Abstract
The dopamine D1/D2 agonist apomorphine (0.63 mg/kg) disrupted prepulse inhibition (PPI) of acoustic startle in rats, a model of sensorimotor gating deficits observed in schizophrenia. All current antipsychotics, which antagonize D2 receptors, prevent this apomorphine-induced deficit. A novel class of antipsychotics possesses, in addition to D2 antagonist property, various levels of 5-HT1A agonist activity. Considering that the latter itself produces PPI deficits, it appeared necessary to assess the potential of this novel class of antipsychotics to reverse apomorphine-PPI deficits. Potent D2 antagonists, like haloperidol (0.63–2.5 mg/kg), risperidone (0.63–10 mg/kg), and olanzapine (0.63–40 mg/kg) prevented apomorphine PPI disruption. The atypical antipsychotics, clozapine (40 mg/kg), nemonapride (0.01–2.5 mg/kg), ziprasidone (10 mg/kg), and aripiprazole (0.01 and 10 mg/kg), which all exhibit 5-HT1A agonist properties, reversed PPI deficits at some doses only, whereas the anti-dyskinetic agent sarizotan (0.16–10 mg/kg), an efficacious 5-HT1A agonist, did not. New generation antipsychotics with marked 5-HT1A agonist properties, such as SLV313 and SSR181507 (0.0025–10 mg/kg and 0.16–10 mg/kg, respectively) did not reverse these deficits whereas bifeprunox (0.04–2.5 mg/kg) did. To reveal the contribution of 5-HT1A agonist properties in the lack of effects of SLV313 and SSR181507, we pretreated rats with the 5-HT1A antagonist WAY100635 (0.63 mg/kg). Under these conditions, significant reversal of PPI deficit was observed, indicating that D2 antagonist properties of SLV313 and SSR181507 are now sufficient to overcome the disruptive effects of apomorphine. To summarize, antipsychotics possessing agonist efficacy at 5-HT1A receptors exhibit diverse profiles against apomorphine-induced PPI deficits, depending on the balance between D2 and 5-HT1A activities, suggesting that they may display distinct activity on some aspects of gating deficits in schizophrenic patients.
Similar content being viewed by others
INTRODUCTION
Several neuropsychiatric disorders, such as schizophrenia, are associated with deficits in sensorimotor gating, and the prepulse inhibition (PPI) model of the acoustic startle reflex was developed in rodents to mimic these deficits (Geyer and Braff, 1987; Braff and Geyer, 1990, 2001). PPI is defined as the attenuation of the response to a startling stimulus (pulse), when such a stimulus is briefly preceded by a stimulus of subthreshold intensity (prepulse). PPI can be disrupted by acting on developmental and environmental factors such as isolation rearing of rats (Geyer et al, 1993; Varty et al, 1999), early maternal or nutritional deprivation (Ellenbroek et al, 1998), and neonatal lesions of neuronal circuitry linking the limbic structures and basal ganglia (Lipska et al, 1995). However, the pharmacological disruption approach, for reasons of ease of implementation, is more commonly used. Among the three main pharmacological models of disruption of PPI in rats, that is, those induced by dopamine (DA) receptor agonists, 5-HT2A receptor agonists, and NMDA/glutamate receptor antagonists, the DA receptor agonist-induced PPI deficit model appears to be the best-validated for the identification of antipsychotics with DA D2 receptor blocking properties. Indeed, PPI can be disrupted by either direct DA receptor agonists, such as apomorphine, or indirect DA agonists that facilitate dopaminergic transmission, such as d-amphetamine, and these effects can be prevented by DA D2 (and/or D1) receptor antagonists (Swerdlow et al, 1986, 1994; Mansbach et al, 1988). Hence, antipsychotics that have appreciable affinity for DA D2 receptors such as haloperidol, reliably prevent apomorphine-induced deficits in rats (Mansbach et al, 1988; Geyer et al, 2001; Ralph and Caine, 2005).
All current antipsychotics have more or less marked DA D2 receptor antagonists properties, thought to be responsible for their efficacy, at least against positive symptoms (Kapur and Remington, 2001; Wadenberg et al, 2000b). Another major monoaminergic system, the serotonergic system, has also been implicated in various aspects of the neurobiology of schizophrenia. Two subtypes of serotonin receptors, the 5-HT2 and the 5-HT1A, have been the objects of great interest. As a matter of fact, most atypical antipsychotics are DA D2 and 5-HT2 receptors blockers, and it has been proposed that antagonist activity at 5-HT2 receptors prevents the deleterious effects of DA D2 receptor blockade, that is, extrapyramidal signs (EPS) (Kapur, 1996; Remington and Kapur, 1999). Besides, there is ample pre-clinical evidence that activation of 5-HT1A receptors should also prove beneficial in schizophrenia (Millan, 2000; Bantick et al, 2001; Ichikawa et al, 2001). Hence, it has been repeatedly shown that 5-HT1A receptor agonists prevent catalepsy (an animal model of EPS) produced by blockade of DA D2 receptors (Wadenberg and Ahlenius, 1991; Wadenberg et al, 1994; Neal-Beliveau et al, 1993; Prinssen et al, 1998, 1999; Depoortere et al, 2003; Kleven et al, 2005). Consistent with this idea, clinical studies have reported that buspirone and tandospirone, two partial agonists at 5-HT1A receptors, reduce the incidence of EPS in schizophrenic patients treated with haloperidol (Sumiyoshi et al, 2001a, 2001b). Furthermore, these studies have also shown that buspirone and tandospirone substantially ameliorate cognitive performance of patients. At the pre-clinical level, microdialysis experiments have shown that 5-HT1A receptor activation increases DA release in prefrontal cortex (Rollema et al, 1997, 2000; Millan et al, 1998; Sprouse et al, 1999; Ichikawa and Meltzer, 2000). In the light of the proposed deficiency in dopaminergic neurotransmission in this brain area in schizophrenic patients, this 5-HT1A receptor-mediated augmentation of cortical DA tone should help in alleviating negative and cognitive deficits of schizophrenia. In addition, 5-HT1A receptor expression is increased in the dorsolateral prefrontal, temporal, and orbital frontal cortices of autopsied brains from chronic schizophrenics (Hashimoto et al, 1991; Simpson et al, 1996; Burnet et al, 1997). Further, PET studies have revealed an increase in cortical 5-HT1A receptor binding in schizophrenia (Kasper et al, 2002).
