Abstract
Performance of interferon-gamma release assays (IGRAs) is influenced by preanalytical, laboratory and host factors. The data regarding how critical illnesses influence IGRA results are limited. This study aimed to investigate IGRA performance among critically ill patients. Patients admitted to intensive care unit (ICU) were prospectively enrolled and underwent QuantiFERON-TB Gold In-Tube testing on admission and discharge. The associations between patient factors and IGRA results were explored. In total, 118 patients were included. IGRA results on admission were positive, negative and indeterminate for 10(9%), 36(31%) and 72(61%) patients. All indeterminate results were due to a low mitogen response. Indeterminate results were associated with higher disease severity and lower serum albumin levels. Ninety(76%) patients survived to ICU discharge and had repeat IGRA testing 13.3 ± 10.1 days after first ones. Of those, 43(48%) had indeterminate results and no IGRA conversion or reversion was observed. The majority (35/51, 69%) of ICU survivors with initial indeterminate results still had indeterminates on follow-up testing. Acute critical illnesses exert a significant impact on IGRA performance and a high proportion of indeterminate results was seen in ICU patients. This study highlights limitation of IGRAs in the critically ill and judicious selection of patients to be tested should be considered.
Similar content being viewed by others
Introduction
One-third of the individuals worldwide are infected with Mycobacterium tuberculosis (MTB)1. Among them, immunocompetent subjects have a 5–10% lifetime risk of progressing to active tuberculosis (TB). Thus, latent TB infection (LTBI) serves as a significant reservoir of future epidemics. Identification and treatment of LTBI is a key element in post-2015 strategy for global TB control2. The tuberculin skin test (TST) and interferon-gamma (IFN-γ) release assays (IGRAs) are currently available methods for diagnosis of LTBI. The TST has been the most widespread used test for detecting LTBI since a century ago3. Until recently, IGRAs arise as a promising alternative to the TST because of their equivalent sensitivity and improved specificity4,5. IGRAs are functional assays measuring T cell response to MTB-specific antigens in either whole blood or peripheral blood-derived mononuclear cells5. IGRAs also have advantages of an objective readout, no need for revisit and no boost effect compared to the TST4. In light of this, IGRAs have been incorporated into international guidelines for LTBI screening and diagnosis in several countries, either as a confirmatory test for a positive TST or as a substitute for the TST6.
Despite these logistical advantages, many issues regarding IGRAs, such as suboptimal reproducibility, unknown prognostic value and limited interpretive criteria, need to be settled7. The causes of considerable IGRA variability are far from fully understood. It has been shown that assay, preanalytical and analytical factors all have an impact on reproducibility of IGRA results8,9,10. Even a small change in blood volume or the extent of tube shaking may significantly influence IGRA performance11. These emphasize the importance of assay standardization and appropriate quality control. Additionally, IGRA performance may be altered because of host biological and immunological variations; certain chronic illnesses or conditions like age, malnutrition, lymphocytopaenia, human immunodeficiency virus (HIV) infection, malignancy and renal dysfunction are recognized ones12,13,14. Acute febrile illnesses or dysfunction of organs are associated with altered immune reactions15,16,17 and they may theoretically have effects on the performance and reproducibility of IGRAs. However, little is known about how acute insults affect IGRA results. Clinically, such data are essential because diagnosis and treatment decisions could be impacted by testing results. In this way, physicians would better realize the limitations in applying IGRAs.
In the present study, we aimed to investigate IGRA performance among patients suffering from acute critical illnesses. In addition, we explored patient factors, which may influence the IGRA results.
Methods
Study population
This prospective observational study was conducted in the National Taiwan University Hospital (NTUH). The study received approval from the Research Ethics Committee of the NTUH (201308080RIND) and written informed consent has been obtained from all patients before the study. In addition, the study was conducted in accordance with the amended Declaration of Helsinki. From May 2014 to December 2014, all critically ill patients were eligible for this study if they were aged 20 years or more and provided written informed consent. To study the effects of acute critical illnesses on the performance and reproducibility of IGRAs, patients were excluded if they were admitted from the ward or referred from another hospital, had hospitalizations in past 3 months, were not expected to survive or stay in the intensive care unit (ICU) longer than 24 hours, or had HIV infection.
