Abstract
The serotonergic hypothesis for depression in Parkinson's disease (PD) states that the reduced cerebral serotonergic activity that occurs in PD constitutes a biological risk factor for depression. The aim of our study was to assess the serotonergic hypothesis of depression in PD patients using an experimental approach. In a double-blind, randomized order, placebo-controlled crossover design, the response on the Profile of Mood States (POMS) questionnaire to acute tryptophan depletion (ATD) was studied in 15 PD nondepressed patients and 15 control subjects, without a prior personal or family history of depression. PD patients had lower (worse) baseline scores on the sadness, fatigue and vigor subscales of the POMS, in both ATD and the placebo condition, but not on the tension and anger subscales. There was however neither a significe between group effect, nor significe within-group effect due to ATD. We could find no evidence of a specific serotonergic vulnerability of PD patients for depression. Therefore, our results do not support the serotonergic hypothesis for depression in PD.
Similar content being viewed by others
INTRODUCTION
Mood disturbance, and especially major depressive disorder, is a common condition in Parkinson's disease (PD), with an average prevalence of 25–40% in outpatient settings (Leentjens, 2004). Depression is associated with a reduced quality of life, increased functional disability, more severe cognitive symptoms, and enhanced caregiver's stress (Troster et al, 1995; Liu et al, 1997; Aarsland, 1999; Hobson et al, 1999). Although there is some knowledge about risk factors associated with depression in PD, little is known about its pathophysiology. The serotonergic hypothesis is one of the few hypotheses that have tried to link the pathophysiology of PD with an increased risk of depression (Mayeux, 1990). This hypothesis is based on three observations. The first is that serotonergic activity is reduced in PD. Indeed, degeneration of serotonergic nerve cells, decreased brain serotonin content, and alterations in the activities of various types of serotonin receptors, have all been demonstrated in post-mortem studies using neurochemical and autoradiographic techniques (Jellinger, 1991) (Scatton et al, 1983; Chen et al, 1998). Moreover, in vivo studies have consistently demonstrated reduced levels of 5-hydroxyindoleacetic acid (5-HIAA), a breakdown product of serotonin, in the cerebrospinal fluid (CSF) of PD patients (Johanson and Roos, 1967; Kuhn et al, 1996), with some studies reporting an additional reduction of 5-HIAA in depressed PD patients (Mayeux et al, 1984; Kostic et al, 1987). These findings show the involvement of serotonin in PD. The second observation is the finding in animal studies that serotonin has the ability to inhibit striatal dopamine release (Gerson and Baldessarini, 1980; Jenner et al, 1983; Jacobs and Fornal, 1993). This implies that reduction of serotonergic activity leads to less inhibition and a greater dopamine availability. The third is that a reduced serotonergic tone is a known a risk factor for depression (Van Praag and De Haen, 1979). Based on these observations Mayeux et al have formulated the serotonergic hypothesis of depression in PD. This hypothesis considers the reduced serotonergic tone a physiological adaptation to the reduced dopamine activity, while at the same constituting a risk factor for depression (Mayeux et al, 1984; Mayeux, 1990). Although there are attractive alternative hypotheses about the role of serotonin in PD, this hypothesis is appealing because it provides an explanation for some common clinical observations. The presence of this biological risk factor for depression may explain the high prevalence of this condition in patients with PD (Leentjens, 2004). It may also explain the increased incidence of depression preceding the diagnosis of PD, because of the fact that pathophysiological compensatory mechanisms are already in action long before clinical symptoms become apparent (Leentjens et al, 2003b). Finally, it may provide an explanation for the exacerbation of extrapyramidal symptoms that occur in some PD patients treated with selective serotonin reuptake inhibitors (SSRIs) (Leo, 1996; Gerber and Lynd, 1998). In spite of the fact that this hypothesis was launched in 1984, to date it has not been experimentally verified.
The aim of this study is to test the serotonergic hypothesis of depression in PD in an experimental approach using the acute tryptophan depletion (ATD) paradigm.