These considerations have led to the development of compounds with preferential DA D2 receptor antagonist or partial agonist, and 5-HT1A agonist activities, such as bifeprunox (Feenstra et al, 2001; Wolf, 2003), SSR181507 (Claustre et al, 2003; Depoortere et al, 2003; Boulay et al, 2004), SLV313 (Feenstra et al, 2002; McCreary et al, 2002), and sarizotan (that has been re-oriented towards an anti-dyskinetic indication: Bibbiani et al, 2001; Rabiner et al, 2002; Bartoszyk et al, 2004).
However, it has been reported that activation of 5-HT1A receptors by agonists such as 8-OH-DPAT and buspirone, disrupts PPI of the acoustic startle response in rodents (Nanry and Tilson, 1989; Rigdon and Weatherspoon, 1992; Sipes and Geyer, 1994, 1995a; Sipos et al, 2000). Notwithstanding the numerous reports of deleterious effects of 5-HT1A receptor agonists on PPI, activity of mixed DA D2 receptor antagonist/partial agonist and 5-HT1A agonist on models of sensorimotor gating deficits have not been characterized. We therefore examined the ability of such drugs to prevent apomorphine-induced PPI deficits, since the influence of their 5-HT1A agonist properties on sensorimotor gating is unknown. The present study had two objectives: First, to compare the effects of these new compounds with those of older antipsychotic agents (haloperidol, clozapine, ziprasidone, risperidone, olanzapine, aripiprazole, and nemonapride) acting by a variety of mechanisms in addition to/instead of 5-HT1A receptor activation. For the purpose of internal validation, we included the selective 5-HT1A receptor agonist, F13714 (Koek et al, 2001) to verify, under our experimental conditions, the disruptive influence of 5-HT1A receptor activation. Second, to verify that effects of compounds with preferential 5-HT1A receptor agonist properties were specifically mediated through this receptor; to that end, interaction studies with the specific 5-HT1A receptor antagonist WAY100635 were undertaken whenever appropriate.
MATERIALS AND METHODS
Animals
Male Sprague–Dawley rats (ICO: OFA SD, Iffa Credo, Les Oncins, France), weighing 180±20 g upon arrival were group-housed (n=5/cage) in an environmentally controlled room (temperature 21±1°C and relative humidity 55±5%) on a 12 h : 12 h light : dark cycle (lights on at 0700), in stainless steel cages with grid flooring (internal dimensions: 26 × 42 × 18 cm; W × L × H). Animals were held in quarantine for 4–8 days, with free access to standard laboratory food (A04, Scientific Animal Food and Engineering, Epinay sur Orge, France) and filtered water (0.22 μm pores; in bottles). A 5-day acclimatization period was allowed before animals were used in experiments. Twenty-four hours before testing, the animals were individually housed in an environmentally controlled test room in plastic hanging cages with a grid floor (internal dimensions: 11 × 31 × 18 cm; W × L × H), where they had free access to water, but not food. Animals were handled and cared for in accordance with the ‘Guide and Care and Use of Laboratory Animals (National Institutes of Health) and the European Directive 86/609, and was carried out in compliance with French regulations and the local ethical committee guidelines for animal research.
Apparatus
Startle chambers (SR LAB, San Diego Instruments, San Diego, CA) were used. Each chamber consisted of a transparent acrylic cylinder (inside diameter: 8.8 cm; inside length: 18.4 cm), resting on a Plexiglas base in a sound-attenuated ventilated enclosure illuminated by a 15 W lamp. Pulses and pre-pulses (white noise bursts) were presented via a loudspeaker mounted 28 cm above the animal. Startle reflexes within the cylinder were detected by a piezoelectric accelerometer attached to the base. Response sensitivities were calibrated using a standard calibrator tube (San Diego Instruments), and were adjusted to 150 units. Sound levels were calibrated (±1 dB) using the A scale of a sound level meter (Radio Shack, Tandy Corp., Fort Worth, TX). All events were controlled and recorded on a PC using the San Diego Instruments Startle software.
Procedure
Pre-test and test sessions
Animals, which were used only once, were pre-tested in startle chambers 1 h 45 min before the pharmacological challenge (test) session. This pre-test session that lasted 13 min, was used to habituate rats to the procedure. Three different trial types were presented against a continuous 70 dB background noise: no pulse (NP), 118 dB pulse (pulse alone; PA), and 78 dB prepulse (pp) followed by a 118 dB pulse (prepulse-pulse; ppP). The PA and P duration was 40 ms, the pp duration 20 ms, and the interval between the end of the pp and the onset of the PA or P 80 ms. Sessions started with a 5-min adaptation period after which the animals were exposed to 10 PA (included to induce habituation to startle, such that habituation during the following PPI assessment would be minimized: these trials were not used for data analysis). These 10 PA trials were followed by 10 PA, 10 ppP, and 3 NP trials presented in a pseudo-random order. The interval between trials was variable but with a median of 15 s. The startle response was defined as the average amplitude measured during 100 consecutive samples of 1 ms, which were recorded from the onset of the pulse by means of a 12-bit AD acquisition card (range: 0–4095 arbitrary units). Rats were returned to their home cages at the end of the pre-test session.
Test sessions were in all respects similar to the pre-test sessions (vide supra). Rats that showed any one of these four criteria at least once during either the pre-test or test session were not retained for data analysis: (i) an amplitude of the startle reflex following presentation of the PA less than 10 arbitrary units, or (ii) more than four amplitudes for PA equal to 4095 (ceiling value of the 12-bits AD acquisition card) for the PA condition or for the ppP condition, or (iii) a (PA-NP) amplitude/PA amplitude <80% or (iv) a pp amplitude>PA amplitude (this last elimination criterion was used only for the pre-test session).
Pharmacological treatments
At the end of the pre-test session, animals were treated as follows: for the dose-effect study of apomorphine and F13714, animals were injected s.c. 60 min before the beginning of the test session with vehicle, and 45 min later with apomorphine or F13714. For the reversion of the apomorphine-induced PPI deficits with antipsychotics, animals were injected 60 min before with the test compound or its vehicle, and 45 min later with apomorphine. For the interaction of the 5-HT1A antagonist and SLV313 or SSR181507, WAY100635 or its vehicle was injected s.c. 75 min before the beginning of the test session, followed by the injection protocol described right above. The dose of apomorphine used in double and triple treatments was 0.63 mg/kg. After each injection, the animals were put back in their home cages. Following is a schematic of the injection protocol:

Data Analysis
For each test session, the median of the amplitude of the startle responses for the last 10 PA trials and for the 10 ppP was calculated. The percentage PPI was calculated as follows:

Data (percentage PPI) were analyzed with an one-way ANOVA with the treatment as the between-subjects factor, followed by a Dunnett's post hoc test for comparison with the saline/saline group (for the apomorphine and F13714 dose–response study) or the saline/apomorphine group (for the apomorphine/antipsychotics interaction experiments). For the experiments on the interaction between WAY100635 and SLV313 or SSR181507, a non-parametric (Kruskal–Wallis) test was used (due to heterogeneity of variance) to compare the saline/test compound/apomorphine groups to the WAY100635/test compound/apomorphine groups. It was followed by a Dunn's post hoc test for comparing pretreatment with saline or WAY100635 for selected doses of test compounds.