Data collection
Variables retrieved included demographics, body mass index, comorbidities, history of prior TB, Bacillus Calmette-Guerin (BCG) vaccination status, diagnosis of acute illnesses, blood testing results, events during the ICU stay and patient outcomes. BCG vaccination status was assessed by examination for the presence of BCG scar and information from the patients. Acute physiology and chronic health evaluation (APACHE) II scores were calculated18.
Blood sampling and assays
Venous blood samples were obtained on ICU admission and again before discharge. To minimize preanalytical variability, blood sampling was done by a single technician and samples were transported within 1 hour to the laboratory and immediately processed. The QuantiFERON-TB Gold In-Tube (QFT-GIT) test (Qiagen, Carnegie, Australia) was applied in this study. The assays were performed strictly according to the manufacturer’s instructions19. To avoid laboratory variability, the QFT-GIT assay was done by the same experienced technician who was blinded to the clinical information. Positive, negative and indeterminate results were defined per manufacturer20. 20IGRA conversion was defined as a negative result at baseline and a positive result on subsequent testing; IGRA reversion was defined as a change from a positive QFT-GIT result to a negative QFT-GIT result according to CDC guidelines21. Because the upper limit of accuracy in QFT-GIT assays was an IFN-γ level of 10 international units (IU)/ml, all values greater than 10 IU/ml were truncated at 10 IU/ml for the analysis.
Statistical analysis
Analyses were conducted employing statistical software SPSS (version 15.0, SPSS Inc., Chicago, IL). Data were presented as mean ± standard deviation, number or number (%). Inter-group comparisons were analysed using the Student t test or one-way analysis of variance for continuous variables and χ2 or Fisher’s exact test for categorical variables. The multivariate logistic regression analysis was performed to identify independent factors to affect the QFT-GIT results. All P values were two-tailed and a P value of <0.05 denoted statistical significance.
Results
Patients
Between May and December 2014, 257 ICU patients were screened for eligibility and finally a total of 118 patients participated in the study (Fig. 1). Characteristics of the study subjects are listed in Table 1. The mean age was 62 years and 69 (59%) were men. The mean APACHE II score on ICU admission was 21. Previous BCG vaccination was confirmed in 105 (89%) patients and 10 (8%) study subjects had active or prior history of TB. The ICU and hospital mortality rates were 24% and 36%, respectively.
QFT-GIT results
Overall, 10 (9%) of the patients had a positive QFT-GIT result and 36 (31%) of the study subjects had a negative QFT-GIT result on ICU admission. All indeterminate results (72/118, 61%) were due to a low mitogen response. Patients with indeterminate QFT-GIT results tended to have higher ICU mortality than those with interpretable ones (20/72, 28% vs. 8/46, 17%; p = 0.196).
The comparison of the proportion of positive, negative and indeterminate QFT-GIT results between patient groups with different disease severity is shown in Table 2. Patients with a higher severity score had worse ICU and hospital outcomes. Indeterminate QFT-GIT findings occurred more often among patients with higher APACHE II scores compared with those with lower scores. Moreover, the mitogen response diminished as patients’ disease severity increased.
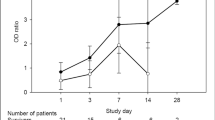
Variability of QFT-GIT results
Ninety (76%) patients survived to ICU discharge and had paired QFT-GIT results (Table 3). The interval between first and second IGRA testing was 13.3 ± 10.1 days. On ICU discharge, 43 (48%) ICU survivors had an indeterminate QFT-GIT result. Of note, 51 patients with an initial indeterminate result survived to be discharged from the ICU and 35 (69%) of them still had an indeterminate result. No IGRA conversion or reversion was found in this study. There was no difference in the time interval between paired QFT-GIT assays among patients with concordant (positive-positive [n = 9], negative-negative [n = 22], indeterminate-indeterminate [n = 35]) and discordant (positive-indeterminate [n = 1], negative-indeterminate [n = 7], indeterminate-negative [n = 16]) results (13.7 ± 12.1 vs. 13.5 ± 7.6 days; P = 0.958). Among 66 patients with concordant QFT-GIT results, those with persistent indeterminate results (n = 35) had higher disease severity, a lower serum albumin level and a worse in-hospital outcome compared to the others (Table 4).
