the present study, the frequency of outpatient attendance of allergic conjunctivitis was inversely correlated with the humidity and positively correlated with temperature. The correlation between temperature change and pollen distribution has been well described in the literature. Theoretically, increased temperature stimulates earlier flowering and longer pollen seasons2. Results have indicated that if temperature increases under a doubled greenhouse gases scenario by the end of the twenty-first century, pollination seasons will start on average one month earlier and airborne pollen concentrations will be 50 percent higher than they are today21. Meanwhile, low humidity increases land surface evaporation, thus resulting in an increase in airborne pollen concentrations22. Pollen sensitivities were indicated as the most frequent triggers for allergic conjunctivitis23. Mimura et al. reported that Cedar pollen-specific IgE were significantly higher in tears of allergic conjunctivitis patients than in control subjects24. These weather pattern changes, in combination with air pollution, will further add to the burden of allergic disease in exposed populations. For patients with allergic conjunctivitis, the results of our study mean that both air quality and weather conditions play important roles in minimizing exposure and symptoms.
Our study also reported the time-lag effect of air pollutants and weather pattern changes on outpatient visits for allergic conjunctivitis. The finding that outpatient visits reached their highest level after three weeks of exposure to pollutants might be of assistance to the public health systems, so that they may better monitor and prepare for environmental events. In addition, the selective and delayed response in patients implies a certain regulatory mechanism that is still not fully understood.
In summary, our study found that higher levels of ambient NO2, O3 and temperature and lower humidity lead to an increased chance of outpatient visits for allergic conjunctivitis. Our study indicates that ocular surface health may be impaired by long-term exposure to air pollution. These results suggest that efforts to control emissions of both air pollutants and greenhouse gases are warranted. The relationship of these environmental factors to ocular surface health underscores the importance of having all members of the health care team—including health policy decision-makers, specialists and primary care providers—send the same message to all patients about the necessity of controlling the exposure of the ocular surface to air pollution and adverse weather conditions, as this should help to prevent the onset of allergic conjunctivitis and should minimize the symptoms and signs in patients who already suffer from the condition.
Strengths and limitations of the study
While our findings are strengthened by the use of a representative, large-population, registry sample, the present study does have several limitations. First, data on pollen and microbial exposure are not available in our study, which are important outdoor environmental factors associated with allergic conjunctivitis25. One may suspect that the overlap time between the concentration of air pollutants and allergens, such as pollens, could bias our findings. Our data, however, did not support this possibility. For example, NO2 concentration peaks in winter while pollens are more in spring and summer (Fig. 4). Our findings showed that NO2 and O3 are independent risk factors that add to the risk posed by the pollens. Second, one may raise the concern about using ambient air pollutant concentrations as exposure surrogates, because people spend more time indoors. However, measurements of indoor air pollutants have a large inter-subject variability. In addition, it seems that the infiltration of ambient pollutants to indoor environments occurs under a high ambient fine particle pollution condition26. Real-time ventilation measurements for indoor air pollution are recommended to address this issue. Third, as a registry study, we were not able to take the geographic mobility of the population into account during the follow-up period. Fourth, the SHIS is not solely designated for evaluating the prevalence or clinical characteristics of allergic conjunctivitis. As a result, body mass indexes, sociodemographic situations, education levels and systemic health conditions were not available for further analysis. This is an inherent limitation of studies that use a pre-existing database. Finally, although we could use the patient’s specific diagnostic codes, uncertainties were unavoidable because the exact diagnosis of each case could not be confirmed without individuals’ medical records.
Methods
Allergic Conjunctivitis Data
Data on outpatient visits between January 1, 2008 and December 31, 2012 were obtained from the database of the Shanghai Health Insurance System (SHIS). More than 96 percent of Shanghai’s residents—15.9 million—receive SHIS’s compulsory universal health insurance. All hospitals in Shanghai are required to contract with the SHIS and submit standard claim documents for medical expenses on a computerized form that includes the date of visit and discharge, identification number, sex, birthday and the diagnosis for each patient. Outpatient visits for allergic conjunctivitis were selected in the current study according to the diagnosis codes of the International Classification of Diseases, ninth revision (ICD-9). The following codes were included: 372.05 (acute atopic conjunctivitis), 372.13 (vernal conjunctivitis) and 372.14 (other chronic allergic conjunctivitis). Only outpatient visits with the aforementioned ICD-9 codes as the major diagnosis were included in the study.