PATIENTS AND METHODS
Subjects
In all, 15 consecutively referred eligible patients with PD, as defined by the United Kingdom Parkinson's Disease Society Brain Bank (UK-PDS-BB) criteria, were included in the study (De Rijk et al, 1997). Criteria for exclusion were the presence of concomitant neurological disorders other than PD, and the presence of concurrent psychiatric disorders, notably major depressive disorder and dementia, as defined by the criteria of the DSM IV (American Psychiatric Association, 2000a). The presence of these psychiatric disorders was assessed in a clinical interview. A prior personal or family history of major depressive disorder, as defined by DSM IV criteria, were also considered exclusion criteria. This was carried out with the intention of excluding patients with pre-existing risk factors for depression that are not associated with PD-related neurotransmitter changes. A prior personal or family history of depression are known independent risk factors for depression in the general population, that also play a role in patients with PD, and inclusion of patients with these risk factors would confound the recognition of a specific vulnerability related to the pathophysiology of PD (Leentjens et al, 2002). For the same reason, as well as to ensure optimal cooperation with and reliability of the procedure, patients with dementia, as well as those with a score lower than 23 on the Mini Mental State Examination (MMSE), were excluded (Folstein et al, 1975). Patients currently using psychopharmacological medications could not participate. Although ideally only drug-naïve, de novo patients should be included, this was not considered feasible. For pragmatic reasons the use of antiparkinsonian medication as such was not considered a ground for exclusion, except for preparations with a known strong interference with the serotonergic neurotransmitter system, such as levodopa preparations, lisuride, and selegeline. Patients on stable doses of dopamine agonists or anticholinergics were included. No patients were taken off any medication for the sake of the study. The PD patients were individually matched for sex, age, and educational level with healthy control persons from an existing bank of volunteer subjects of the Institute of Brain and Behaviour of Maastricht University, to which the same exclusion criteria were applied.
Prior to participation, the general health of the subjects was ascertained by physical examination, screening blood tests, and an electrocardiogram. Moreover, an MMSE and a Hamilton Depression Rating Scale (HAMD) were administered, to assess the patients’ cognitive and affective status (Hamilton 1960). If these investigations revealed additional grounds for exclusion, the patient could not participate. Finally, the patient was classified according to the Hoehn and Yahr (H&Y) staging system, in order to describe the global severity of PD (Hoehn and Yahr, 1967).
Patients were given a verbal explanation and written information of the study and the procedure. All participants gave their written informed consent. Our hospitals’ Medical Ethics Committee approved the study.
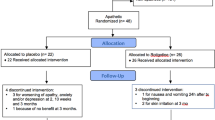
Design
The experiment was designed as a double-blind, placebo-controlled, randomized order, crossover study. Every subject underwent the ATD procedure twice: once with an amino-acid mixture without tryptophan (the active condition), and once with an amino-acid mixture containing a balanced amount of tryptophan (the placebo condition). These interventions were performed in a randomized order and spaced at least 1 week apart in order to exclude carry-over effects. Thus, both within-subject comparison between the active and placebo condition, as well as a comparison between PD patients and controls became possible.
Amino-Acid Mixtures
The preparation and composition of the amino-acid mixture was the same as described by Klaassen et al (1999b) and Riedel et al (1999) In the active condition, 3 g/100 g tryptophan was left out. Apart from the amino acids, the mixture contained 63 g carbohydrates and 33 g fat in order to dissolve the amino acids and provide caloric value. On both test occasions, the subjects ingested 75 g of amino-acid mixture, dissolved in 250 ml of water.
ATD reduces the availability of tryptophan, the precursor of serotonin, in two ways. Firstly, protein synthesis is stimulated, which uses circulating tryptophan and reduces serum tryptophan levels. Secondly, tryptophan competes with the large neutral amino acids (LNAAs: valine, leucine, isoleucine, phenylalanine, and tyrosine) for active transport over the blood–brain barrier, which results in less tryptophan entering the brain. Both plasma concentrations of tryptophan start falling 2 h, and CSF levels 2.5 h after ingestion of the amino-acid mixture, and reach a minimum after 5–7 h (Carpenter et al, 1998; Williams et al, 1999). As continuous supply and synthesis of serotonin in the brain is necessary to maintain adequate levels of serotonergic transmission, ATD creates a temporary deficiency of serotonin. The clinical and physiological consequences of ATD can be followed over a period of several hours. After the intervention, tryptophan levels quickly return to normal upon return to a normal diet (Klaassen et al, 1999b).
