Abstract
Study design: Case report of a 31-year-old woman who presented with toxic myelopathy due to intrathecal administration of doxorubicin.
Objective: To describe the pathology and the rehabilitation of an uncommon complication of intrathecal drug administration during the oncologic treatment of acute lymphoma.
Setting: Spinal cord rehabilitation center, University Hospital.
Method: Clinical and radiological observations during a rehabilitation program.
Results: Evidence of neurological improvement and rehabilitation potential after severe myelopathy due to intrathecal injection of doxorubicin.
Conclusion: This is, to our knowledge, the first report of severe myelopathy following accidental intrathecal administration of doxorubicin. Despite early complete paraplegia, some neurological and functional recovery was observed.
Similar content being viewed by others
Introduction
Toxic myelopathy is a rare complication of chemotherapy, especially when used intrathecally. The course is, in the majority of cases, bad, often leading to death or severe neurological sequelae.1,2,3,4,5,6,7,8,9,10,11,12 In the last 40 years, 39 cases were reported in the literature. Only 25% of patients recover completely.12 The principal cause is erroneous intrathecal administration of vincristine, methotrexate and cytosine-arabinoside (ARA-C).
The variety of neurological lesions is wide, from central cord necrosis to polyradiculopathy, and ascending myelitis. The histopathology shows either oedema, necrosis of neural tissue or myelitis.1,2,3,4,5,6,11,13
We report a patient with complete paraplegia, level L2, American Spinal Injury Association (ASIA) A, following the intrathecal administration of doxorubicin with incomplete neurological recovery. This is the first case with paraplegia following intrathecal administration of doxorubicin.
Case report
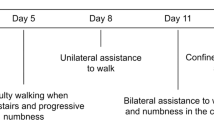
A 31-year-old woman presented with a spontaneous fracture of the sixth thoracic vertebra. Examination revealed a stage IV aggressive lymphoblastic lymphoma. Following anterior decompression and lateral Th5-7 spondylodesis, a LALA 94B protocol (Work Group Leucémie Aiguë Lymphoblastique de l'Adulte) was applied, consisting of daunorubicin 30 mg/m2, cyclophosphamide 750 mg/m2, vincristine 2 mg and prednisone 60 mg/m2, combined with intrathecal chemotherapy with cytarabine (ARA-C), methotrexate and prednisolone. In the course of this treatment, an erroneous lumbar injection of 14.5 mg of doxorubicin was administered instead of methotrexate. Cerebrospinal fluid (CSF) exchange at a rate of 20 cm3/h for a total amount of 500 cm3 was immediately initiated. The lumbar puncture at 24 h revealed a protein of 1.58 g/l. Despite this treatment, hypoesthesia, paraparesis and incontinence progressively developed over 7 days. A repeated CSF examination after 10 days revealed severe inflammation of the meninges and the spinal cord with a protein of 1.95 g/dl and white cell count of 23/ml (7% polymorphonuclear, 32% lymphocytes and 61% monocytes). Magnetic resonance imaging (MRI) was compatible with severe arachnoiditis of the conus medullaris and cauda equina. After 18 days, CSF protein had increased to 3.74 g/l. High dose intravenous methylprednisolone (500 mg/day) for 7 days and immunoglobulin (22 g/day) for 5 days were given without any improvement. The first two electroneuromyographic studies (ENMG), at 14 and 39 days (Table 1), indicated intact peripheral sensory nerve conduction and normal amplitudes of motor potentials. However, a complete paraplegia type ASIA A progressively developed, with a Th8 sensory level and bladder and bowel dysfunction. One month after the onset, the patient was admitted to our spinal cord injury unit. We began training in activities of daily living (ADL) and transfers to the wheelchair. After 3 weeks, she became drowsy, febrile and had meningism. MRI indicated acute quadriventricular hydrocephaly and contrast enhancement of the meninges, indicating adhesive arachnoiditis. A ventriculo-peritoneal shunt was placed resulting in a rapidly improved clinical state. An ENMG after 74 days indicated axonotmesis with massive fibrillations in the muscle quadriceps femoris and the muscle tibialis anterior. The MRI showed a persisting T2-hypersignal in the cona medullaris (Figure 1) with an extension of the arachnoïditis to the brainstem. After 3 months of complete paraplegia, we observed discrete contractions in the right quadricipital, tibialis anterior and plantar flexor group. At 6 months, the global motor score of key muscles (ASIA motor scoring) in the lower limbs was markedly improved. Only the left tibialis anterior muscle and both extensor hallucis were below 3/5 when using the ‘make and break’ technique. At discharge, 8 months after the intrathecal injection of doxorubicin, all tested muscles of the lower limbs had a strength of 3/5 or more, except for the left extensor hallucis (M2/5). The motor score of lower limbs according to the ASIA Classification was 34/50.
During the 7 month-stay in our rehabilitation center, she followed a multidisciplinary rehabilitation program with occupational therapy and physiotherapy, associated with vesico-sphincteral management. She rapidly learned self-catheterization. Occupational therapy led to rapid progress in the activities of daily living with a Barthel-score from 25/100 at the admission time in our rehabilitation center to 90/100 at discharge. In the beginning, physiotherapy was focused on muscular reinforcement of the trunk and upper limbs and passive mobilization of the limbs. Then a more active program with in- and out-water therapy, charge-progressive deambulation and treadmill-walking followed. At discharge, the patient was able to walk alone for 10 m with two crutches, at a low speed of 1 km/h, standing alone for a few seconds and walking 11 steps up and down. For longer distances, the patient still used her wheelchair. Also, urinary stress-leaks disappeared, due to better perineal control.