Drugs
Haloperidol, clozapine, and apomorphine HCl were obtained commercially (Sigma RBI, St Quentin Fallavier, France). Ziprasidone HCl, aripiprazole, bifeprunox mesylate (DU-127090; N-[4-[(3-chloro-4-fluorophenyl)amino]-7-[3-(morpholin-4-yl)propoxy]quinazolin-6-yl]prop-2-enamide mesylate), SSR181507 HCl ((3-exo)-8-benzoyl-N-[[(2S)7-chloro-2,3-dihydro-1,4-benzodioxin-1-yl]methyl]-8-azabicyclo[3.2.1]octane-3-methanamine monohydrochloride), sarizotan HCl (EMD-128130; (-)-3-[[[(R)-2-chromanylmethyl]amino]methyl]-5-(p-fluorophenyl)pyridine monohydrochloride), risperidone, olanzapine, nemonapride, F13714 (3-chloro-4-fluorophenyl-(4-fluoro-4-{[(5-methyl-6-methylamino-pyridin-2-ylmethyl)-amino]-methyl}-piperidin-1-yl-methanone fumaric acid salt) and WAY100635 (N-[2-[4-(2-methoxyphenyl)-1-piperazinyl]-N-(2-pyridinyl)cyclohexanecarboxamide) were synthesized by J-L Maurel at the Centre de Recherche Pierre Fabre (Castres, France). SLV313 HCl (piperazine, 1-(2,3-dihydro-1,4-benzodioxin-5-yl)-4-[[5-(4-fluorophenyl)-3-pyridinyl]methyl) was generously donated by Solvay Pharmaceuticals (Weesp, The Netherlands). SSR181507 (0.16–10 mg/kg), F13714 (0.0025–10 mg/kg), apomorphine (0.04–2.5 mg/kg), and WAY100635 (0.63 mg/kg) were prepared in distilled water and administered s.c., whereas aripiprazole (0.01–10 mg/kg), bifeprunox (0.01–40 mg/kg), sarizotan (0.16–10 mg/kg), and ziprasidone (0.04–10 mg/kg) were prepared as a suspension in aqueous Tween 80 (two drops/10 ml distilled water) and administered i.p. SLV313 (0.0025–10 mg/kg), nemonapride (0.00063–2.5 mg/kg), olanzapine (0.16–40 mg/kg), risperidone (0.04–10 mg/kg), clozapine (2.5–40 mg/kg), and haloperidol (0.01–2.5 mg/kg) were prepared in distilled water with a drop of lactic acid, after which the pH was adjusted to 5–7 with a 1 N solution of sodium hydroxide, and were injected s.c. (except clozapine: i.p.). An injection volume of 10 ml/kg was used throughout and doses refer to the weight of the free base. For each compound, doses were administered in an unsystematic order.
RESULTS
Disruptive Effects on PPI of a Direct DA Receptor Agonist and a 5-HT1A Receptor Agonist
Apomorphine (Figure 1a) significantly disrupted PPI at doses of 0.63 and 2.5 mg/kg in comparison with saline (F(4,143)=25.76, p<0.0001, Dunnett's post hoc test: p<0.01 for both doses). Similarly, F13714 (Figure 1b) disrupted PPI in comparison with saline (F(6,66)=25.89, p<0.0001, Dunnett's post hoc test: <p<0.01 at doses from 0.04 to 2.5 mg/kg).
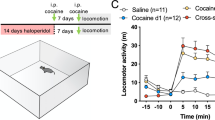
Dose–response curves of the disruption of PPI induced by apomorphine (panel a) or by F13714 (panel b). Rats were injected 60 min before testing with vehicle, followed 45 min after by apomorphine or F13714 or vehicle. The percentage PPI was calculated as: [(median PA amplitude – median ppP amplitude) × 100]/(median PA amplitude). Symbols are means±SEM. Data were analyzed using one-way ANOVA's followed by Dunnett's post hoc tests. **p<0.01, compared with the vehicle/vehicle control group. N=7–9 rats per dose.
Reversal of Apomorphine-Induced PPI Deficits by Antipsychotics with Marked D2 Antagonist Properties and Devoid of 5-HT1A Agonist Activity
Haloperidol (0.63 and 2.5 mg/kg) significantly reversed the disruption of PPI induced by apomorphine (0.63 mg/kg, s.c.) (F(5,198)=8.19, p<0.0001, Dunnett's post hoc test: p<0.01: Figure 2a). Similar significant effects were obtained for olanzapine (Figure 2b) at 0.63, 10, and 40 mg/kg (F(5,197)=7.68, p<0.0001, Dunnett's post hoc test: p<0.05, p<0.01, and p<0.01, respectively) and for risperidone (Figure 2c) at 0.63, 2.5, and 10 mg/kg (F(5,197)=10.36, p<0.0001, Dunnett's post hoc test: p<0.01, p<0.05, and p<0.01, respectively).
Effects of haloperidol (panel a), olanzapine (panel b) and risperidone (panel c) on the disruption of PPI induced by apomorphine. Rats were injected with vehicle or test compounds 60 min before testing, followed 45 min later by apomorphine (0.63 mg/kg, s.c.). See legend of Figure 1 for details. *p<0.05 and **p<0.01, compared with the vehicle/apomorphine control group, following significant one-way ANOVA. N=9 rats per dose.
Effects on Apomorphine-Induced PPI Deficits of Multireceptorial Antipsychotics Possessing Some 5-HT1A Agonist Properties
Clozapine (40 mg/kg) (F(3,181)=6.44, p<0.001, Dunnett's post hoc test p<0.01), ziprasidone (10 mg/kg) (F(5,196)=3.387, p<0.01, Dunnett's post hoc test p<0.05), and aripiprazole (0.04 and 10 mg/kg) (F(6,202)=2.620, p<0.05, Dunnett's post hoc test p<0.05) significantly reversed the deficits of PPI (Figure 3a–c). Over a wider range of doses, nemonapride (0.01–2.5 mg/kg: Figure 3d) significantly prevented the disruption of PPI (F(7,213)=5.37, p<0.0001, Dunnett's post hoc test for 0.01 mg/kg: p<0.05, for 0.04 mg/kg: p<0.05, for 0.16 mg/kg: p<0.05, for 0.63 mg/kg: p<0.01, for 2.5 mg/kg: p<0.05).
