Abstract
Ghrelin, a growth hormone (GH) secretagogue receptor ligand was isolated from the stomach and hypothalamus of rats and humans. In rodents, ghrelin exerts distinct orexigenic action, probably as counterpart of the anorexigenic leptin. In humans, ghrelin infusion enhances appetite. It is unknown whether single intravenous (i.v.) injections of ghrelin affect human eating behavior. Therefore, we investigated the influence of a single i.v. bolus injection of 100 μg ghrelin on appetite, ideas about food, hormone levels, and glucose concentration in young control subjects. In order to test gender differences, we included five women and four men. After ghrelin administration, appetite was enhanced in eight of nine subjects. Seven probands reported a vivid, plastic image of their preferred meal. Furthermore, ghrelin stimulated an immediate increase in plasma levels of GH (area under the curve, mean±SEM 35±16 ng/ml × min after placebo [P] to 2808±533 ng/ml × min after ghrelin [G]; p<0.001), cortisol (5908±984 ng/ml × min [P] to 10179±1293 ng/ml × min [G]; p<0.001), and ACTH (922±103 pg/ml × min [P] to 3030±763 pg/ml × min [G]; p<0.02), whereas leptin levels remained unchanged. Contrary to placebo, glucose concentration did not decrease markedly after administration of ghrelin. Our data suggest that i.v. ghrelin stimulates appetite and images of food in young women and men. Obviously, leptin is not involved in these effects.
Similar content being viewed by others
INTRODUCTION
Ghrelin, a hormone peptide was identified as endogenous ligand of the growth hormone (GH) secretagogue (GHS) receptor. It was isolated from human and rat stomach and immunochemistry indicates its presence in the hypothalamus and other tissues (Kojima et al, 1999; Kojima et al, 2001). In addition to stimulating the release of GH, ACTH, and cortisol in humans (Peino et al, 2000; Takaya et al, 2000; Arvat et al, 2001) and of GH in the rat (Kojima et al, 1999; Wren et al, 2000), ghrelin is thought to play a key role in the energy balance (Horvath et al, 2001). In rats, ghrelin promoted food intake and weight gain (Tschöp et al, 2000; Nakazato et al, 2001; Wren et al, 2000). A complementary action of ghrelin as orexigenic factor and of leptin as inhibitor of food intake was suggested (Horvath et al, 2001). Ghrelin levels were elevated before meals (Cummings et al, 2001) and decreased after food intake (Tschöp et al, 2000). In comparison to normal controls, obese subjects showed blunted ghrelin levels (Tschöp et al, 2001b), whereas ghrelin was elevated in patients with anorexia (Otto et al, 2001). In normal women and men, infusion of ghrelin stimulated appetite and calorie intake (Wren et al, 2001).
We observed recently that after a single intravenous (i.v.) bolus given at 2200, a young normal man who had a sufficient dinner by 1800 developed a hunger attack. Subsequently, he had a large meal (Weikel et al, 2003). This observation fits with various studies from our laboratory and others showing that repetitive (Steiger and Holsboer, 1997; Weikel et al, 2003) and single (Kerkhofs et al, 1993; Antonijevic et al, 1999a) i.v. bolus injections of neuropeptides modulate human behavior, and in the latter experiments, modulate sleep. After a lower dose of ghrelin, 4 × 50 μg given in a pulsatile manner between 2200 and 0100 to young normal male controls, appetite and leptin levels remained unchanged, whereas slow wave sleep (SWS), GH, cortisol, and prolactin secretion increased (Weikel et al, 2003). In a similar protocol, we found previously opposite effects of GH-releasing hormone (GHRH) in normal women and men. After GHRH, sleep was impaired and ACTH and cortisol levels increased in women, whereas sleep was promoted and HPA hormone levels were blunted in men (Antonijevic et al, 2000a, 2000b). In contrast, after 1.0 μg/kg i.v. ghrelin or GHRH given in the morning, no gender differences were found in the response of GH, ACTH, and cortisol (Broglio et al, 2003).
Several issues concerning the neuroendocrine effects of ghrelin remain to be clarified:
-
1)
Is appetite in humans changed by a single bolus injection of 100 μg in the morning?