Factors associated with indeterminate QFT-GIT results
Univariate analyses indicated that an indeterminate QFT-GIT result was associated with a higher APACHE II score and a lower serum albumin value (Table 5). The multivariate logistic regression analysis confirmed that both APACHE II score (odds ratio [OR] per 1 score increment: 1.09; 95% confidence interval [CI]: 1.04–1.15) and serum albumin (OR per 1 g/dl increment: 0.32; 95% CI: 0.15–0.69) were independent variables associated with indeterminate QFT-GIT results. Given that the low mitogen response accounted for all the indeterminate results, the relationships between the mitogen response and APACHE II scores or albumin levels were explored. Figure 2a,b show that patients with an APACHE II score <15 or a serum albumin value >3 g/dl had a significantly higher mitogen response compared to other patient groups.
Boxplots showing the relationships between the mitogen response and the APACHE II score (a) or serum albumin value (b).
*Significant difference (P < 0.05) compared with APACHE II score <15; #Significant difference (P < 0.05) compared with albumin >3 g/dl. APACHE, acute physiology and chronic health evaluation; IU, international unit.
Discussion
This is the first prospective study in the literature examining the IGRA response among critically ill patients. Our study shows that a high proportion (61%) of patients had indeterminate QFT-GIT results on ICU admission. Clinical characteristics associated with an indeterminate QFT-GIT result in this cohort included a higher APACHE II score and a lower serum albumin level. Moreover, APACHE II scores and albumin values were negatively and positively correlated with the mitogen response, respectively. In patients surviving to ICU discharge and having paired QFT-GIT results, no IGRA conversion or reversion was observed, but more than one third of patients had a persistent indeterminate QFT-GIT result. These findings have important implications for the use of IGRAs as diagnosing tools for LTBI or TB in the critically ill settings.
From prior studies of IGRAs in adults, widely varying proportions of indeterminate results, ranging from 0% to 41%, have been reported22,23. Numbers were discrepant on the basis of the population under study; the pooled rate of indeterminate results was 2.1% for the QFT-GIT assay, increasing to 4.4% among immunocompromised subjects24. An extraordinary high proportion (>20%) of indeterminate results has been observed in studies including a significant number of inpatients and HIV-infected patients23,25,26,27,28. Undoubtedly, immunocompromised state, particularly HIV infection, is an important predictor of an indeterminate IGRA result29,30. However, the impact of inpatient status on IGRA performance is seldom described in the literature. A recent paediatric study showed that indeterminate assays were associated with inpatient status (OR: 11.7) and the authors ascribed the causal relationship to modifiable factors, such as specimen handling, external to the patients31. Another study in the adult population also showed a high proportion (19.8%) of indeterminate test results among the inpatients, that was associated with host factors and preanalytical errors28.
In line with these two studies, a large proportion of our study subjects had indeterminate IGRA results and it is probable that critical ill patients were too sick to mount an immune response to the mitogen challenge, as shown in prior studies32. The findings that a higher APACHE II score correlated with a lower mitogen response and a higher proportion of indeterminates also support our contention. Moreover, compared to previous two studies, which were retrospective in nature, our prospective study had put a lot of efforts on eliminating preanalytical and laboratory variability24. Thus, we believe that host factors play a major role in determining the indeterminate results in our study population. In short, the presence of acute illnesses, particularly critical ones, significantly limits the interpretability of IGRAs and cost-effectiveness consideration and careful case selection are important parts in implementing IGRAs in this specific patient population.
Diagnosis of TB in the critically ill setting is challenging and delay in appropriate anti-TB therapy can be associated with worse ICU survival33. Usually, clinical symptoms, microbiological investigation and chest radiographs provide hints or evidence of TB disease. However, so-called characteristic features, such as fever, chronic productive cough and weight loss, are nonspecific among ICU patients. Acid-fast smears of respiratory samples, albeit providing rapid results, have the shortcoming of insufficient sensitivity for TB diagnosis34. The detection of MTB by culture, the gold standard for the definitive diagnosis of TB, takes time to yield results. In the ICU setting, studies failed to identify radiographic changes specific for TB35. Under such circumstances, IGRAs may be a viable modality to facilitate the diagnosis of TB. A recent meta-analysis reported a pooled sensitivity of 80% and specificity of 79% for the TB diagnosis using QFT-GIT assays, yet indeterminate results were excluded from the analysis34. In addition, none of the included studies specifically enrolled ICU patients. Taken together with our study showing a high percentage of indeterminate QFT-GIT results, it is advocated that the critically ill may not be appropriate candidates for IGRA testing.