Effects of clozapine (panel a), ziprasidone (panel b), aripiprazole (panel c) and nemonapride (panel d) on the disruption of PPI induced by apomorphine. Rats were injected with vehicle or test compounds 60 min before testing, followed 45 min later by apomorphine (0.63 mg/kg, s.c.). See legend of Figure 1 for details, and legend of Figure 2 for statistical analysis. N=9 rats per dose.
Effects on Apomorphine-Induced PPI Deficits of Novel Putative Antipsychotics Selectively Targeting D2 and 5-HT1A Receptors
Deficits induced by apomorphine were not significantly reversed by SSR181507 (F(4,189)=1.64, p=0.16) or sarizotan (F(4,189)=0.43, p=0.79) (Figure 4a and b). For SLV313, although there was a significant global effect of the ANOVA (F(7,213)=2.38, p=0.02: Figure 4c), post hoc Dunnett's test did not detect any dose that differed significantly from control. In contrast, bifeprunox (0.04–2.5 mg/kg: Figure 4d) prevented PPI deficits (F(7,213)=6.83, p<0.0001, Dunnett's post hoc test: for 0.04 mg/kg: p<0.01, for 0.16 mg/kg: p<0.05, for 0.63 mg/kg: p<0.01, for 2.5 mg/kg: p<0.01). For the higher doses of 10 and 40 mg/kg, bifeprunox did not significantly reverse the effects of apomorphine (p>0.05).
Effects of SSR181507 (panel a), SLV313 (panel b), sarizotan (panel c) and bifeprunox (panel d) on the disruption of PPI induced by apomorphine. Rats were injected with vehicle or test compounds 60 min before testing, followed 45 min later by apomorphine (0.63 mg/kg, s.c.). See legend of Figure 1 for details, and legend of Figure 2 for statistical analysis. N=9 rats per dose.
Masking by Pretreatment with WAY100635 of the 5-HT1A Agonist Properties of SLV313 and SSR181507: Effects on Apomorphine-Induced PPI Deficits
By blocking the 5-HT1A agonist properties of SLV313 (Figure 5a) and SSR181507 (Figure 5b), WAY100635 (0.63 mg/kg) permitted the reversal of PPI deficits induced by apomorphine. PPI deficits were opposed by 0.01, 2.5, and 10 mg/kg of SLV313 (Kruskal–Wallis test: H=43.44, p<0.0001, Dunn's post hoc test: p<0.05 for all three doses) and by 10 mg/kg of SSR181507 (Kruskal–Wallis test: H=21.74, p<0.01, Dunn's post hoc test: p<0.01).
Pretreatment with the 5-HT1A receptor antagonist WAY100635 reveals the ability of SLV313 (panel a) or SSR181507 (panel b) to reverse the disruption of PPI induced by apomorphine. Rats were injected with vehicle or WAY100635 (0.63 mg/kg, s.c.), vehicle or test compound, followed by apomorphine (0.63 mg/kg, s.c.), 75 min, 60 min and 15 min, respectively, before testing. Data were analyzed using non-parametric Kruskal–Wallis tests followed by a Dunn's post-hoc tests. *p<0.05 and **p<0.01, comparing the WAY100635 pretreated with the saline-pretreated group, at the considered dose of the test compound. See legend of Figure 1 for details. N=9 rats per dose.
Note: effects of compounds on PPI and on pulse alone (PA) amplitude did not appear to be correlated. Table 1 contains a non-exhaustive list of a series of drug treatments, with their effects on PA amplitude and on %PPI. It can be seen that some treatments increased the PA amplitude but decreased the %PPI (first line), while others did not modify the PA amplitude but increased the %PPI (second line), diminished the PA amplitude but augmented (third line) or left intact (fourth line) the %PPI, and finally increased both the PA amplitude and the %PPI (fifth line).
DISCUSSION
The PPI paradigm employed in the present study is widely used for characterizing antipsychotic drugs, and has been claimed to possess face validity, since apomorphine-induced startle gating deficits in rats mimic the abnormalities of gating that are thought to underlie sensory flooding and cognitive fragmentation present in schizophrenic patients (McGhie and Chapman, 1961; Braff et al, 2001). These deficits can be reversed by ‘typical’ high-potency DA D2 receptor antagonists and ‘atypical’ antipsychotics with low activity at 5-HT1A receptors (Swerdlow et al, 1986, 1994; Mansbach et al, 1988; Geyer et al, 2001). However, activation of 5-HT receptor subtypes, such as 5-HT2A and 5-HT1A interferes with sensorimotor gating (Mansbach et al, 1988; Nanry and Tilson, 1989; Rigdon and Weatherspoon, 1992; Sipes and Geyer, 1994, 1995a, 1995b, 1997; Sipos et al, 2000; Wadenberg et al, 2000a; Roth et al, 2004). As such, the exploration of activity of drugs acting preferentially at DA D2 and 5-HT1A receptors (currently under development as antipsychotics) in the apomorphine-PPI model was warranted. The present data show that a wide diversity of responses is observed among these novel compounds (including SSR181507, bifeprunox, SLV313, and sarizotan), which distinguishes them from existing classes of conventional and ‘atypical’ antipsychotics.
Antipsychotics with Marked DA D2 Antagonist But Devoid of 5-HT1A Agonism Properties
Over a broad range of doses (0.63–10 mg/kg or 40 mg/kg), haloperidol, risperidone, and olanzapine prevented the PPI disruptive effects of apomorphine, confirming previous data (Mansbach et al, 1988; Geyer et al, 1990; Schwarzkopf et al, 1993; Rasmussen et al, 1997). These antipsychotics behave as DA D2 receptor antagonists, with low or no affinity at 5-HT1A receptors (Newman-Tancredi et al, 1998; Leysen, 2005). Indeed, the ratios of Ki (rKi) at 5-HT1A vs DA D2 receptors were 275, 468, and 1738, for olanzapine, risperidone, and haloperidol, respectively (Newman-Tancredi et al, 2005). Considering that disruption of PPI by the DA receptor agonist apomorphine has been demonstrated to result primarily by activation of DA D2 receptors in rats (Swerdlow et al, 1986; Mansbach et al, 1988; Geyer et al, 2001), the reversion observed with these three compounds is consistent with their receptorial profile.