-
2)
Does ghrelin affect mental representations of food intake in addition to stimulating hunger?
-
3)
Is a change of appetite after exogenous ghrelin linked with changes of plasma levels of leptin?
-
4)
Is there a sexual dimorphism regarding the behavioral and endocrine effects of ghrelin similar to the opposite effects of GHRH in women and men (Antonijevic et al, 2000a; Antonijevic et al, 2000b)?
In order to clarify these questions, we investigated the effect of an i.v. bolus injection of ghrelin on appetite, ideas about food and levels of GH, ACTH, cortisol, leptin, and glucose.
MATERIAL AND METHODS
Participants
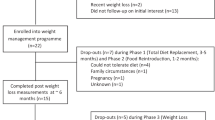
Nine normal control subjects (five women, four men, with a mean age±SD of 28.2±4.1, range 21–31 years) participated in this study. They were of normal height and weight with a body mass index of 22.4±3.1. All subjects underwent clinical examinations and extensive laboratory tests, including electrocardiogram and electroencephalogram to exclude acute illness and psychiatric disorders in their own and in their family history. One female subject was on contraceptive medication; all other females were investigated during their early follicular phase. Another female subject has been taking a constant dose of thyroid medication for 10 years. All other subjects were drug free for at least 2 months. All procedures were carried out with the adequate understanding and written consent of the subjects. The study was approved by the local ethics committee.
Protocol
Participants attended two test sessions on consecutive days. On both study days, after an overnight fast, a forearm i.v. catheter was inserted at 0845. At 0902, 100 μg ghrelin (Clinalfa, Läufelfingen, Switzerland) or placebo (saline infusion) was injected as a single i.v. bolus injection according to a double-blind randomized crossover schedule. Blood samples were taken every 15 min from 0900 to 1000. Plasma concentrations of GH, cortisol, ACTH, and leptin were measured at each time point. In addition, glucose levels were determined at 0900 and 1000. At 1000, subjects filled in a questionnaire comprising a 10-point visual analogue scale for the assessment of self-rated appetite during the past hour, with zero for no and 10 for very high feelings of appetite. Furthermore, the subjects wrote down the kind and the predominant flavor quality (sweet, sour, salty) of the meal for which they realized the strongest appetite. They were additionally asked whether and to which degree they perceived a vivid and plastic visualization of their preferred meal with (+) indicating a low, (++) a medium, and (+++) a high degree of visualization. Finally, the kind and the duration of possible side effects were recorded (fatigue, euphoria, emesis, vertigo, flush).
Hormone Analysis
The plasma concentrations of GH, ACTH, cortisol, and leptin were analyzed by commercial radio immunoassays as reported in detail elsewhere (Frieboes et al, 2004).
Data Analysis
We did not detect any effects of the verum–placebo order. After combining the two order groups, areas under the plasma concentration curves (AUC) were calculated for all endocrine parameters by applying trapezoidal integration. Differences in baseline and change in the AUC values of GH, ACTH, cortisol, leptin, and glucose between placebo and ghrelin infusion was evaluated with nonparametric Wilcoxon's matched pairs test. In case of significant baseline differences, an analysis of covariance controlling for baseline differences was additionally calculated. Gender effects were evaluated by Mann–Whitney U-tests. Associations between endocrine variables and age, gender, BMI, change of plasma glucose levels, and change of appetite level were assessed by nonparametric Kendall's τ correlation.
Means and standard deviations are reported. The level of significance was set to p=0.05.
RESULTS
Effects on Appetite and Side Effects
Ghrelin administration induced a significant increase in appetite in eight of the nine subjects with a mean score of 6.2 (SD=3.2), while this was not the case after placebo infusion (0.9±1.5; p<0.05). Of the nine subjects, seven reported a vivid, plastic visualization of their preferred meal after ghrelin but not after placebo infusion. Three male subjects imagined a salty meal, three women a sweet meal, and one woman a sour meal (Table 1).
Subjects experienced fatigue lasting up to 1 h (n=6), elevated mood (n=3), vertigo (n=3), emesis (n=4), and flush (n=5) after ghrelin infusion, while no side effects were reported after placebo (Table 1).