In accordance with prior studies12,36, we found an association between indeterminate IGRA results and a lower serum albumin value. In critical illness conditions, hypoalbuminaemia is primarily a marker of the systemic inflammatory response that leads to protein-energy malnutrition. IGRA performance depends on intact cell-mediated immunity, especially the T-helper 1 type, that produces IFN-γ in response to the MTB-specific antigen and mitogen. Protein-energy malnutrition exerts several adverse effects on immunocompetence, including a reduction in the number and function of T cells, phagocyte dysfunction and compromised delayed cutaneous hypersensitivity37,38,39. Thus, it is unsurprisingly and biologically plausible that low albumin levels may increase the possibility of indeterminate results. However, it remains uncertain whether hypoalbuminaemia per se takes an influence on IGRA results36.
Besides technical factors, such as blood sampling and specimen processing, indeterminate QFT-GIT results are caused by an excess of T cell reactivity to the nil control or a limited response to the mitogen. All indeterminate results in our study were due to an inadequate mitogen response and this finding is in agreement with published experiences in the adult population28,30,40. An indeterminate IGRA result provides no information with regard to the likelihood of MTB infection. To date, it remains unknown what an indeterminate result means and the optimal follow-up of subjects with indeterminate results has not be established. Repeat QFT-GIT testing may be one of the choices41; however, in our cohort, more than two-thirds of patients with an indeterminate result and repeat testing had another indeterminate one. It is not surprising in that host factors accounting for indeterminate IGRA results in the critically ill may not be modifiable in the short run. Similarly, there are no recommendations on how to interpret repeatedly indeterminate results.
A number of limitations of the present study should be mentioned. First, in lack of a gold standard for diagnosis of LTBI, active TB disease usually serves as a surrogate. However, the limited number of TB patients in our study population makes it difficult to evaluate the diagnostic value of QFT-GIT in critically ill patients with TB. Second, our follow-up period was relatively short, i.e., up to hospital discharge; thus, we are unable to realize the longer-term effects of acute critical illnesses on IGRA performance. Third, the QFT-GIT assay was the only IGRA performed in this study and it is not possible to compare QFT-GIT to the other IGRA, T-SPOT.TB (Oxford Immunotec, Oxford, UK), in the ICU settings. Finally, although we have tried hard to eliminate preanalytical and laboratory variables that may influence IGRA results, we can not exclude the possibility of some unmeasured or unknown confounders in our study. Further studies are needed to resolve these limitations.
In conclusion, we found a large proportion of indeterminate IGRA results in the ICU patients and host factors, including the severity of critical illnesses and serum albumin levels, were associated with indeterminates. Moreover, the majority of patients with indeterminate results still did so on the follow-up testing. This study highlights the limitation in the performance of IGRAs among the critically ill. More works are required to identify best strategies to implement IGRAs and to explore undetermined factors associated with indeterminates in this particular patient population.
Additional Information
How to cite this article: Huang, C.-T. et al. Effects of acute critical illnesses on the performance of interferon-gamma release assay. Sci. Rep. 6, 19972; doi: 10.1038/srep19972 (2016).
References
World Health Organization. Global tuberculosis control: surveillance, planning, financing. Geneva, Switzerland (World Health Organization, 2009).
WHO End TB Strategy. Global strategy and targets for tuberculosis prevention, care and control after 2015. (2015) Available at: http://www.who.int/tb/post2015_strategy/en/. (Accessed: 2nd October 2015).
Huebner, R. E., Schein, M. F. & Bass, J. B. Jr. The tuberculin skin test. Clin. Infect. Dis. 17, 968–975 (1993).
Pai, M., Zwerling, A. & Menzies, D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann. Intern. Med. 149, 177–184 (2008).
Menzies, D., Pai, M. & Comstock, G. Meta-analysis: new tests for the diagnosis of latent tuberculosis infection: areas of uncertainty and recommendations for research. Ann. Intern. Med. 146, 340–354 (2007).
