Abstract
Gefitinib is an essential drug for NSCLC patients harboring EGFR sensitive mutations. The approved dose 250mg/day is based on limited clinical trials, this research aims to explore the relationship between drug exposure and gefitinib response. Ctrough of 87 NSCLC patients harboring EGFR sensitive mutations were determined by LC-MS/MS. The median of Ctrough was 173.9 ng/ml (P25–P75, 130.5–231.2 ng/ml) and cutoff value 200 ng/ml was determined by X-Tile. The PFS between Ctrough < 200 ng/ml and Ctrough ≥ 200 ng/ml groups were not significantly different (17.3 VS 14.8 months; p = 0.258). Ctrough was not significantly associated with rash, diarrhea and hepatotoxicity. Non-smokers enjoyed longer PFS than smokers (18.7 VS 9.3 months; p = 0.025). The results showed that, for NSCLC patients with EGFR sensitive mutations, the PFS in lower trough concentration group were not inferior to that in higher trough concentration group and dose reduction is a rational suggestion for adjustment of dose regimen for aforementioned patients. More clinical trials are warranted to explore the precision dose schedule of gefitinib.
Similar content being viewed by others
Introduction
Gefitinib is an oral, reversible, tyrosine kinase inhibitor (TKI) of epidermal growth factor receptor (EGFR) that plays a key role in the biology of non small cell lung cancer (NSCLC). For patients with advanced NSCLC harboring EGFR-TKI sensitive mutations, using EGFR-TKI as first-line treatment, progression-free survival (PFS) was reported to be two to three times better than platinum-doublet chemotherapy1,2,3. Based on these results, EGFR-TKIs monotherapy has become a standard regimen for advanced NSCLC with EGFR mutations.
However, several questions need to be addressed regarding the approved dosage regimen (250mg/day) established based on limited clinical trials. According to the results of Iressa Dose Evaluation in Advanced Lung Cancer trial ı and trial ıı (IDEAL-1 and IDEAL-2), the doses 250 mg/day and 500 mg/day have comparable response rate in all the NSCLC patients4,5. Meanwhile, recently, a post hoc analysis from NEJ002 was conducted to examine the efficacy of dose-reduction gefitinib compared with that of standard-dose gefitinib in EGFR-mutated NSCLC patients. In this research, a dose reduction of gefitinib by changing the everyday schedule to every 2 days schedule was permitted when grade ıı toxicity was observed. Interestingly, the low-dose group showed not-inferior efficacy (response and survival) compared with standard-dose group6. However, Ichihara E. et al. reported that in EGFR-mutated NSCLC patients, PFS of the subjects with higher BSA was significantly worse than that of those with lower BSA and consequently postulated that blood concentrations were reversely correlated with BSA and then influenced the gefitinib response7. The postulations from Ichihara E.’s research are in contradiction with aforementioned clinical trials. To date, no study has been systemically conducted yet about the relationship between the gefitinib PKs and its effects in NSCLC patients with EGFR mutation. The dose regimen of 250 mg/day has not been optimized for this specific group of NSCLC patients.
Recently, the concept of “precision medicine” has been raised up to further discover inter-individual difference of therapy outcomes and provide the best available care for each individual8. For gefitinib, as aforementioned, available data to verify the relationship between dosage regimen, blood exposure and drug effects are limited in NSCLC patients with EGFR sensitive mutations. The objective of this study was to retrospectively explore the relationship between gefitinib trough concentration and clinical outcomes in both efficacy and safety in patients carrying EGFR sensitive mutations.
Results
Patients’ characteristics
In total, 87 patients were included in the final analysis. Patient characteristics were summarized in Table 1. 80 patients had major EGFR mutations (exon 19 deletions or exon 21 L858R), 7 patients carried other sensitizing-mutations, such as exon 21 L861Q, exon 20 frame insertion. The median BSA was 1.66 m2 (range, 1.26–2.06 m2). The median age was 56 years (range, 29–79). The number of male and female was roughly comparable. Most patients had good PS (performance status) and carried adenocarcinoma histology. 23 (26%) patients were post-operatively relapsed patients. 24 (28%) patients were former or current smokers. 9 patients (10%) suffered from CNS metastases after gefitinib administration. Table 2 compared the characteristics of the patients who were treated with gefitinib in the first-line setting with those in the later-line setting.