Endocrine Effects
Ghrelin exhibited pronounced effects on plasma concentrations of GH, cortisol, and ACTH (see Table 2). Plasma concentrations of these hormones tended to return to baseline after 1 h (Figure 1). Baseline differences (plasma concentration at 0900 prior to saline or ghrelin infusion) were observed for GH (p<0.05) and for cortisol (p<0.05) but not for ACTH (NS) or leptin (NS). Analysis of covariance controlling for baseline difference confirmed the significant effects of ghrelin on GH (F1,7=14.66, p=0.006) and cortisol (F1,7=14.55, p=0.007) plasma concentrations.
Plasma leptin concentrations were not affected by the infusion of ghrelin. Glucose concentrations after administration of ghrelin were almost unchanged (91.4±6.4 to 89.0±11.4 mg/dl) and tended to decrease after placebo (90.8±7.7 to 85.6±13.6 mg/dl), but the difference was not statistically significant (see Table 2).
Gender Effects and Associations with Age- and Weight-Associated Variables
Women exhibited higher GH and leptin concentrations after placebo and after ghrelin infusion (p<0.05) and lower ACTH after placebo infusion (p<0.05). Regarding the effects of ghrelin infusion, we observed a more pronounced increase of GH after ghrelin in women compared with men (Table 3). No gender effects were found for the ghrelin effects on ACTH and cortisol, suggesting a similar pattern of ghrelin-induced HPA system activation in men and women. No gender effects were observed for ghrelin-induced changes on leptin and glucose concentration, which did not surprise since these variables were not affected by the ghrelin infusion.
Neither endocrine changes nor the appetite-stimulating effect of ghrelin were significantly influenced by age or the body mass index. The decrease in the glucose plasma concentrations (0900–1000) under the placebo condition (r=−0.76, p<0.01) but not under the ghrelin stimulation (r=0.06, NS) was correlated with the cortisol levels under the respective conditions.
DISCUSSION
Our data show a rapid stimulation of appetite, imagination of food, GH, ACTH, and cortisol, and an attenuation of glucose levels after an i.v. bolus injection of ghrelin in young normal women and men after an overnight fast in comparison to placebo. Leptin levels, however, remained unchanged.
The view that ghrelin is the most potent endogenous stimulus for appetite is supported. This theory derives originally from the animal model. Acute and chronic administration of ghrelin enhances food intake and weight gain (Tschöp et al, 2000; Nakazato et al, 2001). Furthermore, observations such as the increase of ghrelin concentration before meals (Cummings et al, 2001) and the subsequent decrease after meals (Tschöp et al, 2001a) in normal controls, as well as increased levels of ghrelin in patients with anorexia nervosa (Otto et al, 2001) and moreover blunted levels in obese subjects (Tschöp et al, 2001b) point to a relationship between ghrelin and food intake. In humans, ghrelin infusion induces hunger (Arvat et al, 2000). In a first systematic study on the influence of exogenous ghrelin administration on appetite and eating in humans, Wren et al (2001) infused ghrelin to young normal women and men. The subjects reported an increase in appetite and they showed a higher calorie intake than after placebo.
In our study, a single bolus injection of 100 μg ghrelin was sufficient to prompt a distinct increase of appetite in subjects who were already hungry after an overnight fast. The effects of ghrelin appear to be dose dependent. After 4 × 50 μg ghrelin given in hourly injections between 2200 and 0100, appetite remained unchanged, whereas SWS, GH, cortisol, and prolactin increased (Weikel et al, 2003). In a single case observation, 100 μg ghrelin given at 2200 prompted a distinct increase of hunger and food intake (Weikel et al, 2003). In a similar vein, a study in mice points to different mechanisms in the regulation of food intake and sleep by ghrelin. Ghrelin enhanced eating both in mice with intact and deficient GHRH receptors. On the contrary, promotion of sleep required intact GHRH receptors (Obál et al, 2003).