‘Atypical’ Antipsychotics Possessing, Among Other Properties, 5-HT1A Agonist Activities
Clozapine at the highest dose tested (40 mg/kg) reversed the reduction of PPI induced by apomorphine, confirming previous results for this ‘atypical’ antipsychotic (Swerdlow et al, 1991, 1998; Mansbach et al, 1998). This reversing effect can be explained based on a low efficacy at 5-HT1A receptors (12% that of (+)8-OH-DPAT in an assay of [35S]GTPγS stimulation in rat hippocampal membrane: Newman-Tancredi et al, 2005) combined with a rather low pKi (3.3). The low potency of clozapine is consistent with its very moderate affinity for the DA D2 receptor (pKi: 6.31: Newman-Tancredi et al, 2005). In contrast, nemonapride almost completely prevented PPI deficits over a dose-range of 0.01–2.5 mg/kg. Here again, the rKi was high (37), indicating that over this dose-range, DA D2 receptor blockade largely predominates over the agonist activity at 5-HT1A receptors. Its rather potent efficacy to activate 5-HT1A receptors (39% that of (+)8-OH-DPAT in an assay of [35S]GTPγS stimulation in rat hippocampal membrane: Newman-Tancredi et al, 2005) might explain why the reversing effect is not full at higher doses. Indeed, in a catalepsy test, it was observed that nemonapride produced catalepsy at lower doses (0.04–0.63 mg/kg s.c.) but not at higher doses (from 2.5 to 40 mg/kg s.c.), indicating that the 5-HT1A agonist properties of nemonapride appear at doses approximately 16–64 fold higher than those blocking DA D2 receptors (Prinssen et al, 1998).
The 5-HT1A receptor partial agonist/DA D2 receptor antagonist ziprasidone, and the DA D2 receptor and 5-HT1A receptor partial agonist aripiprazole, reversed apomorphine-induced PPI deficits at some doses only (10 mg/kg, and 0.16 and 10 mg/kg, respectively). Similar results (partial reversal) were obtained by Mansbach et al (2001) with 17 mg/kg (p.o.) of ziprasidone in Wistar rats. As concerns aripiprazole, we believe we are the first group to provide data concerning its actions in this model of sensorimotor gating deficit. The partial reversal seen with ziprazidone might be tentatively explained by a rKi lower than unity (0.4), and a somewhat potent efficacy at 5-HT1A receptors (31 % that of (+)8-OH-DPAT). A similar explanation would be less applicable to aripiprazole: the compound has a rKi of 15, and an efficacy at 5-HT1A receptors of 22%. However, it behaves as a DA D2 receptor partial agonist (efficacy: 26% that of apomorphine in an assay of [35S]GTPγS stimulation in membrane from Sf9 cells expressing the human D2L receptor: (Cosi et al, in press). As a consequence, the partial agonist activity at DA D2 receptors at low doses is relayed by the 5-HT1A receptor partial agonist properties at higher doses, resulting in a lack of clear-cut reversing effect. In addition, in both rats and humans, a major metabolite of aripiprazole is a pure DA D2 receptor antagonist (Lawler et al, 1999), which adds a further dimension to the complexity of pharmacological interaction between apomorphine and aripiprazole in this test.
Influence of 5-HT1A Receptor Agonism on the Ability of Novel Antipsychotics Selectively Targeting DA D2 and 5-HT1A Receptors to Reverse Apomorphine-Induced PPI Deficits
Neither SSR181507, SLV313 nor sarizotan reversed apomorphine-induced PPI deficits. All three compounds are characterized by their strong affinity for and fairly high efficacy at 5-HT1A receptors (Newman-Tancredi et al, 2005). These data are consistent with the disruptive influence of the selective 5-HT1A agonist, F13714 (Figure 1b), and of the prototypic 5-HT1A agonist, 8-OH-DPAT, as well as the partial 5-HT1A agonists, buspirone, gepirone, and ipsapirone (Rigdon and Weatherspoon, 1992; Sipes and Geyer, 1995a; Sipos et al, 2000). Among a whole series of compounds tested (Newman-Tancredi et al, 2005), sarizotan exhibited the highest efficacy at 5-HT1A receptors (100% that of (+)8-OH-DPAT), and possessed a low rKi (0.3). Furthermore, sarizotan behaved as a partial DA D2 receptor agonist (Bartoszyk et al, 2004; Kuzhikandathil et al, 2004). These observations indicate that the 5HT1A receptor agonist properties of sarizotan are predominant: this most likely explains the lack of activity of this compound against apomorphine-induced PPI disruption, and might also be the reason why it was originally developed as an antipsychotic, but has been more recently re-oriented towards an anti-dyskinetic indication (Bibbiani et al, 2001). SSR181507 exhibited a moderate efficacy at 5-HT1A receptors (39% that of (+)8-OH-DPAT) with a rKi of 0.8, and also behaved as a partial DA D2 receptor agonist (18% that of apomorphine, Cosi et al, in press). Here again, it can be considered that the compound preferentially activates 5-HT1A receptors, hence its lack of activity against apomorphine-induced PPI impairment. The case for SLV313 is slightly different: despite the fact that it had even more moderate efficacy at 5-HT1A receptors (28% that of (+)8-OH-DPAT), its rKi was also close to unity (0.9: Newman-Tancredi et al, 2005) but it behaved as a DA D2 receptor antagonist (Feenstra et al, 2002; McCreary et al, 2002; Cosi et al, in press). Nonetheless, it seems that overall, its 5-HT1A receptor agonist activity predominates. It should be noted, however, that in the only other study (in an abstract form) published on SLV313, it was reported that the compound could attenuate effect of PPI disruption at doses less than 0.1 mg/kg (McCreary et al, 2002). The reasons for this discrepancy between this study and ours are not clear at the moment. Administration of the 5-HT1A receptor antagonist WAY-100635 revealed the ability of SSR181507 and SLV313 to prevent apomorphine-induced PPI deficits. This provides a cogent demonstration implicating the 5-HT1A receptor agonist activity of these compounds in their lack of efficacy for reversal of this type of disruption.
Surprisingly, bifeprunox potently prevented apomorphine-induced gating deficits at doses from 0.04 to 2.5 mg/kg, with a loss of activity at 10 and 40 mg/kg. One possible explanation is that bifeprunox, although having a quite substantial efficacy at 5-HT1A receptors (54% that of (+)8-OH-DPAT), has higher affinity for D2 than for 5-HT1A receptors (rKi of 44). It thus appears that the partial agonist activity at DA D2 receptors (27% that of apomorphine, Cosi et al, in press) predominates over this dose-range, and reverses the deficit produced by the full D2 receptor agonist apomorphine whereas at higher doses (10 and 40 mg/kg), the 5-HT1A agonist activity exerts its deleterious effects on PPI.