Procedure and Measures
At the days of the intervention, the subjects fasted from midnight. Upon arrival at our department at 0900 a baseline amino-acid spectrum was obtained, and the 32 item abbreviated Dutch version of the Profile of Mood States (POMS) questionnaire was administered (McNair et al, 1971). This version of the POMS is a measure of mood states that assesses five different qualities of mood: sadness, tension, anger, vigor, and fatigue on a 100 mm visual analogue scale. Lower scores indicate higher symptom levels. As a result of its sensitivity for transient mood changes, this questionnaire is more appropriate, and often used, in acute interventional studies than depression scales such as the HAMD or Beck Depression Inventory (BDI), because these last two are designed to measure mood over a longer period of time (typically 1 or 2 weeks) (Hamilton, 1960; Beck et al, 1961). Patients were allowed 30 min for ingestion of the amino-acid drink. At 3 and 6 h after the start of ingestion, the POMS was taken again. Subjects were provided a light protein-free lunch at noon.
Power Calculation and Statistical Procedures
As this is the first study using the ATD paradigm in PD patients a formal power calculation based on previously reported findings of effect sizes and standard deviations (SD) could not be performed. Hence, sample size calculation was based on the effect sizes and SD results of two earlier tryptophan depletion studies involving healthy volunteers, conducted in our department (Klaassen et al, 1999a, 1999b). A sample size of 15 persons per group would be adequate for detecting a difference of 1 SD with a power of 80% in a between-group analysis. As a result of two reasons we expected that with this calculation the actual power in our study would be on the safe side. First it was expected that the effect sizes (but possibly also the SD) in PD patients would be greater than in healthy control subjects because of the hypothesized greater vulnerability of PD patients. Second, sample size calculation was based on a between-group comparison only, and addition of a within-group comparison within the same multivariate analysis of variance (MANOVA) would further increase the power.
A planned interim analysis was performed after inclusion of five patients and five control subjects in order to evaluate whether ATD would be a feasible intervention in PD, and to ascertain adequate levels of tryptophan depletion (Leentjens, 2002).
Demographic variables were compared by Student's t-tests. Testing was always carried out two-tailed with the level of significance set at 0.05. The score on the POMS sadness subscale was considered the primary outcome measure. As serotonin is also associated with other disturbances in mood, the other POMS subscales were considered secondary outcome measures. Using a multiple repeated measures MANOVA, the effects of disease, disease by intervention, and disease by intervention by time were analyzed for all POMS subscales. All calculations were performed with the Statistical Package for the Social Sciences (SPSS), version 10.0 (SPSS Inc., Chicago, 1998).
RESULTS
Participants
Nine male and six female patients with an average age of 61.9 years (SD 7.51) were included in the study. Their average MMSE score was 28.9 (SD 1.4), and their average HAMD score was 2.1 (SD 1.4). The median H&Y stage was II (average stage 2.4, SD 0.6, range I–III). Two patients were medication-free de novo patients; the other patients were using an NMDA antagonist (n=1), dopamine agonists (n=4) or a combination of both (n=8). Control subjects were individually matched for sex, age, and educational level. Thus, there were no significant differences in age and MMSE score. There was however a significant, albeit not clinically relevant, difference in HAMD score between PD patients and controls that was due to higher scores of PD patients on some of the somatic symptoms of this scale. Neither patients nor control subjects had a prior personal or family history of depression. The demographic characteristics are summarized in Table 1.
Procedure
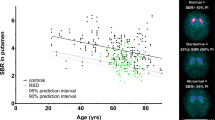
All subjects tolerated the procedure well. At the time of the interim analysis, there were no gross clinical changes in motor, affective, and cognitive symptomatology that would make continuation of this study unethical. Apart from the nausea, that occurred in four patients and two control subjects, there were no adverse events. In both PD patients and controls a significant reduction of serum tryptophan was achieved during the active procedure, but not during the placebo procedure. After 3 h, the ratio of tryptophan to other LNAA (trp/LNAA) in patients had fallen with 85%, from 7.2 to 1.1%. In control subjects the trp/LNAA ratio had fallen with 65% from 7.4 to 2.6% in the active condition. These rates of depletion were maintained until after the second set of measurements at 6 h. In the placebo condition there was a slight increase in trp/LNAA ratio. The effect of ATD is visualized in Figure 1.