Air Quality and Weather Data
Daily ambient air-quality data between 2008 and 2012 were obtained from the database of the Shanghai Key Laboratory of Meteorology and Health (SKLMH)27. Ambient air pollutants included in the analysis were PM10, PM2.5, NO2, O3 and SO2. Weather data (daily mean temperature, relative humidity and wind velocity) were also obtained. All data were collected on an hourly basis. We calculated the daily average for each variable and then calculated the weekly average for use in this study. The study protocol was approved by the ethics committee of the Shanghai Eye, Ear, Nose and Throat Hospital and the SKLMH. The requirement for informed consent was waived.
Statistical Analysis
The univariate generalized least squares (GLS) model was used to evaluate the effect of the environmental factors on the outpatient attendance of allergic conjunctivitis. For the environmental and clinical data, we first took the average by each calendar week to eliminate the periodic trends caused by patients’ regular working hours. The time series of interest were then fit to a simple linear regression model. We applied the Ljung–Box method to the residual of the linear model to determine the correlation structure between the two time series (moving average, autocorrelation) and the corresponding latency (p, q). The Ljung–Box test is to test28:
H0: The data are independently distributed.
Ha: The data are dependent on each other, they exhibit serial correlation.
Finally, a GLS model with correlation structure of autoregressive–moving-average (ARMA; p, q) was used to evaluate the association between environmental factors and outpatient attendance. ARMA models are widely used in hydrology29, econometrics30 and other fields31. The ARMA model consists of two parts, an autoregressive (AR) part, represented by p (the order of the autoregressive part) and a moving average (MA) part, represented by q (the order of the moving average part).
The GLS model is written as:

where Y is defined as the outpatient attendance of allergic conjunctivitis, X denotes an environmental factor, ε is the residual error (from which we constructed the ARMA [p, q]), Ω is a known matrix of the conditional variance of the error when given X and β is an unknown coefficient to be estimated. We called the test P of the regression coefficient significant if it was less than 0.05. We used R software version 3.1 (www.r-project.org) for all of the statistical analyses. The R packages we used in this study include “nlme”, “zoo” and “car”. All P values were based on two-sided tests.
In order to determine the time-lag effects of the pollutants, we used the Ljung–Box test to evaluate the significance of correlation between outpatient visits and the concentration of pollutants in the past with time-lags of 1 week to 5 weeks, respectively (Supplemental file 3). The time-lag was then determined as the first time point where the test P value became insignificant (more than 0.1). Most of the pollutants were found to show significant time-lag effects in week 3, therefore we established the ARMA [p = 3, q = 0] except for SO2, which had a time-lag of 1 week. To set our age groups, we compared the results of principal component analysis (<20, 20–50 and >50 years, Supplemental file 4) with the Chinese hospital standard.for age classification (childhood and adolescence, <18 years; adult, 18 to 40 years; middle age, 41 to 60 years; and elderly, >60 years, Table 4) and found that the two classifications did not match. To facilitate the understanding for clinicians and to have a relatively high resolution, we finally decided to use the latter age classification32.
Additional Information
How to cite this article: Hong, J. et al. Ambient air pollution, weather changes and outpatient visits for allergic conjunctivitis: A retrospective registry study. Sci. Rep. 6, 23858; doi: 10.1038/srep23858 (2016).
References
Zhang, J. et al. Environmental health in China: progress towards clean air and safe water. Lancet 375, 1110–1119 (2010).
Azari, A. A. & Barney, N. P. Conjunctivitis: a systematic review of diagnosis and treatment. JAMA 310, 1721–1729 (2013).
Bielory, B. P., O’Brien, T. P. & Bielory, L. Management of seasonal allergic conjunctivitis: guide to therapy. Acta Ophthalmol 90, 399–407 (2012).
