Abstract
Study design: Case report of two subjects.
Objective: Charcot joints of the spine as a cause of Autonomic Dysreflexia in spinal cord lesions.
Setting: Stoke Mandeville Hospital, UK.
Method: Two patients with long standing spinal cord lesions developed symptoms of headaches and sweating associated with sitting up and transfers. In both cases no other cause was found to account for Autonomic Dysreflexia.
Result: Charcot Joints of the spine below the level of injury were demonstrated in both cases and symptoms resolved with prolonged bed rest.
Conclusion: As care of spinally injured patients continues to improve, they live longer and lead a more active lifestyle, it is expected that the incidence and prevalence of Charcot's joints will increase. Therefore the knowledge and heightened awareness of this entity, early diagnosis and detection with plain X-rays for urinary surveillance, may reduce the morbidity in spinal cord injured patients.
Similar content being viewed by others
Introduction
Autonomic dysreflexia is usually associated with disturbance of bowel or bladder function.1,2,3 However, if patients develop symptoms on movement and sitting up, lesions of the lumbar spine should be considered. Charcot's joints of the spine in association with lesions of the spinal cord are well recognised.4,5,6,7,8,9,10,11,12,13 We report two cases that presented with sweating and headaches associated with sitting up and transfers.
Case 1
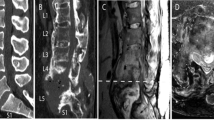
A tetraplegic man, now aged 53 years, sustained a C7–T1 complete (Frankel A) injury following a road traffic accident in 1971. Thirty years later he presented to the spinal outpatients with severe headaches and neck pain, on sitting up and during transfers. He was unable to maintain his mobility and independence. No recent changes had occurred in relation to his bowel habit, bladder or skin. Blood pressure on sitting ranged from 170/90 to 210/100. Thee were no other abnormal features on examination. Routine A-P X-ray of the urinary tract, showed a Charcot joint at T11–12, with underlying radiological features of ankylosing spondylitis (Figure 1). MRI scan showed changes in keeping with Charcot's joint at T11–12 (Figure 2). C-reactive protein was 3, ESR 8, Treponemal antibody tests were negative and together with MRI appearances, we concluded that the changes were due to Charcot's joint and not as a result of malignancy or infection.
Surgical fusion was considered but the patient was reluctant to consider an operation at that time. Bed rest was maintained for 6 weeks followed by gradual mobilisation, over a period of 2 weeks, during which time his symptoms resolved, and since that time there have been no further episodes of dysreflexia.
Case 2
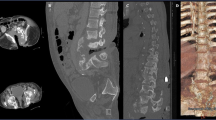
A man now aged 61 years sustained a C5 complete (Frankel A) injury, following a road traffic accident in 1966. He sustained a fracture at C5–6 that was treated conservatively. Thirty years later he presented with headaches and sweating, particularly, during the daytime and while sitting. There was an increase in spasticity. Blood pressure on sitting ranged from 170/80–190/100, and all other clinical examinations were normal. Plain X-rays of the spine showed extensive degeneration changes and ankylosis involving the lower thoracic and lumbar spine, and Charcot's joints at L4–5 and L5–S1 levels (Figure 3). MRI scan indicated these joints to be neuropathic in origin and not malignant or infected (Figure 4). He was treated with bed rest for a period of 8 weeks, during which symptoms of sweating and headaches resolved, and remain so at 4-year follow-up.
MRI of Lumbar spine, sagittal T2 weighted image. There is collapse at L5 with replacement of the L4–5 level with extensive high signal tissue anteriorly and changes in the posterior elements. Appearances are of pseudoarthrosis with surrounding inflammatory changes at L4–5 level. There is associated canal stenosis adjacent to the L4–5 level and ankylosis at some of the other levels of lumbar spine
Discussion
Jean Martin Charcot described neuropathic joints in association with neuro-syphilis.13,14 Any condition where joints have an impairment in the protective sensation but retained motor power, as in diabetic neuropathy, spinal dysraphism and syringomyelia, Charcot's joints may occur.4,5,6,7,8,9 However in complete spinal cord injury, movement occurs involuntarily during transfers and pressure relief.9 Degenerative changes of the lower spine are common in wheelchair users, and in some patients changes progress to form Charcot's joints.