Mood
The scores on all POMS subscales for patients and control subjects during the procedure are tabulated in Table 2. PD patients scored significantly lower (worse) on three of the subscales of the POMS: sadness, fatigue, and vigor, indicating a significant ‘disease effect’ (for depression F=6.49, df=1,28, p=0.017; for fatigue F=4.88, df=1,28, p=0.035; for vigor F=5.82, df=1,28, p=0.020). No significant ‘disease effect’ could be found for hostility and tension (for hostility F=3.09, df=1,28, p=0.089; for tension F=0.92, df=1,28, F=0.346). There was no significant ‘disease by intervention’ effect, nor a ‘disease by intervention by time’ effect for any of the POMS subscales. This means that for both patients and control subjects there was no within-group effect of ATD on POMS scores, nor was there any difference in response on the POMS between the two groups.
DISCUSSION
ATD Procedure
ATD has been extensively used in psychiatry to study the role of serotonin in aspects of mood regulation and cognition. Most studies report mood lowering effects of ATD in patients at risk of depression, such as patients with a mood disorder in remission, or a family history of depression or bipolar disorder (Delgado et al, 1990; Åberg-Wistedt et al, 1998; Klaassen et al, 1999a; Sobczak et al, 2002). In vulnerable individuals, ATD also exacerbates anxiety, panic, and aggression (Kent et al, 1996; Klaassen et al, 1998; LeMarquand et al, 1998).
In PD patients ATD has so far not been used to study the role of serotonin in mood or other symptom areas. Perhaps this is due to the negative experience of ATD in the only case history of a PD patient described so far (McCance-Katz et al, 1992). In this case history, the patient experienced a serious exacerbation of motor symptoms as well as emergence of depressive symptoms and a significant bradyphrenia occurred during the ATD procedure. All of these symptoms resolved within 2 h of discontinuing the testing and ingesting a meal containing a tryptophan supplement. In our study, none of these adverse events occurred and adequate levels of tryptophan depletion were achieved. Our experience is that ATD is a feasible paradigm to assess serotonergic function in PD patients.
Mood
In spite of lower baseline scores on the ‘sadness,’ ‘fatigue,’ and ‘vigor’ subscales of the POMS, there was no differential effect of ATD and the placebo condition within each group, nor was there a difference in response to the interventions between the two groups. With respect to mood, this is in contrast with earlier studies that have used the POMS during ATD to assess mood changes in non-PD subjects at risk of depression because of a positive personal or family history of depression. In our study, subjects with these known risk factors were excluded in order to study a potential risk of depression that would be specifically attributable to PD. We could find no differential responses between PD patients and control subjects that would support such a specific serotonergic vulnerability for depression.
Several potential explanations for these negative findings should be considered. A first possibility would be a possible underpowerment of the study. The difficulties in performing an adequate sample size calculation were discussed in Patients and methods. However, estimation of requested sample size was performed on the basis of two earlier studies. These studies showed that the POMS is sensitive enough to detect differential responses between study groups in vulnerable individuals even with a lower number of included subjects (Klaassen et al, 1999a, 1999b). Another possible explanation may be the existence of a floor effect. It may not be possible to further lower serotonergic activity, and thus elicit mood symptoms, in persons with an already diminished serotonergic function, such as is the case in patients with PD. A similar explanation was given by Delgado et al who reported no additional mood changes during ATD in untreated depressed patients (Delgado et al, 1994). However, our PD patients were not depressed and thus lowering of mood would be possible as a reaction to ATD. Yet another explanation is the fact that ATD is a method that is especially suitable to demonstrate presynaptic serotonergic dysfunction, while being less sensitive to demonstrate postsynaptic dysfunction. In the case of postsynaptic serotonergic dysfunction the postsynaptic cells may already be less responsive to serotonin anyway (Delgado et al, 1994). There is some evidence for postsynaptic serotonergic dysfunction in PD. Three interventions assessed serotonergic function in PD patients with different serotonin agonists. Blunted cortisol, ACTH, and prolactine responses to a fenfluramine challenge, and a blunted growth hormone response to a 5HT1A receptor challenge with sumatriptan have been reported (Kostic et al, 1996; Volpi et al, 1997a, 1997b). These studies are all indicative of a defective serotonergic control of the hypothalamic–pituitary–adrenal (HPA) axis in PD patients. A limitation of these interventions is that in a design where agonist substances are used, which enhance serotonin availability, it is not possible to elicit mood symptoms. Hence these designs are not suitable to study the serotonergic hypothesis of depression in PD. With the exception one pilot study that assessed postsynaptic 5HT2a receptor binding in PD, only presynaptic parameters, such as the 5HT transporter (5HTT) and the 5HT1a receptor have been studied. In the pilot study 5HT2a receptors were differentially increased and decreased in different brain regions that could not be linked to depression (Van Kroonenburgh et al, 2001).