Mimura, T. et al. Airborne particulate matter (PM2.5) and the prevalence of allergic conjunctivitis in Japan. Sci Total Environ 487, 493–499 (2014).
Chang, C. J., Yang, H. H., Chang, C. A. & Tsai, H. Y. Relationship between air pollution and outpatient visits for nonspecific conjunctivitis. Invest Ophthalmol Vis Sci 53, 429–433 (2012).
Forsberg, B. et al. An expert assessment on climate change and health - with a European focus on lungs and allergies. Environ Health 11, S4 (2012).
McMichael, A. J., Woodruff, R. E. & Hales, S. Climate change and human health: present and future risks. Lancet 367, 859–869 (2006).
Kan, H., Chen, R. & Tong, S. Ambient air pollution, climate change and population health in China. Environ Int 42, 10–19 (2012).
Hwang, B. F. & Lee, Y. L. Air pollution and prevalence of bronchitic symptoms among children in Taiwan. Chest 138, 956–964 (2010).
Pan, G. et al. Air pollution and children’s respiratory symptoms in six cities of Northern China. Respir Med 104, 1903–1911 (2010).
Hwang, B. F., Lee, Y. L., Lin, Y. C., Jaakkola, J. J. & Guo, Y. L. Traffic related air pollution as a determinant of asthma among Taiwanese school children. Thorax 60, 467–473 (2005).
Riediker, M., Monn, C., Koller, T., Stahel, W. A. & Wüthrich, B. Air pollutants enhance rhinoconjunctivitis symptoms in pollen-allergic individuals. Ann Allergy Asthma Immunol 87, 311–318 (2001).
Lin, M., Stieb, D. M. & Chen, Y. Coarse particulate matter and hospitalization for respiratory infections in children younger than 15 years in Toronto: a case-crossover analysis. Pediatrics 116, e235–e240 (2005).
Xu, K. P. & Tsubota, K. Correlation of tear clearance rate and fluorophotometric assessment of tear turnover. Br J Ophthalmol 79, 1042–1045 (1995).
Andres, S., Garcia, M., Espina, M., Valero, J. & Valls, O. Tear pH, air pollution and contact lenses. Am J Optom Physiol Opt 65, 627–631 (1988).
Torricelli, A. A. et al. Correlation between signs and symptoms of ocular surface dysfunction and tear osmolarity with ambient levels of air pollution in a large metropolitan area. Cornea 32, e11–15 (2013).
Pacini, S. et al. Association between atmospheric ozone levels and damage to human nasal mucosa in Florence, Italy. Environ Mol Mutagen 42, 127–135 (2003).
Novaes, P. et al. Ambient levels of air pollution induce goblet-cell hyperplasia in human conjunctival epithelium. Environ Health Perspect 115, 1753–1756 (2007).
Fujishima, H. et al. Effects of diesel exhaust particles on primary cultured healthy human conjunctival epithelium. Ann Allergy Asthma Immunol 110, 39–43 (2013).
Huang, S. K., Zhang, Q., Qiu, Z. & Chung, K. F. Mechanistic impact of outdoor air pollution on asthma and allergic diseases. Journal of thoracic disease 7, 23–33, doi: 10.3978/j.issn.2072-1439.2014.12.13 (2015).
Garcia-Mozo, H. et al. Quercus pollen season dynamics in the Iberian peninsula: response to meteorological parameters and possible consequences of climate change. Ann Agric Environ Med 13, 209–224 (2006).
D’Amato, G. & Cecchi, L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin Exp Allergy 38, 1264–1274 (2008).
Leonardi, A. et al. Allergic conjunctivitis: a cross-sectional study. Clin Exp Allergy 45, 1118–1125, doi: 10.1111/cea.12536 (2015).
Mimura, T. et al. Rapid immunochromatographic measurement of specific tear immunoglobulin E in moderate to severe cases of allergic conjunctivitis with Immfast Check J1 in the spring. Cornea 30, 524–527, doi: 10.1097/ICO.0b013e3181f23932 (2011).