Although autonomic dysreflexia is a useful warning mechanism it can be a distressing and often alarming symptom in patients with spinal cord injury. Alteration in the function or distension of urinary bladder, large bowel, rectum and the anal canal are the most common causes of autonomic dysreflexia.1,2,3 Less common causes are catheterisation and manipulation of indwelling catheters, urinary tract infections and urinary calculi.1,2,3 Diseases of the gastrointestinal tract such as peptic ulcers, haemorrhoids and anal fissures may induce dysreflexic symptoms.1,2,3 Cutaneous stimuli from pressure sores, paronychia, and burns, along with limb fractures, vertebral fractures below the level of injury, joint dislocations and heterotopic ossification can be responsible for autonomic dysreflexia.1,2,3 Sexual intercourse, ejaculation, pregnancy and labour are some other causes.1,2,3 Syringomyelia below the level of spinal cord lesion and muscle spasms are also reported to cause dysreflexic symptoms.1,2,3 Infections in other hollow organs such as appendicitis and cholecystitis are some other causes.1,2,3 In all these cases, sitting up lowers the blood pressure and relieves headache. If, however, dysreflexic symptoms occur on movements and are aggravated as a result of sitting up, it is important to consider lesions of the lower spine and the hips, as an underlying cause. Beard et al.15 reported a case of positional autonomic dysreflexia in a patient with sacral fracture.
Charcot's joints are a recognised entity in spinal cord injured patients, but may be overlooked as a precipitating cause for dysreflexic symptoms, especially as they commonly occur below the level of spinal cord injury and fracture. As care of spinally injured patients continues to improve, they live longer and lead a more active lifestyle, it is expected that the incidence and prevalence of Charcot's joints will increase. Therefore a heightened awareness is essential to exclude them. A routine plain X-ray for the surveillance of the urinary tract performed in the spinal outpatients is sufficient for initial diagnosis, as in our first patient.
References
Karlsson AK . Autonomic dysreflexia Spinal Cord 1999 37: 383–391
Mathias CJ, Bannister R . Autonomic disturbances in spinal cord lesions In: Autonomic failure: A textbook of clinical disorders of the autonomic nervous system 4th Edn Oxford University Press 1999 pp. 494–513
Mathias CJ, Frankel HL, Cole JD . Management of cardiovascular abnormalities caused by autonomic dysfunction in spinal cord injury In: Spinal Cord Dysfunction Vol II: Oxford: Oxford University Press 1992 pp. 101–120
Kalen V, Isono SS, Cho CS, Perkash I . Charcot arthropathy of the spine in longstanding paraplegia Spine 1987 12: 42–47
Slaburgh PB, Smith TK . Neuropathic spine after spinal cord injury J Bone Joint Surg [Am] 1978 60: 1005–1006
Sobel JW, Bohlman HH, Freehafer AA . Charcot's arthropathy of the spine following spinal cord injury J Bone Joint Surg [AM] 1985 67: 771–776
Shwartz HS . Traumatic Charcot Spine J of Spinal Disorders 1990 3: 269–275
Wirth CR, Jacobs RL, Rolander SD . Neuropathic Spinal Arthropathy: A Review of the Charcot Spine Spine 1980 5: 558–567
Eloesser L . On the nature of neuropathic affections of the joints Ann Surg 1917 55: 201
Hoppenfield S, Gross M, Giangarra C . Non-operative treatment of neuropathic spinal arthropathy Spine 1990 6: 54–56
Kapila A, Lines M . Neuropathic spinal arthropathy: CT and MR findings J Comput Assist Tomogr 1987 11: 736–739
Zucker G, Marder MJ . Charcot spine due to diabetic neuropathy Am J Med 1952 12: 118–124
Johnston JTH . Neuropathic fractures and joint injuries: pathogenesis and rationale of prevention and treatment J Bone Joint Surg [AM] 1967 49: 1–30
Charcot JM . Sur quelques arthropathies qui paraissant dependre d'une lesion du cerveau on de la moelle epinèere Arch Physiol Norm Pathol 1868 1: 161–178
Beard JP, Wade WH, Barber DB . Sacral insufficiency stress fracture as etiology of positional autonomic dysreflexia: Case report Paraplegia 1996 34: 173–175
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Selmi, F., Frankel, H., Kumaraguru, A. et al. Charcot joint of the spine, a cause of autonomic dysreflexia in spinal cord injured patients. Spinal Cord 40, 481–483 (2002). https://doi.org/10.1038/sj.sc.3101345
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101345
Keywords
This article is cited by
-
Resection of hip heterotrophic ossification leads to resolution of autonomic nervous system dysfunction in a patient with spinal Charcot arthropathy: a case report
Spinal Cord Series and Cases (2020)
-
Surgical management of a complex case of Charcot arthropathy of the spine: a case report
Spinal Cord Series and Cases (2019)
-
Discovertebral (Andersson) lesion of the Ankylosing Spondylitis, a cause of autonomic dysreflexia in spinal cord injury
Spinal Cord Series and Cases (2016)
-
Charcot spinal arthropathy: an increasing long-term sequel after spinal cord injury with no straightforward management
Spinal Cord Series and Cases (2015)
-
Sitting imbalance cause and consequence of post-traumatic Charcot spine in paraplegic patients
European Spine Journal (2014)