If we accept that these explanations are unlikely, the only feasible explanation is that, contrary to other vulnerable groups, the known vulnerability for depression in PD patients is not directly related to the reduced serotonergic activity.
Other limitations of this study that ought to be mentioned are the fact that the allowed medication may still have played a confounding role, and the fact that there are no data on validity or reliability of the POMS in patients with PD.
Implications
In our study, the vulnerability of PD patients for depression cannot be directly linked to a reduction in serotonin activity. It can also be hypothesized that serotonin plays a more indirect role as a regulator of other neurotransmitters involved in the pathophysiology of depression, such as dopamine and noradrenalin. Although in men most studies point at an antagonistic interaction between serotonin and dopamine, animal studies also support an agonistic interaction (Scholtissen et al (accepted)). Some authors suggest that in PD serotonergic degeneration may be primary, and the degeneration of the dopamine system secondary (Steinbusch and De Vente, 1997; Braak et al, 2003). Moreover, other neurotransmitters may be more directly related to mood symptoms in PD, such as dopamine. The ‘dopaminergic hypothesis for depression in PD,’ was formulated by Fibiger in the same year as the serotonergic hypothesis was formulated (Fibiger, 1984). He considers the reduced responsible for the high incidence of depression. Deficiency in this system would lead to malfunction of self-reward systems that would constitute a risk for depression. This hypothesis would also provide an explanation for the high prevalence of depression in PD and the fact that depression may precede PD. It also provides an explanation for the beneficial effects on mood of some of the dopamine agonists, and for the problem of dopamine dependence that exists in some patients(Corrigan et al, 2000; DeBattista et al, 2000; Lawrence et al, 2003; Goldberg et al, 2004). Although formulated in 1984, this hypothesis too is still in need of experimental verification.
The pathophysiological basis of depression in PD may also influence the clinical approach to treatment. In clinical practice the treatment of depression in PD patients, is largely focused around selective serotonin reuptake inhibitors (SSRIs) or atypical agents such as venlafaxine and mirtazepine. In the ‘Practice guideline for the treatment of major depression in adults’ of the American Psychiatric Association (APA) SSRIs are mentioned, alongside bupropion, as a first choice treatment for depression in PD (American Psychiatric Association, 2000b). This advice is based on side-effect profiles, but not on efficacy or pathophysiological arguments. The two placebo-controlled trials with an SSRI in PD are characterized by a high placebo response without superior efficacy of citalopram or sertraline, respectively (Wermuth et al, 1998; Leentjens et al, 2003a). In a Cochrane review no evidence was found for superior efficacy of any antidepressant over placebo in depressed PD patients (Ghazi-Noori et al, 2004). If serotonergic deficiency is not the main pathophysiological mechanism in depression in PD, it may be worthwhile to look at other potential treatment options, including agents that more specifically address the noradrenergic and the dopaminergic system.
Conclusion
ATD is a feasible research method to assess central serotonergic function in PD. Adequate levels of tryptophan depletion were achieved without clinical adverse effects. No differential response on the POMS subscales were observed between the active and placebo condition within each group, nor was there any difference during the active condition between PD patients and controls. Although serotonin is clearly involved in the pathophysiology of PD, our study did not find evidence for a direct relation between serotonergic activity and mood symptoms. Thus, this study provides no support for the serotonergic hypothesis of depression PD. In this light, alternative hypotheses, such as the ‘dopaminergic hypothesis,’ would merit experimental investigation. In the clinical practice of treating depressed PD patients, nonserotonergic antidepressants may be interesting treatment options that should be further explored.