Association between clinicopathologic features and gefitinib trough concentration
The median of gefitinib trough concentration is 173.9 ng/ml (P25–P75, 130.5–231.2 ng/ml). For clinicopathologic features such as gender, BSA, PS, smoker, CNS metastases and age, no factor was significantly correlated with gefitinib trough concentration (Table 3). The association between the BSA and trough concentration was analyzed by Spearman rank correlation test, rs = −0.112 (P = 0.320). Gefitinib trough concentration was not correlated with CNS metastases. (Spearman rank correlation test, rs = −0.142, P = 0.194).
Relationship between gefitinib trough concentration and objective response, progression-free survival
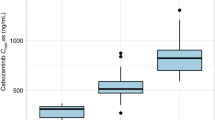
The objective response (complete response or partial response [PR]) rate is 57.5%. The disease control (complete response, partial response [PR] or stable disease [SD]) rate is 93.1%. In univariate analysis, gefitinib trough concentration was not a predictor of objective response. The log-rank test was used to compare progression-free survival in each subset of patients (Table 4). The PFS between Ctrough < 200 ng/ml and Ctrough ≥ 200 ng/ml were not significantly different (17.3 VS 14.8 months; p = 0.258, Fig. 1).
Relationship between clinicopathologic features and objective response, progression-free survival
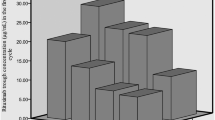
In univariate analysis, no factors were strong predictors of objective response. In log-rank test, non-smokers enjoyed longer progression-free survival than smokers (18.7 VS 9.3 months; p = 0.025, Fig. 2, Table 4).
Correlation between gefitinib trough concentration and toxicity
In binary logistic regression, trough concentration did not significantly associate with rash, diarrhea and hepatotoxicity (Table 5).
Discussion
Gefitinib is a standard therapy for NSCLC patients with EGFR sensitive mutations, however, few clinical trials have been conducted to discuss the association between gefitinib exposure and drug effect. Until now, whether the approved dose 250 mg/day is a rational dose schedule in patients with EGFR sensitive mutations remains disputable. We undertook this retrospective research to evaluate the impact of pharmacokinetic factors on gefitinib drug effect and adverse drug reaction in NSCLC patients with EGFR sensitive mutations. Our results indicated that, for patients with EGFR sensitive mutations, after using gefitinib 250 mg/day, the progression-free survival of Ctrough < 200 ng/ml group were not inferior to that in higher trough concentration (Ctrough ≥ 200 ng/ml) group. Meanwhile, trough concentration was not significantly associated with the adverse effects, including skin rash, diarrhea and hepatotoxicity. What’s more, non-smokers enjoyed better progression free survival. To our knowledge, this research provides the first evidence that the inter-patient pharmacokinetic variability is not the major cause of variation in gefitinib responses in patients with EGFR sensitive mutations.
One of the characteristics for molecularly targeted anticancer agents, the dose and response in efficacy and safety are not tightly correlated9,10. Regarding to gefitinib, 250 mg/day had a comparable response rate to 500 mg/day and milder adverse effects, in the Iressa Dose Evaluation in Advanced Lung Cancer (IDEAL-1 and –2) trials4,5. The results from NEJ002 study are similar, in which the progression-free survival and overall survival of dose-reduction group tended to be better, or at least similar to those of the standard-dose group6. Our results further confirmed this phenomenon. Recently, a retrospective study, focused on the relationship between BSA and PFS, demonstrated that for patients harboring EGFR mutations, the median PFS of the patients with higher BSA (≥1.5 m2) was significantly worse than that of those with lower BSA (<1.5 m2) (10.4 VS 18.0 months; p = 0.019, log-rank test). The authors postulated that blood concentrations were reversely correlated with BSA and then influenced the gefitinib response7. However, this postulation has not been confirmed in our study. In our research, the BSA and trough concentration were not significantly correlated.
Further, both preclinical and clinical research revealed that the concentrations of gefitinib in tumor and skin were much higher than plasma concentrations in xenograft mice and patients, indicating potential tissue concentration of gefitinib9,10,11. In this research, the trough concentration ranged from 34.0 ng/mL to 503.0 ng/mL. According to literature, the ratio of tumor concentration to plasma concentration ranged from 1.12~250 to 1 (median 40 to 1), which demonstrated tremendous interindividual variability12. Haura EB et al. reported that the lowest tumor concentration detected in operative tumor was 3.638 μM12, which was much higher than gefitinib IC50 for growth in cell lines with EGFR sensitive mutations (gefitinib IC50 for H3255 cell lines = 0.04 μM)13. Consistent with the results from IDEAL1 and IDEAL2 clinical trials, our research further proved that, in patients with EGFR sensitive mutations, once plasma levels adequate to block tyrosine kinase have been achieved, additional plasma concentration escalations are unlikely to improve response.