In addition to the augmentation of appetite, seven out of nine subjects reported that they had vivid imagination of their favorite meal after ghrelin administration. The imagined, preferred flavor of this meal differed between females and males. These observations suggest that the role of ghrelin in the regulation of human food intake is more complex than a signal for hunger. In humans, various cognitive components participate in the initiation of eating and in the selection of food. The hippocampus is thought to be a site for visual imagination (Kreiman et al, 2000) and GHS receptors in the hippocampus are targets for ghrelin (Nakazato et al, 2001) and may mediate its effect on the imagination of food. Similar to our previous studies on specific effects of peripherally administered peptides on the sleep electroencephalogram in humans (for a review see Steiger and Holsboer, 1997), the blood–brain interface did not prevent effects of ghrelin on behavior. It was hypothesized that the unique Ser3 acylation facilitates the penetration of the blood–brain interface by ghrelin (Horvath et al, 2001).
Next to ghrelin, leptin is thought to be the other major factor in the energy balance. Contrary to ghrelin, leptin appears to inhibit food intake. We observed elevated nocturnal leptin levels in patients with affective disorders (Antonijevic et al, 1998) when compared to controls. This may contribute to the loss of appetite in depression. Preclinical data suggest an inverse interaction of ghrelin and leptin (Shintani et al, 2001), whereas leptin levels remained unchanged in the rat after i.v. administration of a synthetic peptide corresponding to amino acid 1–28 of rodent ghrelin (Kamegai et al, 2001). Our present study shows acute CNS and pituitary effects of ghrelin, but no effects on leptin levels during the relatively short interval of the examination. Obviously, the observed acute behavioral effects of ghrelin are not mediated by leptin. Similarly, nocturnal leptin concentrations remained unchanged after repetitive administration of 40 × 50 μg ghrelin, a dose which did not affect appetite (Weikel et al, 2003), and after the synthetic GHS, hexarelin in young normal men (Frieboes et al, 2004). Furthermore, injection of leptin into nonobese humans had no effects on the cardiovascular or autonomic nervous systems and no evident effects on weight control (Mackintosh and Hirsch, 2001). Possible long-term effects of ghrelin on leptin in humans should be investigated in future studies. In contrast to leptin, ghrelin affected glucose levels. The decline in glucose levels after placebo was attenuated. This resembles the increase of glucose after ghrelin in normal male volunteers (Broglio et al, 2001). This effect may play a role in the conservation of energy by ghrelin.
As expected from recent human and preclinical studies (Arvat et al, 2000; Peino et al, 2000; Takaya et al, 2000; Kojima et al, 2001; Wren et al, 2000), GH, ACTH, and cortisol levels increased after ghrelin. Similarly, we found increases of nocturnal GH, ACTH, and cortisol levels after ghrelin (Weikel et al, 2003) and after the synthetic GHS, GH-releasing peptide-6 (GHRP-6) (Frieboes et al, 1999) and hexarelin (Frieboes et al, 2004).
The response of GH to ghrelin was more distinct in women than in men. Physiologically, the GH profile in women shows various peaks during the 24 h rhythms, whereas in men there are more distinct peaks associated with sleep onset (Antonijevic et al, 1999b). This might be an explanation for higher basal and, in consequence, stimulated GH levels in women in the morning hours. Given the small sample size, our observation should be seen with caution, since in another report, after 1 μg/kg ghrelin, the GH response did not show a difference between young females and young males (Broglio et al, 2003). Similar to this study, no other gender-dependent difference in the response of appetite and hormone secretion to ghrelin was found. This is in contrast to the inverse action of GHRH on sleep EEG and on sleep-related hormone secretion in females and males (Antonijevic et al, 2000b). However, it cannot be ruled out that the sample size in our study is too small to provide sufficient power for the detection of all gender effects. Fatigue was the most frequent side effect of ghrelin in our study. In related studies, we (Weikel et al, 2003; Frieboes et al, 1999) and others (Copinschi et al, 1997) reported sleep promotion by ghrelin, GHRP-6, and the GHS MK-677. Interestingly, transient euphoria was found in three subjects. Systematic studies appear necessary to elucidate the role of ghrelin in the regulation of mood and in the involvement in the pathophysiology of affective disorders. Interestingly, besides appetite also emesis was induced in four subjects. This effect was rated ‘low’ in three persons and ‘middle’ in one subject. The lack of visualization of a favorite meal in this subject may be explained by the latter side effect.