References
Aarsland D (1999). Mental symptoms in Parkinson's disease are important contributors to caregiver distress. Int J Geriat Psychiatr 14: 866–874.
Åberg-Wistedt A, Hasselmark L, Stain-Malmgren R, Apéria B, Kjellman BF, Mathé AA (1998). Serotonergic ‘vulnerability’ in affective disorder: a study of the tryptophan depletion test and the relationships between peripheral and central serotonin indexes in citalopram-responders. Acta Psychiatr Scand 97: 374–380.
American Psychiatric Association (2000a). Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). American Psychiatric Association: Washington.
American Psychiatric Association (2000b). Practice guideline for major depressive disorder in adults. American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorder. American Psychiatric Association: Washington. pp 413–495.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961). An inventory for measuring depression. Arch Gen Psychiatr 4: 561–571.
Braak H, Del Treci K, Rub U, De Vos RAI, Jansen Steur ENH, Braak E (2003). Staging brain pathology related to sporadic Parkinson's disease. Neurobiol Aging 24: 197–211.
Carpenter LL, Anderson GM, Pelton GH, Gudin JA, Kirwin PDS, Price LH et al (1998). Tryptophan depletion during continuous CSF sampling in healthy human subjects. Neuropsychopharmacology 19: 26–35.
Chen CPLH, Alder JT, Bray L, Kingsbury AE, Francis PT, Foster OJF (1998). Post-synaptic 5-HT1a and 5-HT2a receptors are increased in Parkinson's disease neocortex. Ann NY Acad Sci 861: 288–289.
Corrigan MH, Denehan AQ, Wright CE, Ragual RJ, Evans DL (2000). Comparison of pramipexole, fluoxetine, and placebo in patients with major depression. Depression Anxiety 11: 58–65.
De Rijk MC, Rocca WA, Anderson DW, Melcon MO, Breteler MMB, Maraganore DM (1997). A population perspective on diagnostic criteria for Parkinson's disease. Neurology 48: 1277–1281.
DeBattista C, Solvason HB, Heilig Breen JA, Schatzberg AF (2000). Pramipexole augmentation of a selective serotonin reuptake inhibitor in the treatment of depression. J Clin Psychopharm 20: 274–275.
Delgado PL, Charney DS, Price LH, Aghajanian GK, Landis H, Heninger R (1990). Serotonin functions and the mechanism of antidepressant action: reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatr 47: 411–418.
Delgado PL, Price LH, Miller HL, Salomon RM, Aghajanian GK, Henninger GR et al (1994). Serotonin and the neurobiology of depression. Effects of tryptophan depletion in drug-free depressed patients. Arch Gen Psychiat 51: 865–874.
Fibiger HC (1984). The neurobiological substrates of depression in Parkinson's disease: a hypothesis. Can J Neurol Sci 11 (Suppl 1): 105–107.
Folstein MF, Folstein SE, McHugh PR (1975). Mini Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189–198.
Gerber PE, Lynd LD (1998). Selective serotonin-reuptake inhibitor-induced movement disorders. Ann Pharmacother 32: 692–698.
Gerson SC, Baldessarini RJ (1980). Motor effects of serotonin in the central nervous system. Life Sci 27: 1435–1451.
Ghazi-Noori S, Chung TH, Deane KHO, Rickards H, Clarke CE (2004). Therapies for Depression in Parkinson's Disease. John Wiley & Sons: Chichester.
Goldberg JF, Burdick KE, Endick CJ (2004). Preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment resistent bipolar depression. Am J Psychiatr 161: 564–566.
Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatr 23: 56–62.
Hobson P, Holden A, Meara J (1999). Measuring the impact of Parkinson's disease with the Parkinson's Disease Quality of Life questionnaire. Age Ageing 28: 341–346.
Hoehn MM, Yahr MD (1967). Parkinsonism: onset, progression and mortality. Neurology 17: 427–442.