Our research showed that non-smokers enjoyed longer PFS for patients with EGFR sensitive mutations. This is consistent with the results from several randomized trials1,14,15. Whole genome sequencing analyses have shown that lung cancer due to tobacco smoking was associated with a significant higher number of mutations per Mb (mutations per Mb: median 10.5, range 4.9–17.6) compared to never-smokers with lung cancer (mutations per Mb: median 0.6, range 0.6–0.9)16. The differences in mutation frequencies and the distinctive sets of mutations may contribute to potential difference in the predictive and/or prognostic significance according to smoking history. Future investigations into the predictive difference by smoking history may lead to the optimization of current targeted therapy and detailed mechanism researches about the eruption of smoking-related lung cancer are of great value for cancer therapy.
As a targeted therapy agent, the tolerability profile of gefitinib is better than previous cytotoxic agents and the most common adverse events include rash, diarrhea, nausea and hepatotoxicity. Although Yuanyuan Zhao et al. found that in EGFR wide-type patients, those with Ctrough ≥ 200 ng/ml suffered more rash than with Ctrough < 200 ng/ml17. In our research, trough concentration was not significantly associated with skin rash, diarrhea and hepatotoxicity in patients with EGFR sensitive mutations. To date, some studies have shown that the mechanisms of these adverse effects are considerably complex and need to be answered18,19,20,21. In terms of cutaneous toxicities, no significant correlation were seen between dose levels and EGFR signaling pathway inhibition in skin biopsies9. What’s more, the eruption of cutaneous adverse drug reaction results from not only the inhibition of EGFR pathway, which acts as an initiation stage and leads to abnormal proliferation, migration and differentiation of keratinocytes22, but also the disruption of the integrity of the skin with the recruitment of inflammatory cells23. In conclusion, the blood concentration, in itself, is not enough to account for the interindividual variability of adverse drug reaction, indicating that it is the tissue specific concentration that results in related toxicity.
This research has some limitations. This type of study retrospectively analyzed heterogeneous data with regard to patient cohort and follow-up pattern, meaning that the study results seem speculative, not definitive. Therefore, our results should be interpreted cautiously. In addition, to date, a number of somatic mutations in the EGFR gene have been identified that are associated with increased activity of EGFR tyrosine kinase inhibitors and inherited polymorphisms in the EGFR gene have been associated with altered EGFR expression or function, future study should consider all these factors in the enrolled subjects.
In conclusion, our retrospective analysis suggests that, under standard-dose gefitinib, patients with lower trough concentration may be clinically equivalent to patients with higher trough concentration for NSCLC patients with EGFR sensitive mutations. In NSCLC patients with EGFR mutation under the dosage of 250 mg/day, gefitinib PKs and its clinical outcome were not closely correlated. Thus, dose reduction is a rational suggestion for adjustment of dose schedule. Prospective clinical trials to clarify and explore the precision dose schedule for patients with EGFR sensitive mutation are warranted. Meanwhile, non-smokers enjoyed better progression free survival for this specific group of NSCLC patients.
Material and methods
Subjects
The main patient entry criteria included: age ≥ 18 years; histologically and cytologically proved NSCLC; Eastern cooperative oncology group performance status (ECOG PS) ≤ 2; adequate hematological, renal and hepatic functions; direct sequencing and Real-time PCR proved EGFR sensitive mutations.
Main exclusion criteria were as follows: uncontrolled systemic disease, any evidence of clinically active interstitial lung diseases and other chemotherapy at the time of inclusion. The protocol was approved by the Ethical Committee of Cancer Center of Sun Yat-Sen University (CCSU) and written informed consent was obtained from each patient. The methods were carried out in accordance with the approved guidelines. This trial was registered with ClinicalTrials.gov, number NCT01994057 (date of registration: 2013/11/23).