SUMMARY AND CONCLUSIONS
Although several novel antipsychotics share the capacity to interact at both 5-HT1A and DA D2 receptors, their ability to reverse apomorphine-induced PPI deficits is highly diverse. In fact, this variety of profiles could be related to their diverging affinities and efficacies at 5-HT1A and DA D2 receptors, as has been characterized in detail in cellular models of receptor interaction (Newman-Tancredi et al, 2005, Cosi et al, in press). Thus, the present data suggest that in this apomorphine-induced gating deficits model, a narrow window of efficacy exists between DA D2 receptor blockade and serotonin 5-HT1A receptor activation. While the latter property is considered to be desirable for attenuating negative, cognitive, and affective symptoms of schizophrenia, as well as neuroleptic-induced EPS (Millan, 2000; Bantick et al, 2001; Kleven et al, 2005), it appears that too pronounced an activation of 5-HT1A receptors impairs the ability of compounds, such as SLV313 and SSR181507 to reverse apomorphine-induced PPI deficits. Taken together, these data indicate that 5-HT1A activation can alter the antipsychotic-like effects of DA D2 receptor antagonists in this model of positive symptoms of schizophrenia. However, this does not hold true for at least one other model predictive of antipsychotic activity, such as the active (two-way) avoidance task: in mice, the coadministration of the 5-HT1A antagonist SL88.0338 did not modify the activity of SSR181507 in this test (Depoortere et al, 2003). In addition, data obtained in the same test but in rats, suggest that the potency of DA D2 receptor antagonists (such as raclopride and haloperidol) is even enhanced by addition of a compound with 5-HT1A agonist properties such as 8-OH-DPAT (Prinssen et al, 1996).
Taken together, these considerations indicate complex interactions in the balance of DA D2 and 5-HT1A activities that could profoundly influence the pharmacological and therapeutic profiles of new generation ligands targeting these receptors.
References
Bantick RA, Deakin JF, Grasby PM (2001). The 5-HT1A receptor in schizophrenia: a promising target for novel atypical neuroleptics? J Psychopharmacol 15: 37–46.
Bartoszyk GD, Van Amsterdam C, Greiner HE, Rautenberg W, Russ H, Seyfried CA (2004). Sarizotan, a serotonin 5-HT1A receptor agonist and dopamine receptor ligand. 1. Neurochemical profile. J Neural Transm 111: 113–126.
Bibbiani F, Oh JD, Chase TN (2001). Serotonin 5-HT1A agonist improves motor complications in rodent and primate parkinsonian models. Neurology 57: 1829–1834.
Boulay D, Depoortere R, Louis C, Perrault G, Griebel G, Soubrie P (2004). SSR181507, a putative atypical antipsychotic with dopamine D2 antagonist and 5-HT1A agonist activities: improvement of social interaction deficits induced by phencyclidine in rats. Neuropharmacology 46: 1121–1129.
Braff DL, Geyer MA (1990). Sensorimotor gating and schizophrenia. Human and animal model studies. Arch Gen Psychiatry 47: 181–188.
Braff DL, Geyer MA, Light GA, Sprock J, Perry W, Cadenhead KS et al (2001). Impact of prepulse characteristics on the detection of sensorimotor gating deficits in schizophrenia. Schizophr Res 49: 171–178.
Burnet PW, Eastwood SL, Harrison PJ (1997). [3H]WAY-100635 for 5-HT1A receptor autoradiography in human brain: a comparison with [3H]8-OH-DPAT and demonstration of increased binding in the frontal cortex in schizophrenia. Neurochem Int 30: 565–574.
Claustre Y, Peretti DD, Brun P, Gueudet C, Allouard N, Alonso R et al (2003). SSR181507, a dopamine D2 receptor antagonist and 5-HT1A receptor agonist. I: Neurochemical and electrophysiological profile. Neuropsychopharmacology 28: 2064–2076.
Cosi C, Carilla-Durand E, Assié MB, Ormière AM, Maraval M, Leduc N et al. Partial agonism of the antipsychotics SSR181507, aripiprazole and bifeprunox at D2 receptors: G-protein activation and prolactin release. Eur J Pharmacol (in press).
Depoortere R, Boulay D, Perrault G, Bergis O, Decobert M, Francon D et al (2003). SSR181507, a dopamine D2 receptor antagonist and 5-HT1A receptor agonist. II: Behavioral profile predictive of an atypical antipsychotic activity. Neuropsychopharmacology 28: 1889–1902.
Ellenbroek BA, van den Kroonenberg PT, Cools AR (1998). The effects of an early stressful life event on sensorimotor gating in adult rats. Schizophr Res 30: 251–260.
Feenstra RW, de Moes J, Hofma JJ, Kling H, Kuipers W, Long SK et al (2001). New 1-aryl-4-(biarylmethylene)piperazines as potential atypical antipsychotics sharing dopamine D2-receptor and serotonin 5-HT1A-receptor affinities. Bioorg Med Chem Lett 11: 2345–2349.
Feenstra RW, Long SK, Kuipers W, van der Heyden JA, Tulp MT, Kruse CG (2002). New approaches for psychosis treatment: design, synthesis and SAR of ligands binding to dopamine D2 and serotonin 5-HT1A receptors. Drugs of the future. XVIIth International Symposium on Medicinal Chemistry 27(Suppl A): P237.
Geyer MA, Braff DL (1987). Startle habituation and sensorimotor gating in schizophrenia and related animal models. Schizophr Bull 13: 643–668.
Geyer MA, Krebs-Thomson K, Braff DL, Swerdlow NR (2001). Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: a decade in review. Psychopharmacology 156: 117–154.
Geyer MA, Swerdlow NR, Mansbach RS, Braff DL (1990). Startle response models of sensorimotor gating and habituation deficits in schizophrenia. Brain Res Bull 25: 485–498.
Geyer MA, Wilkinson LS, Humby T, Robbins TW (1993). Isolation rearing of rats produces a deficit in prepulse inhibition of acoustic startle similar to that in schizophrenia. Biol Psychiatry 34: 361–372.
Hashimoto T, Nishino N, Nakai H, Tanaka C (1991). Increase in serotonin 5-HT1A receptors in prefrontal and temporal cortices of brains from patients with chronic schizophrenia. Life Sci 48: 355–363.
Ichikawa J, Ishii H, Bonaccorso S, Fowler WL, O'Laughlin IA, Meltzer HY (2001). 5-HT2A and D2 receptor blockade increases cortical DA release via 5-HT1A receptor activation: a possible mechanism of atypical antipsychotic-induced cortical dopamine release. J Neurochem 76: 1521–1531.