Mazurek, G. H. et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection-United States, 2010. MMWR. Recomm. Rep. 59, 1–25 (2010).
Herrera, V., Perry, S., Parsonnet, J. & Banaei, N. Clinical application and limitations of interferon-gamma release assays for the diagnosis of latent tuberculosis infection. Clin. Infect. Dis. 52, 1031–1037 (2011).
Doberne, D., Gaur, R. L. & Banaei, N. Preanalytical delay reduces sensitivity of QuantiFERON-TB gold in-tube assay for detection of latent tuberculosis infection. J. Clin. Microbiol. 49, 3061–3064 (2011).
Metcalfe, J. Z. et al. Test variability of the QuantiFERON-TB gold in-tube assay in clinical practice. Am. J. Respir. Crit. Care. Med. 187, 206–211 (2013).
van Zyl-Smit, R. N., Zwerling, A., Dheda, K. & Pai, M. Within-subject variability of interferon-g assay results for tuberculosis and boosting effect of tuberculin skin testing: a systematic review. PLoS. One. 4, e8517 (2009).
Gaur, R. L., Pai, M. & Banaei, N. Impact of blood volume, tube shaking and incubation time on reproducibility of QuantiFERON-TB gold in-tube assay. J. Clin. Microbiol. 51, 3521–3526 (2013).
Kobashi, Y. et al. Indeterminate results of QuantiFERON TB-2G test performed in routine clinical practice. Eur. Respir. J. 33, 812–815 (2009).
Ferrara, G. et al. Routine hospital use of a new commercial whole blood interferon-gamma assay for the diagnosis of tuberculosis infection. Am. J. Respir. Crit. Care. Med. 172, 631–635 (2005).
Madariaga, M. G., Jalali, Z. & Swindells, S. Clinical utility of interferon gamma assay in the diagnosis of tuberculosis. J. Am. Board. Fam. Med. 20, 540–547 (2007).
Berczi, I., Quintanar-Stephano, A. & Kovacs, K. Neuroimmune regulation in immunocompetence, acute illness and healing. Ann. N. Y. Acad. Sci. 1153, 220–239 (2009).
Kluth, D. C., Erwig, L. P. & Rees, A. J. Multiple facets of macrophages in renal injury. Kidney. Int. 66, 542–557 (2004).
Cabrera-Perez, J., Condotta, S. A., Badovinac, V. P. & Griffith, T. S. Impact of sepsis on CD4 T cell immunity. J. Leukoc. Biol. 96, 767–777 (2014).
Knaus, W. A., Draper, E. A., Wagner, D. P. & Zimmerman, J. E. APACHE II: a severity of disease classification system. Crit. Care. Med. 13, 818–829 (1985).
Cellestis. QuantiFERON-TB Gold package insert. Cellestis Limited, Carnegie, Victoria, Australia (Cellestis, 2013).
Detjen, A. K. et al. Short-term reproducibility of a commercial interferon gamma release assay. Clin. Vaccine. Immunol. 16, 1170–1175 (2009).
Mazurek, G. H. et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection-United States, 2010. MMWR. Recomm. Rep. 59, 1–25 (2010).
Mahomed, H. et al. Comparison of mantoux skin test with three generations of a whole blood IFN-gamma assay for tuberculosis infection. Int. J. Tuberc. Lung. Dis. 10, 310–316 (2006).
Baba, K. et al. Evaluation of immune responses in HIV infected patients with pleural tuberculosis by the QuantiFERON TB-Gold interferon-gamma assay. BMC. Infect. Dis. 8, 35 (2008).
Diel, R., Loddenkemper, R. & Nienhaus, A. Evidence-based comparison of commercial interferon-gamma release assays for detecting active TB: a metaanalysis. Chest. 137, 952–968 (2010).
Raby, E. et al. The effects of HIV on the sensitivity of a whole blood IFN-gamma release assay in Zambian adults with active tuberculosis. PLoS. One. 3, e2489 (2008).
Syed Ahamed Kabeer, B. et al. Role of interferon gamma release assay in active TB diagnosis among HIV infected individuals. PLoS. One. 4, e5718 (2009).
Tsiouris, S. J. et al. Sensitivity analysis and potential uses of a novel gamma interferon release assay for diagnosis of tuberculosis. J. Clin. Microbiol. 44, 2844–2850 (2006).