BSA was calculated as follows: BSA (m2) = (body weight [kg]) 0.425 × (height [cm]) 0.725 × 0.007184
Drug administration and disease assessment
Patients were treated with gefitinib monotherapy, 250 mg/day, until progression. Before study entry and prior to each subsequent treatment cycle (the first duration cycle is one month, then the rest of intervals for tumor reassessment are two months), routine laboratory tests (hematology and biochemistry assessments) and full tumor assessment with computed tomography (CT) scans or magnetic resonance imaging (MRI) scans were performed by the investigator and radiologists according to the response evaluation criteria in solid tumors [RECIST]. Objective responses (complete response or partial response [PR]) were confirmed 4 or more weeks after responses were first observed, stable disease [SD] was confirmed 4 weeks after responses were first observed. CNS metastases were recorded as progression disease. Adverse events (AEs) were recorded, graded for toxicity using the NCI-CTC and assessed by the investigator.
Detection of trough concentration and EGFR mutation
Plasma samples (2 mL) were collected on days 28 prior to drug administration, first tumor and toxicity assessment, frozen at −80 °C until analysis. The steady state trough concentration was analyzed with validated high-performance liquid chromatographic method with tandem mass spectrometric (LC-MS/MS)24. Details of the assay and partial validation data were included in the Supplementary material. EGFR mutation analysis was conducted using a primary tumor, metastatic lesion, such as lymph mode metastasis, or pleural effusion. EGFR mutation status was assessed by direct sequencing and real-time PCR (RT-PCR).
Statistical analysis
Pharmacokinetic parameters were characterized by the use of descriptive statistics. The plasma gefitinib trough concentration (minimum steady-state concentration) was categorized into two groups: ‘low’ (trough concentration < 200 ng/ml) and ‘high’ (trough concentration ≥ 200 ng/ml). This trough concentration cutoff value was selected based on published data showing that a mean trough concentration of 0.40 μM (178.76 ng/ml) was achieved following oral dosing with gefitinib 250 mg9. Meanwhile, the cutoff value was validated by X-tile 3.4.7 independently25. Patients were further stratified according to gender (male versus female), smoking history (never vs. ever), tumor histology (adenocarcinoma versus non-adenocarcinoma), development of diarrhea or skin rash (yes vs. no) and trough concentration (‘high’ vs. ‘low’). The association between the potential predictive factors and trough concentration was analyzed by Spearman rank correlation test. Potential predictive factors were tested in univariate models (with chi-square tests or the Fisher exact test) to predict response to gefitinib. Kaplan–Meier analysis was used to estimate patient survival outcome. The log-rank test was used to compare the survival of patients with different predictive factors. Each analysis was two-sided, with a 5% significance level and a 95% confidence interval and was performed with SPSS 13.0 for Windows software.
Additional Information
How to cite this article: Xin, S. et al. The Dissociation of Gefitinib Trough Concentration and Clinical Outcome in NSCLC Patients with EGFR Sensitive Mutations. Sci. Rep. 5, 12675; doi: 10.1038/srep12675 (2015).
References
Mitsudomi, T. et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 11, 121–8 (2010).
Mok, T. S. et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361, 947–57 (2009).
Zhang, L. et al. Gefitinib versus placebo as maintenance therapy in patients with locally advanced or metastatic non-small-cell lung cancer (INFORM; C-TONG 0804): a multicentre, double-blind randomised phase 3 trial. Lancet Oncol 13, 466–75 (2012).
Fukuoka, M. et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer. Journal of Clinical Oncology 21, 2237–2246 (2003).
Kris, M. G. et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 290, 2149–58 (2003).
Satoh, H. et al. Low-dose gefitinib treatment for patients with advanced non-small cell lung cancer harboring sensitive epidermal growth factor receptor mutations. J Thorac Oncol 6, 1413–7 (2011).
Ichihara, E. et al. Impact of physical size on gefitinib efficacy in patients with non-small cell lung cancer harboring EGFR mutations. Lung Cancer 81, 435–9 (2013).
Mirnezami, R., Nicholson, J. & Darzi, A. Preparing for precision medicine. N Engl J Med 366, 489–91 (2012).
Albanell, J. et al. Pharmacodynamic studies of the epidermal growth factor receptor inhibitor ZD1839 in skin from cancer patients: histopathologic and molecular consequences of receptor inhibition. J Clin Oncol 20, 110–24 (2002).
McKillop, D. et al. Tumor penetration of gefitinib (Iressa), an epidermal growth factor receptor tyrosine kinase inhibitor. Mol Cancer Ther 4, 641–9 (2005).
Marko-Varga, G. et al. Drug localization in different lung cancer phenotypes by MALDI mass spectrometry imaging. J Proteomics 74, 982–92 (2011).