Ichikawa J, Meltzer HY (2000). The effect of serotonin1A receptor agonism on antipsychotic drug-induced dopamine release in rat striatum and nucleus accumbens. Brain Res 858: 252–263.
Kapur S (1996). 5-HT2 antagonism and EPS benefits: is there a causal connection? Psychopharmacology 124: 35–39.
Kapur S, Remington G (2001). Dopamine D2 receptors and their role in atypical antipsychotic action: still necessary and may even be sufficient. Biol Psychiatry 50: 873–883.
Kasper S, Tauscher J, Willeit M, Stamenkovic M, Neumeister A, Kufferle B et al (2002). Receptor and transporter imaging studies in schizophrenia, depression, bulimia and Tourette's disorder—implications for psychopharmacology. World J Bio Psychiatry 3: 133–146.
Kleven M, Barret-Grévoz C, Bruins Slot L, Newman-Tancredi A (2005). Novel antipsychotic agents with 5-HT1A agonist properties: role of 5-HT1A receptor activation in attenuation of catalepsy induction in rats. Neuropharmacology 49: 135–143.
Koek W, Vacher B, Cosi C, Assie MB, Patoiseau JF, Pauwels PJ et al (2001). 5-HT1A receptor activation and antidepressant-like effects: F 13714 has high efficacy and marked antidepressant potential. Eur J Pharmacol 420: 103–112.
Kuzhikandathil EV, Sayed N, Pasuit JB, Bartoszyk GD (2004). Differential effects of Sarizotan on dopamine receptor function. Society for Neuroscience 163: 6.
Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA et al (1999). Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes. Neuropsychopharmacology 20: 612–627.
Leysen J (2005). Receptor profile of antipsychotics. In: Ellenbroek BA, Cools AR (eds). Atypical Antipsychotics. Birkhaüser Verlag: Basel, Switzerland. pp 57–81.
Lipska BK, Swerdlow NR, Geyer MA, Jaskiw GE, Braff DL, Weinberger DR (1995). Neonatal excitotoxic hippocampal damage in rats causes post-pubertal changes in prepulse inhibition of startle and its disruption by apomorphine. Psychopharmacology 122: 35–43.
Mansbach RS, Brooks EW, Sanner MA, Zorn SH (1998). Selective dopamine D4 receptor antagonists reverse apomorphine-induced blockade of prepulse inhibition. Psychopharmacology 135: 194–200.
Mansbach RS, Carver J, Zorn SH (2001). Blockade of drug-induced deficits in prepulse inhibition of acoustic startle by ziprasidone. Pharmacol Biochem Behav 69: 535–542.
Mansbach RS, Geyer MA, Braff DL (1988). Dopaminergic stimulation disrupts sensorimotor gating in the rat. Psychopharmacology 94: 507–514.
McCreary AC, Glennon J, Tuinstra T, Herremans AHJ, van der Heyden JA, Feenstra RW et al (2002). SLV313: a novel antipsychotic with additional antidepressant and anxiolytic-like actions. Eur Neuropsychopharmacol 12(Suppl 3): P.2.046.
McGhie A, Chapman J (1961). Disorders of attention and perception in early schizophrenia. Br J Med Psychol 34: 103–116.
Millan MJ (2000). Improving the treatment of schizophrenia: focus on serotonin 5-HT1A receptors. J Pharmacol Exp Ther 295: 853–861.
Millan MJ, Brocco M, Veiga S, Cistarelli L, Melon C, Gobert A (1998). WAY 100,635 enhances both the ‘antidepressant’ actions of duloxetine and its influence on dialysate levels of serotonin in frontal cortex. Eur J Pharmacol 341: 165–167.
Nanry KP, Tilson HA (1989). The role of 5-HT1A receptors in the modulation of the acoustic startle reflex in rats. Psychopharmacology 97: 507–513.
Neal-Beliveau BS, Joyce JN, Lucki I (1993). Serotonergic involvement in haloperidol-induced catalepsy. J Pharmacol Exp Ther 265: 207–217.
Newman-Tancredi A, Assie MB, Leduc N, Ormiere AM, Danty N, Cosi C (2005). Novel antipsychotics activate recombinant human and native rat serotonin 5-HT1A receptors: affinity, efficacy and potential implications for treatment of schizophrenia. Int J Neuropsychopharmacol 8: 341–356.
Newman-Tancredi A, Gavaudan S, Conte C, Chaput C, Touzard M, Verriele L et al (1998). Agonist and antagonist actions of antipsychotic agents at 5-HT1A receptors: a [35S]GTPgammaS binding study. Eur J Pharmacol 355: 245–256.
Prinssen EP, Kleven MS, Koek W (1996). Effects of dopamine antagonists in a two-way active avoidance procedure in rats: interactions with 8-OH-DPAT, ritanserin, and prazosin. Psychopharmacology 128: 191–197.
Prinssen EP, Kleven MS, Koek W (1998). The cataleptogenic effects of the neuroleptic nemonapride are attenuated by its 5-HT1A receptor agonist properties. Eur J Pharmacol 356: 189–192.
Prinssen EP, Kleven MS, Koek W (1999). Interactions between neuroleptics and 5-HT1A ligands in preclinical behavioral models for antipsychotic and extrapyramidal effects. Psychopharmacology 144: 20–29.
Rabiner EA, Gunn RN, Wilkins MR, Sedman E, Grasby PM (2002). Evaluation of EMD 128 130 occupancy of the 5-HT1A and the D2 receptor: a human PET study with [11C]WAY-100635 and [11C]raclopride. J Psychopharmacol 16: 195–199.
Ralph RJ, Caine SB (2005). Dopamine D1 and D2 agonist effects on prepulse inhibition and locomotion: comparison of Sprague-Dawley rats to Swiss-Webster, 129X1/SvJ, C57BL/6J, and DBA/2J mice. J Pharmacol Exp Ther 312: 733–741.
Rasmussen K, Gates MR, Burger JE, Czachura JF (1997). The novel atypical antipsychotic olanzapine, but not the CCK-B antagonist LY288513, blocks apomorphine-induced disruption of pre-pulse inhibition. Neurosci Lett 222: 61–64.
Remington G, Kapur S (1999). D2 and 5-HT2 receptor effects of antipsychotics: bridging basic and clinical findings using PET. J Clin Psychiatry 60(Suppl 10): 15–19.
Rigdon GC, Weatherspoon JK (1992). 5-Hydroxytryptamine 1a receptor agonists block prepulse inhibition of acoustic startle reflex. J Pharmacol Exp Ther 263: 486–493.
Rollema H, Lu Y, Schmidt AW, Sprouse JS, Zorn SH (2000). 5-HT1A receptor activation contributes to ziprasidone-induced dopamine release in the rat prefrontal cortex. Biol Psychiatry 48: 229–237.