In sum, our findings suggest that the role of ghrelin in the regulation of human eating is even more complex than suspected so far. In addition to stimulation of appetite, cognitive functions appear to be involved. Exogenous i.v. ghrelin is suggested to be capable of promoting appetite independently from acute action on leptin. Fatigue and elevated mood in some subjects after administration of ghrelin suggest widespread behavioral effects of ghrelin.
References
Antonijevic IA, Murck H, Frieboes RM, Barthelmes J, Steiger A (2000a). Sexually dimorphic effects of GHRH on sleep–endocrine activity in patients with depression and normal controls—part I: the sleep EEG. Sleep Res Online 3: 5–13.
Antonijevic IA, Murck H, Frieboes RM, Holsboer F, Steiger A (1999a). Hyporesponsiveness of the pituitary to CRH during slow wave sleep is not mimicked by systemic GHRH. Neuroendocrinology 69: 88–96.
Antonijevic IA, Murck H, Frieboes RM, Holsboer F, Steiger A (1999b). On the gender differences in sleep–endocrine regulation in young normal humans. Neuroendocrinology 70: 280–287.
Antonijevic IA, Murck H, Frieboes RM, Horn R, Brabant G, Steiger A (1998). Elevated nocturnal profiles of serum leptin in patients with depression. J Psychiatr Res 32: 403–410.
Antonijevic IA, Murck H, Frieboes RM, Steiger A (2000b). Sexually dimorphic effects of GHRH on sleep–endocrine activity in patients with depression and normal controls—part II: hormone secretion. Sleep Res Online 3: 15–21.
Arvat E, Di Vito L, Broglio F, Papotti M, Muccioli G, Dieguez C et al (2000). Preliminary evidence that ghrelin, the natural GH secretagogue (GHS)-receptor ligand, strongly stimulates GH secretion in humans. J Endocrinol Invest 23: 493–495.
Arvat E, Maccario M, Di Vito L, Broglio F, Benso A, Gottero C et al (2001). Endocrine activities of ghrelin, a natural growth hormone secretagogue (GHS), in humans: comparison and interactions with hexarelin, a nonnatural peptidyl GHS, and GH-releasing hormone. J Clin Endocrinol Metab 86: 1169–1174.
Broglio F, Arvat E, Benso A, Gottero C, Muccioli G, Papotti M et al (2001). Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J Clin Endocrinol Metab 86: 5083–5086.
Broglio F, Benso A, Castiglioni C, Gottero C, Prodam F, Destefanis S et al (2003). The endocrine response to ghrelin as a function of gender in humans in young and elderly subjects. J Clin Endocrinol Metab 88: 1537–1542.
Copinschi G, Leproult R, Van Onderbergen A, Caufriez A, Cole KY, Schilling LM et al (1997). Prolonged oral treatment with MK-677, a novel growth hormone secretagogue, improves sleep quality in man. Neuroendocrinology 66: 278–286.
Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS (2001). A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50: 1714–1719.
Frieboes RM, Antonijevic IA, Held K, Murck H, Pollmächer T, Uhr M et al (2004). Hexarelin decreases slow-wave sleep and stimulates the sleep-related secretion of GH, ACTH, cortisol and prolactin in healthy volunteers. Psychoneuroendocrinology 29: 851–860.
Frieboes RM, Murck H, Antonijevic IA, Steiger A (1999). Effects of growth hormone-releasing peptide-6 on the nocturnal secretion of GH, ACTH and cortisol and on the sleep EEG in man: role of routes of administration. J Neuroendocrinol 11: 473–478.
Horvath TL, Diano S, Sotonyi P, Heiman M, Tschöp M (2001). Minireview: ghrelin and the regulation of energy balance—a hypothalamic perspective. Endocrinology 142: 4163–4169.
Kamegai J, Tamura H, Shimizu T, Ishii S, Sugihara H, Wakabayashi I (2001). Chronic central infusion of ghrelin increases hypothalamic neuropeptide Y and agouti-related protein mRNA levels and body weight in rats. Diabetes 50: 2438–2443.
Kerkhofs M, Van Cauter E, Van Onderbergen A, Caufriez A, Thorner MO, Copinschi G (1993). Sleep-promoting effects of growth hormone-releasing hormone in normal men. Am J Physiol 264: E594–E598.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K (1999). Ghrelin is a growth hormone-releasing acylated peptide from stomach. Nature 402: 656–660.