Ege, M. J. et al. GABRIELA Transregio 22 Study Group. Exposure to environmental microorganisms and childhood asthma. N Engl J Med 364, 701–709 (2011).
Huang, L., Pu, Z., Li, M. & Sundell, J. Characterizing the Indoor-Outdoor Relationship of Fine Particulate Matter in Non-Heating Season for Urban Residences in Beijing. PloS one 10, e0138559, doi: 10.1371/journal.pone.0138559 (2015).
Kan, H. et al. Season, sex, age and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPA) Study. Environ Health Perspect 116, 1183–1188, doi: 10.1289/ehp.10851 (2008).
Box, G. E. P. & Pierce, D. A. Distribution of Residual Autocorrelations in Autoregressive-Integrated Moving Average Time Series Models. Journal of the American Statistical Association 65, 1509–1526 (1970).
Camacho, F., McLeod, A. I. & Hipel, K. W. Multivariate contemporaneous ARMA model with hydrological applications. Stochastic Hydrol Hydraul 1, 141–154, doi: 10.1007/BF01543810 (1987).
Chib, S. & Greenberg, E. Bayes inference in regression models with ARMA (p, q) errors. Journal of Econometrics 64, 183–206 (1994).
Kizilkaya, A. & Kayran, A. ARMA model parameter estimation based on the equivalent MA approach. Digital Signal Processing 16, 670–681 (2006).
Yan, S. et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obesity reviews: an official journal of the International Association for the Study of Obesity 13, 810–821, doi: 10.1111/j.1467-789X.2012.01016.x (2012).
Acknowledgements
The authors thank Prof. Reza Dana and Prof. David A. Sullivan from Schepens Eye Research Institute, Massachusetts Eye and Ear Infirmary, Harvard Medical School, for their constructive critique and suggestions. The authors were supported by grants from the Key Clinic Medicine Research Program, the Ministry of Health, China (201302015); the National Science and Technology Research Program, the Ministry of Science and Technology, China (2012BAI08B01); the National Natural Science Foundation of China (81170817, 81200658, 81300735, 81270978, U1205025 and 81330022); the Scientific Research Program, Science and Technology Commission of Shanghai Municipality, Shanghai (13441900900, 13430720400); the Chinese Postdoctoral Fund (XMU135890); and the New Technology Joint Research Project in Shanghai Hospitals (SHDC12014114). The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
J.H., Q.L., T.Z. and Jianjiang X. were involved in the design of the study. Jianming X., X.Y., Z.M., H.L. and J.H. prepared and cleaned the data. J.H., A.M., Y.Z., H.L. and T.Z. conducted the statistical analysis and wrote the first draft. Y.L., A.M., X.S., Z.L., Y.Z., H.L., M.T. and Jianjiang X. helped to revise the paper. Z.L. and Jianjiang X. are the guarantors for the study. J.H., T.Z. and Q.L. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hong, J., Zhong, T., Li, H. et al. Ambient air pollution, weather changes and outpatient visits for allergic conjunctivitis: A retrospective registry study. Sci Rep 6, 23858 (2016). https://doi.org/10.1038/srep23858
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23858
This article is cited by
-
An update on the association between ambient short-term air pollution exposure and daily outpatient visits for conjunctivitis: a time-series study in Hangzhou, China
Environmental Science and Pollution Research (2023)
-
Long-term effects of meteorological factors and extreme weather on daily outpatient visits for conjunctivitis from 2013 to 2020: a time-series study in Urumqi, China
Environmental Science and Pollution Research (2023)
-
Size-specific particulate matter and outpatient visits for allergic conjunctivitis in children: a time-stratified case-crossover study in Guangzhou, China
Environmental Science and Pollution Research (2022)
-
Aktuelle und zukünftige Auswirkungen des Klimawandels auf die Augenheilkunde
Die Ophthalmologie (2022)
-
Fine particulate matter measured by satellites predicts the risk of age-related macular degeneration in a longitudinal cohort study
Environmental Science and Pollution Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.