Discussion
The present article describes, to our knowledge, the first patient with complete paraplegia following accidental intrathecal administration of doxorubicin, treated by a LALA-chemotherapy for an aggressive stage IV lymphoblastic lymphoma with incomplete neurological recovery in approximately 14 months. The literature about the toxic complications of intrathecal use of chemotherapeutic agents provides 39 cases since 1960. Thus, Garcia-Tena12 reviewed 36 cases of erroneous intrathecal administration of chemotherapeutic agents, such as vincristine or doxorubicin. The overall prognosis of such a complication was bad; only nine patients (25%) had complete neurological recovery. More impressive is that approximately the same percentage (22.2%) have no recovery and 36.1% of persons died. It has been postulated that the main physiopathological process is necrosis at the medullary or central brain level with cellular edema, associated with diffuse axonal degeneration and demyelinization. In these cases, the evolution leads to death. Other reports, showing medullar edema, arachnoiditis or hydrocephaly have observed neurological and functional recovery.1,2,3,5,6,11,13
The most efficient therapy seems to be CSF drainage, ventriculo-peritoneal derivation, systemic administration of folinic acid or glutamate.14,15,16,17,18 In our case, a CSF exchange was performed.
Regarding the recovery potential, our case illustrates that a bad initial course should not necessarily be considered as definitive and does not preclude successful rehabilitation. The patient presented a three-phase clinical evolution: first, the neurological deterioration to complete flaccid paraplegia within 20 days, then the development of a tetraventricular hydrocephaly due to probable adhesive arachnoiditis after 7 weeks and finally, an incomplete neurological recovery, 14 months after the intrathecal administration of doxorubicin, allowing the patient to walk short distance with two crutches.
In summary, very few cases of central cord complications after erroneous intrathecal administration of chemotherapeutic agents have been described in the literature. Despite the fact that the overall prognosis of such patient is bad with 36.1% death and 22.2% having no recovery, a long-term active rehabilitation program and consequent management of complications are warranted in these cases.
References
Slyter H, Liwnicz B, Herrick MK, Mason R . Fatal myeloencephalopathy caused by intrathecal vincristine. Neurology 1980; 30: 867–871.
Williams ME, Walker AN, Bracikowski JP, Garner L, Wilson KD, Carpenter JT . Ascending myeloencephalopathy due to intratechal vincristine sulfate. A fatal chemotherapeutic error. Cancer 1983; 51: 2041–2047.
Manelis J, Freudlich E, Ezekiel E, Doron J . Accidental intratechal vincristine administration. Report of a case. J Neurol 1982; 228: 209–213.
Resar LM, Phillips PC, Kastan MB, Leventhal BG, Bowman PW, Civin CI . Actue neurotoxicity after intratechal cytosine arabinoside in two adolescents with acute lymphobastic leukemia of B-cell type. Cancer 1993; 71: 117–123.
Mena H, Garcia JH, Velandia F . Central and peripheral myelinopathy associated with systemic neoplasia and chemotherapy. Cancer 1981; 48: 1724–1737.
Kwack EK, Kim DJ, Park TI, Cho KR, Kkwon IH, Sohn YK . Neural toxicity induced by accidental intrathecal vincristine administration. J Korean Med Sci 1999; 14: 668–692.
Arico M, Nespoli L, Porta F, Caselli D, Raiteri E, Burgio GR . Severe acute encephalopathy following inadvertent intrathecal doxorubicin administration. Med Pediatr Oncol 1990; 18: 261–263.
Meggs WJ, Hoffman RS . Fatality resulting from intraventricular vincristine administration. J Toxicol Clin Toxicol 1998; 36: 243–246.
Al Fawaz IM . Fatal myeloencephalopathy due to intratechal vincristine administration. Ann Trop Paediatr 1992; 12: 339–342.
Zaragoza MR, Ritchey ML, Walter A . Neurourologic consequences of accidental intratechal vincristine: a case report. Med Pediatr Oncol 1995; 24: 61–62.
Kleinschmidt-DeMasters BK, Yeh M . ‘Locked-In-Syndrome’ after intratechal cytosine arabinoside therapy for malignant immunoblastic lymphoma. Cancer 1992; 70: 2504–2507.
Garcia-Tena J et al. Intratechal chemotherapy-related myeloencephalopathy in a young child with acute lymphoblastic leukemia. Pediatr Hematol Oncol 1995; 12: 377–385.
Ribeiro C, Reis FC . Adhesive lumbar arachnoiditis. Acta Med Port 1998; 11: 59–65.
Gaidys WG, Dickerman JD, Walters CL, Young PC . Intratechal vincristine. Report of a fatal case despite CNS washout. Cancer 1983; 52: 789–801.
Lafolie P, Liliemark J, Bjork O, Aman J, Wranne L, Peterson C . Exchange of cerebrospinal fluid in accidental intrathecal overdose of cytarabine. Med Toxicol Adverse Drug Exp 1998; 3: 248–252.
Al Feraysan A, Russell NA, Al Wohaibi M, Awada A, Scherman B . Cerebrospinal fluid lavage in the treatment of inadvertent intrathecal vincristine injection. Childs Nerv Syst 1999; 15: 87–89.
Grush OC, Morgan SK . Folinic acid rescue for vincristine toxicity. Clin Toxicol 1979; 14: 71–78.
Michelagnoli MP, Bailey CC, Wilson I, Livingston J, Kinsey SE . Potential salvage therapy for inadvertent intratechal administration of vincristine. Br J Haematol 1997; 99: 364–367.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jordan, B., Pasquier, Y. & Schnider, A. Neurological improvement and rehabilitation potential following toxic myelopathy due to intrathecal injection of doxorubicin. Spinal Cord 42, 371–373 (2004). https://doi.org/10.1038/sj.sc.3101592
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101592