Rollema H, Lu Y, Schmidt AW, Zorn SH (1997). Clozapine increases dopamine release in prefrontal cortex by 5-HT1A receptor activation. Eur J Pharmacol 338: R3–R5.
Roth BL, Hanizavareh SM, Blum AE (2004). Serotonin receptors represent highly favorable molecular targets for cognitive enhancement in schizophrenia and other disorders. Psychopharmacology 174: 17–24.
Schwarzkopf SB, Bruno JP, Mitra T (1993). Effects of haloperidol and SCH 23390 on acoustic startle and prepulse inhibition under basal and stimulated conditions. Prog Neuropsychopharmacol Biol Psychiatry 17: 1023–1036.
Simpson MD, Lubman DI, Slater P, Deakin JF (1996). Autoradiography with [3H]8-OH-DPAT reveals increases in 5-HT1A receptors in ventral prefrontal cortex in schizophrenia. Biol Psychiatry 39: 919–928.
Sipes TA, Geyer MA (1994). Multiple serotonin receptor subtypes modulate prepulse inhibition of the startle response in rats. Neuropharmacology 33: 441–448.
Sipes TA, Geyer MA (1995a). 8-OH-DPAT disruption of prepulse inhibition in rats: reversal with (+)WAY 100,135 and localization of site of action. Psychopharmacology 117: 41–48.
Sipes TA, Geyer MA (1995b). DOI disruption of prepulse inhibition of startle in the rat is mediated by 5-HT2A and not by 5-HT2C receptors. Behav Pharmacol 6: 839–842.
Sipes TA, Geyer MA (1997). DOI disrupts prepulse inhibition of startle in rats via 5-HT2A receptors in the ventral pallidum. Brain Res 761: 97–104.
Sipos ML, Bauman RA, Widholm JJ, Kant GJ (2000). Behavioral effects of 8-OH-DPAT in chronically stressed male and female rats. Pharmacol Biochem Behav 66: 403–411.
Sprouse JS, Reynolds LS, Braselton JP, Rollema H, Zorn SH (1999). Comparison of the novel antipsychotic ziprasidone with clozapine and olanzapine: inhibition of dorsal raphe cell firing and the role of 5-HT1A receptor activation. Neuropsychopharmacology 21: 622–631.
Sumiyoshi T, Matsui M, Nohara S, Yamashita I, Kurachi M, Sumiyoshi C et al (2001a). Enhancement of cognitive performance in schizophrenia by addition of tandospirone to neuroleptic treatment. Am J Psychiatry 158: 1722–1725.
Sumiyoshi T, Matsui M, Yamashita I, Nohara S, Kurachi M, Uehara T et al (2001b). The effect of tandospirone, a serotonin(1A) agonist, on memory function in schizophrenia. Biol Psychiatry 49: 861–868.
Swerdlow NR, Braff DL, Geyer MA, Koob GF (1986). Central dopamine hyperactivity in rats mimics abnormal acoustic startle response in schizophrenics. Biol Psychiatry 21: 23–33.
Swerdlow NR, Braff DL, Taaid N, Geyer MA (1994). Assessing the validity of an animal model of deficient sensorimotor gating in schizophrenic patients. Arch Gen Psychiatry 51: 139–154.
Swerdlow NR, Keith VA, Braff DL, Geyer MA (1991). Effects of spiperone, raclopride, SCH 23390 and clozapine on apomorphine inhibition of sensorimotor gating of the startle response in the rat. J Pharmacol Exp Ther 256: 530–536.
Swerdlow NR, Varty GB, Geyer MA (1998). Discrepant findings of clozapine effects on prepulse inhibition of startle: is it the route or the rat? Neuropsychopharmacology 18: 50–56.
Varty GB, Braff DL, Geyer MA (1999). Is there a critical developmental ‘window’ for isolation rearing-induced changes in prepulse inhibition of the acoustic startle response? Behav Brain Res 100: 177–183.
Wadenberg MG, Sills TL, Fletcher PJ, Kapur S (2000a). Antipsychotic-like effects of amoxapine, without catalepsy, using the prepulse inhibition of the acoustic startle reflex test in rats. Biol Psychiatry 47: 670–676.
Wadenberg ML, Ahlenius S (1991). Antipsychotic-like profile of combined treatment with raclopride and 8-OH-DPAT in the rat: enhancement of antipsychotic-like effects without catalepsy. J Neural Transm [GenSect] 83: 43–53.
Wadenberg ML, Cortizo L, Ahlenius S (1994). Evidence for specific interactions between 5-HT1A and dopamine D2 receptor mechanisms in the mediation of extrapyramidal motor functions in the rat. Pharmacol Biochem Behav 47: 509–513.
Wadenberg ML, Kapur S, Soliman A, Jones C, Vaccarino F (2000b). Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology 150: 422–429.
Wolf W (2003). DU-127090 Solvay/H Lundbeck. Curr Opin Investig Drugs 4: 72–76.
Acknowledgements
We thank Solvay Pharmaceuticals for supplying SLV313. Alexandra Galinier, Christelle Benas and Catherine Barret-Grevoz are thanked for their expert technical assistance. All authors of this manuscript are employees of the Pierre Fabre Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Auclair, A., Kleven, M., Besnard, J. et al. Actions of Novel Antipsychotic Agents on Apomorphine-Induced PPI Disruption: Influence of Combined Serotonin 5-HT1A Receptor Activation and Dopamine D2 Receptor Blockade. Neuropsychopharmacol 31, 1900–1909 (2006). https://doi.org/10.1038/sj.npp.1301015
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301015
Keywords
This article is cited by
-
The novel dehydroepiandrosterone (DHEA) derivative BNN27 counteracts cognitive deficits induced by the D1/D2 dopaminergic receptor agonist apomorphine in rats
Psychopharmacology (2021)
-
A Natural Product with High Affinity to Sigma and 5-HT7 Receptors as Novel Therapeutic Drug for Negative and Cognitive Symptoms of Schizophrenia
Neurochemical Research (2019)
-
Effects of the monoamine stabilizer (−)-OSU6162 on locomotor and sensorimotor responses predictive of antipsychotic activity
Naunyn-Schmiedeberg's Archives of Pharmacology (2018)
-
1-Aminocyclopropanecarboxylic acid (ACPC) produces procognitive but not antipsychotic-like effects in rats
Psychopharmacology (2015)
-
Co-administration of 5-HT6 receptor antagonists with clozapine, risperidone, and a 5-HT2A receptor antagonist: effects on prepulse inhibition in rats
Psychopharmacology (2014)