Haura, E. B., Sommers, E., Song, L., Chiappori, A. & Becker, A. A pilot study of preoperative gefitinib for early-stage lung cancer to assess intratumor drug concentration and pathways mediating primary resistance. J Thorac Oncol 5, 1806–14 (2010).
Paez, J. G. et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304, 1497–500 (2004).
Rosell, R. et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13, 239–46 (2012).
Miller, V. A. et al. Afatinib versus placebo for patients with advanced, metastatic non-small-cell lung cancer after failure of erlotinib, gefitinib, or both and one or two lines of chemotherapy (LUX-Lung 1): a phase 2b/3 randomised trial. Lancet Oncol 13, 528–38 (2012).
Govindan, R. et al. Genomic landscape of non-small cell lung cancer in smokers and never-smokers. Cell 150, 1121–34 (2012).
Zhao, Y. Y. et al. The relationship between drug exposure and clinical outcomes of non-small cell lung cancer patients treated with gefitinib. Med Oncol 28, 697–702 (2011).
Lacouture, M. E. Mechanisms of cutaneous toxicities to EGFR inhibitors. Nat Rev Cancer 6, 803–12 (2006).
Hare, K. J., Hartmann, B., Kissow, H., Holst, J. J. & Poulsen, S. S. The intestinotrophic peptide, glp-2, counteracts intestinal atrophy in mice induced by the epidermal growth factor receptor inhibitor, gefitinib. Clin Cancer Res 13, 5170–5 (2007).
Kijima, T. et al. Safe and successful treatment with erlotinib after gefitinib-induced hepatotoxicity: difference in metabolism as a possible mechanism. J Clin Oncol 29, e588–90 (2011).
Ku, G. Y., Chopra, A. & Lopes Gde, L. Jr. Successful treatment of two lung cancer patients with erlotinib following gefitinib-induced hepatotoxicity. Lung Cancer 70, 223–5 (2010).
Manousaridis, I., Mavridou, S., Goerdt, S., Leverkus, M. & Utikal, J. Cutaneous side effects of inhibitors of the RAS/RAF/MEK/ERK signalling pathway and their management. J Eur Acad Dermatol Venereol 27, 11–8 (2013).
Zaiss, D. M. et al. Amphiregulin enhances regulatory T cell-suppressive function via the epidermal growth factor receptor. Immunity 38, 275–84 (2013).
Zhao, M. et al. Specific method for determination of gefitinib in human plasma, mouse plasma and tissues using high performance liquid chromatography coupled to tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 819, 73–80 (2005).
Camp, R. L., Dolled-Filhart, M. & Rimm, D. L. X-tile: A new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clinical Cancer Research 10, 7252–7259 (2004).
Acknowledgements
This research was funded by the China national natural science foundation: 81173131, 81072708, 81102515 and 81372502; the National Major Scientific and Technological Special Project for “Significant New Drugs Development” during the Twelfth Five-year Plan Period 2012ZX09506001-004 and the National High Technology Research and Development Program of China (2012AA02A502).
Author information
Authors and Affiliations
Contributions
S.X., Y.Y.Z., X.D.W., L.Z. and M.H. wrote the manuscript and designed the research; Y.Y.Z, Y.H., J.Z., Y.X.M., Z.H.H. and L.Z. recruited the patients and collected the samples; S.X., J.L.L, L.Y.C. and H.L.L. performed the research; S.X., Y.Y.Z., Y.G. and X.D.W. analyzed the data. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xin, S., Zhao, Y., Wang, X. et al. The Dissociation of Gefitinib Trough Concentration and Clinical Outcome in NSCLC Patients with EGFR Sensitive Mutations. Sci Rep 5, 12675 (2015). https://doi.org/10.1038/srep12675
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep12675
This article is cited by
-
Therapeutic Drug Monitoring of Kinase Inhibitors in Oncology
Clinical Pharmacokinetics (2023)
-
Rational application of gefitinib in NSCLC patients with sensitive EGFR mutations based on pharmacokinetics and metabolomics
Acta Pharmacologica Sinica (2022)
-
Optimized Dosing: The Next Step in Precision Medicine in Non-Small-Cell Lung Cancer
Drugs (2022)
-
Lung cancer organoids analyzed on microwell arrays predict drug responses of patients within a week
Nature Communications (2021)
-
Polymorphisms of NF-κB pathway genes influence adverse drug reactions of gefitinib in NSCLC patients
The Pharmacogenomics Journal (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.