Fabre, V., Shoham, S., Page, K. R. & Shah, M. High proportion of indeterminate QuantiFERON-TB Gold In-Tube results in an inpatient population is related to host factors and preanalytical steps. Open. Forum. Infect. Dis. 1, ofu088 (2014).
Lange, B., Vavra, M., Kern, W. V. & Wagner, D. Indeterminate results of a tuberculosis-specific interferon-gamma release assay in immunocompromised patients. Eur. Respir. J. 35, 1179–1182 (2010).
Oni, T. et al. Risk factors associated with indeterminate gamma interferon responses in the assessment of latent tuberculosis infection in a high-incidence environment. Clin. Vaccine. Immunol. 19, 1243–1247 (2012).
Bui, D. H., Cruz, A. T. & Graviss, E. A. Indeterminate QuantiFERON-TB gold in-tube assay results in children: possible association with procedural specimen collection. Pediatr. Infect. Dis. J. 33, 220–222 (2014).
Haustein, T. et al. The likelihood of an indeterminate test result from a whole-blood interferon-gamma release assay for the diagnosis of Mycobacterium tuberculosis infection in children correlates with age and immune status. Pediatr. Infect. Dis. J. 28, 669–673 (2009).
Zahar, J. R. et al. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive. Care. Med. 27, 513–520 (2001).
Sester, M. et al. Interferon-gamma release assays for the diagnosis of active tuberculosis: a systematic review and meta-analysis. Eur. Respir. J. 37, 100–111 (2011).
Wu, J. Y. et al. The role of chest radiography in the suspicion for and diagnosis of pulmonary tuberculosis in intensive care units. Int. J. Tuberc. Lung. Dis. 13, 1380–1386 (2009).
Papay, P. et al. Predictors of indeterminate IFN-gamma release assay in screening for latent TB in inflammatory bowel diseases. Eur. J. Clin. Invest. 41 (2011).
Chandra, R. K. Numerical and functional deficiency in T helper cells in protein energy malnutrition. Clin. Exp. Immunol. 51, 126–132 (1983).
Niiya, T. et al. Impaired dendritic cell function resulting from chronic undernutrition disrupts the antigen-specific immune response in mice. J. Nutr. 137, 671–675 (2007).
Redmond, H. P. et al. Impaired macrophage function in severe protein-energy malnutrition. Arch. Surg. 126, 192–196 (1991).
Cho, K. et al. Factors Associated with Indeterminate and False Negative Results of QuantiFERON-TB Gold In-Tube Test in Active Tuberculosis. Tuberc. Respir. Dis. (Seoul). 72 (2012).
Powell, R. D. 3rd, Whitworth, W. C., Bernardo, J., Moonan, P. K. & Mazurek, G. H. Unusual interferon gamma measurements with QuantiFERON-TB Gold and QuantiFERON-TB Gold In-Tube tests. PLoS. One. 6, e20061 (2011).
Acknowledgements
This work was supported by National Taiwan University Hospital (NTUH.103-N2589 and NTUH.104-N2899). We thanked the staff of the Eighth Core Lab, Department of Medical Research, National Taiwan University Hospital for technical support during the study.
Author information
Authors and Affiliations
Contributions
C.T.H. contributed to the study design, data interpretation and analysis and drafting and approval of the manuscript. S.Y.R., Y.J.T., P.H.K., S.C.K., P.L.L., L.C.K., C.L.H., C.K.H., C.Y.Y., Y.C.C. and C.J.Y. contributed to the study design, data collection and analysis and approval of the manuscript. J.Y.W. had full access to all of the data in the study, took responsibility for the integrity of the data and the accuracy of the data analysis, critically reviewed and revised the manuscript and approved the submission of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Huang, CT., Ruan, SY., Tsai, YJ. et al. Effects of acute critical illnesses on the performance of interferon-gamma release assay. Sci Rep 6, 19972 (2016). https://doi.org/10.1038/srep19972
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep19972
This article is cited by
-
Low-dose steroids are associated with indeterminate QuantiFERON-TB Gold In-Tube assay results in immunocompetent children
Scientific Reports (2021)
-
Decreased ex vivo production of interferon-gamma is associated with severity and poor prognosis in patients with lupus
Arthritis Research & Therapy (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.