Jacobs BL, Fornal CA (1993). 5-HT and motor control: a hypothesis. Trends Neurosci 16: 346–352.
Jellinger KA (1991). Pathology of Parkinson’ disease. Changes other than the nigrostriatal pathway. Mol Chem Neuropathol 14: 153–197.
Jenner P, Sheehy M, Marsden CD (1983). Noradrenaline and 5-hydroxytryptamine modulation of brain dopamine function: implications for the treatment of Parkinson's disease. Br J Clin Pharmacol 15: 277S–289S.
Johanson B, Roos B-E (1967). 5-Hydroxyindoleacetic and homvanillic acid levels in the cerebrospinal fluid of healthy volunteers and patients with Parkinson's syndrome. Life Sci 6: 1449–1454.
Kent JM, Coplan JD, Martinez J, Karmally W, Papp LA, Gorman JM (1996). Ventilatory effects of tryptophan depletion in panic disorder: a preliminary report. Psychiatr Res 64: 83–90.
Klaassen T, Klumperbeek J, Deutz NEP, Van Praag HM, Griez E (1998). Effects of tryptophan depletion on anxiety and on panic provoked by carbon dioxide challenge. Psychiatr Res 77: 167–174.
Klaassen T, Riedel WJ, Van Someren A, Deutz NEP, Honig A, Van Praag HM (1999a). Mood effects of 24-h tryptophan depletion in healthy first degree relatives of patients with affective disorders. Biol Psychiatr 46: 489–497.
Klaassen T, Riedel WJ, Deutz NEP, Van Someren A, Van Praag HM (1999b). Specificity of the tryptophan depletion method. Psychopharmacology 141: 279–286.
Kostic VS, Djuricic BM, Covickovic-Sternic N, Bumbasirevic L, Nikoloc M, Mrsulja BB (1987). Depression and Parkinson's disease: possible role of serotonergic mechanisms. J Neurol 234: 94–96.
Kostic VS, Lecic D, Doder M, Marinkovic J, Filipovic S (1996). Prolactine and cortisol responses to fenfluramine in Parkinson's disease. Biol Psychiatr 40: 769–775.
Kuhn W, Muler T, Gerlach M, Sofic E, Fuchs G, Heye N (1996). Depression in Parkinson's disease: biogenic amines in CSF of ‘de novo’ patients. J Neural Transm 103: 1441–1445.
Lawrence AD, Evans AH, Lees AJ (2003). Compulsive use of dopamine replacement therapy in Parkinson's disease: reward systems gone awry? Lancet Neurol 2: 595–604.
Leentjens AFG (2002). Parkinson's Disease, Depression, and Serotonin. Datwyse/Universitaire Pers Maastricht: Maastricht.
Leentjens AFG (2004). Depression in Parkinson's disease: conceptual issues and clinical challenges. J Geriat Psychiatr Neurol 17: 120–126.
Leentjens AFG, Vreeling FW, Luijckx GJ, Verhey FRJ (2003a). SSRIs in the treatment of depression in Parkinson's disease. Int J Geriat Psychiatr 18: 552–554.
Leentjens AFG, Van den Akker M, Metsemakers JFM, Lousberg R, verhey J FR (2003b). Higher incidence of depression preceding the onset of Parkinson's disease: a register study. Mov Disord 18: 414–418.
Leentjens AFG, Lousberg R, Verhey FRJ (2002). Markers for depression in Parkinson's disease. Acta Psychiatr Scand 106: 196–201.
LeMarquand DG, Pihl RO, Young SN, Tremblay RE, Sequin JR, Palmour RM et al (1998). Tryptophan depletion, executive functions, and disinhibition in agressive, adolescent males. Neuropsychopharmacology 19: 333–341.
Leo RJ (1996). Movement disorders associated with the serotonin selective reuptake inhibitors. J Clin Psychiatr 57: 449–454.
Liu CY, Wang SJ, Fuh JL, Lin CH, Yang YY, Liu HC (1997). The correlation of depression with functional ability in Parkinson's disease. J Neurol 244: 493–498.
Mayeux R (1990). The ‘serotonergic hypothesis’ for depression in Parkinson's disease. Adv Neurol 53: 163–166.
Mayeux R, Stern Y, Cote L, Williams BW (1984). Altered serotonin metabolism in depressed patients with Parkinson's disease. Neurology 34: 642–646.
McCance-Katz EF, Marek KL, Price LH (1992). Serotonergic dysfunction in depression associated with Parkinson's disease. Neurology 42: 1813–1814.
McNair DM, Lorr M, Droppleman LF (1971). Manual for the Profile of Mood States. Educational and Industrial Testing Service: San Diego.
Riedel W, Klaassen T, Deutz NEP, Honig A, Van Someren A, Van Praag HM (1999). Tryptophan depletion in normal volunteers produces selective impairment in memory consolidation. Psychopharmacology 141: 362–369.
Scatton B, Javoy-Agid F, Rouquier L, Dubois B, Agid Y (1983). Reduction of cortical dopamine, noradrenaline, serotonin and their metabolites in Parkinson's disease. Brain Res 275: 321–328.
Scholtissen B, Verhey FRJ, Steinbusch HWM, Leentjens AFG (accepted). Serotonergic mechanisms in Parkinson's disease: opposing results from preclinical and clinical data. J Neural Transm.
Sobczak S, Honig A, Nicolson N, Riedel W (2002). Effects of acute tryptophan depletion on mood and cortisol levels in first-degree relatives of type I and type II bipolar patients and healthy matched controls. Neuropsychopharmacology 27: 834–842.
Steinbusch HWM, De Vente J (1997). New vistas on the neurobiology of depression: colocalization of serotonin-, dopamin-, and nitric oxide synthase-containing neurones in the dorsal raphe. In: Honig A, Van Praag HM (eds). Depression: Neurobiological, Psychopathological and Therapeutic Advances. John Wiley & Sons Ltd: Chichester.
Troster AI, Stalp LD, Paolo AM, Fields JA, Koller WC (1995). Neuropsycholological impairment in Parkinson's disease with and without depression. Arch Neurol 52: 1164–1169.
Van Kroonenburgh M, Leentjens A, Verhey F, Vreeling F, Troost J (2001). Imaging of serotonin 5-HT2a receptors in Parkinson's disease. J Nucl Med 42 (Suppl 5): 227P.
Van Praag HM, De Haen S (1979). Central serotonergic metabolism and frequency of depression. Psychiatr Res 1: 219–224.
Volpi R, Caffara P, Scaglioni A, Boni S, Saginario A, Chiodera P et al (1997a). Defective 5-HT1-receptor-mediated neurotransmission in the control of growth hormon in Parkinson's disease. Neuropsychobiology 35: 79–83.
Volpi R, Caffarra P, Boni S, Scaglioni A, Malvezzi L, Saginario A et al (1997b). ACTH/cortisol involvement in the serotonergic disorder affecting the Parkinsonian brain. Neuropsychobiology 35: 73–78.
Wermuth L, Sorensen PS, Timm S, Christensen B, Utzon NP, Boas J et al (1998). Depression in idiopathic Parkinson's disease treated with citalopram. Nordic J Psychiatr 52: 163–169.
Williams WA, Shoaf SE, Hommer D, Rawling R, Linnoilla M (1999). Effects of acute tryptophan depletion on plasma and cerebrospinal fluid tryptophan and 5-hydroxyindoleacetic acid in normal volunteers. J Neurochem 72: 1641–1647.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leentjens, A., Scholtissen, B., Vreeling, F. et al. The Serotonergic Hypothesis for Depression in Parkinson's Disease: an Experimental Approach. Neuropsychopharmacol 31, 1009–1015 (2006). https://doi.org/10.1038/sj.npp.1300914
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300914
Keywords
This article is cited by
-
Depression in Parkinson disease—epidemiology, mechanisms and management
Nature Reviews Neurology (2012)
-
Personality traits in patients with Parkinson’s disease: assessment and clinical implications
Journal of Neurology (2012)
-
Impulse control disorders in Parkinson’ disease: the role of personality and cognitive status
Journal of Neurology (2012)
-
Serotonergic vulnerability and depression: assumptions, experimental evidence and implications
Molecular Psychiatry (2007)