Kojima M, Hosoda H, Matsuo H, Kangawa K (2001). Ghrelin: discovery of the natural endogenous ligand for the growth hormone secretagogue receptor. Trends Endocrinol Metab 12: 118–122.
Kreiman G, Koch C, Fried I (2000). Imagery neurons in the human brain. Nature 408: 357–361.
Mackintosh RM, Hirsch J (2001). The effects of leptin administration in non-obese human subjects. Obesity Res 9: 462–469.
Nakazato M, Murakami N, Date Y, Kojima M, Matsuo H, Kangawa K et al (2001). A role for ghrelin in the central regulation of feeding. Nature 409: 194–198.
Obál Jr F, Alt J, Taishi P, Gardi J, Krueger JM (2003). Sleep in mice with non-functional growth hormone-releasing hormone receptors. Am J Physiol – Regul Integr Comp Physiol 284: R131–R139.
Otto B, Cuntz U, Fruehauf E, Wawarta R, Folwaczny C, Riepl RL et al (2001). Weight gain decreases elevated plasma ghrelin concentrations of patients with anorexia nervosa. Eur J Endocrinol 145: R5–R9.
Peino R, Baldelli R, Rodriguez-Garcia J, Rodriguez-Segade S, Kojima M, Kangawa K et al (2000). Ghrelin-induced growth hormone secretion in humans. Eur J Endocrinol 143: R11–R14.
Shintani M, Ogawa Y, Ebihara K, Aizawa-Abe M, Miyanaga F, Takaya K et al (2001). Ghrelin, an endogenous growth hormone secretagogue, is a novel orexigenic peptide that antagonizes leptin action through the activation of hypothalamic neuropeptide Y/Y1 receptor pathway. Diabetes 50: 227–232.
Steiger A, Holsboer F (1997). Neuropeptides and human sleep. Sleep 20: 1038–1052.
Takaya K, Ariyasu H, Kanamoto N, Iwakura H, Yoshimoto A, Harada M et al (2000). Ghrelin strongly stimulates growth hormone (GH) release in humans. J Clin Endocrinol Metab 85: 4908–4911.
Tschöp M, Smiley DL, Heiman ML (2000). Ghrelin induces adiposity in rodents. Nature 407: 908–913.
Tschöp M, Wawarta R, Riepl RS, Friedrich S, Bidlingmaier M, Landgraf R et al (2001a). Post-prandial decrease of circulating human ghrelin levels. J Endocrinol Invest 24: RC19–RC21.
Tschöp M, Weyer C, Tataranni PA, Devanarayan V, Ravussin E, Heiman ML (2001b). Circulating ghrelin levels are decreased in human obesity. Diabetes 50: 707–709.
Weikel JC, Wichniak A, Ising M, Brunner H, Friess E, Held K et al (2003). Ghrelin promotes slow-wave sleep in humans. Am J Physiol – Endocrinol Metab 284: E407–E415.
Wren AM, Seal LJ, Cohen MA, Brynes AE, Frost GS, Murphy KG et al (2001). Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab 86: 5992–5995.
Wren AM, Small CJ, Ward HL, Murphy KG, Dakin CL, Taheri S et al (2000). The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology 141: 4325–4328.
Acknowledgements
This study was supported by a grant from the Deutsche Forschungsgemeinschaft (Ste 486/5-1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmid, D., Held, K., Ising, M. et al. Ghrelin Stimulates Appetite, Imagination of Food, GH, ACTH, and Cortisol, but does not Affect Leptin in Normal Controls. Neuropsychopharmacol 30, 1187–1192 (2005). https://doi.org/10.1038/sj.npp.1300670
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300670
Keywords
This article is cited by
-
Involvement of the ghrelin system in the maintenance and reinstatement of cocaine-motivated behaviors: a role of adrenergic action at peripheral β1 receptors
Neuropsychopharmacology (2022)
-
Potential gut–brain mechanisms behind adverse mental health outcomes of bariatric surgery
Nature Reviews Endocrinology (2021)
-
The cellular and molecular bases of leptin and ghrelin resistance in obesity
Nature Reviews Endocrinology (2017)
-
Mindfulness Reduces Reactivity to Food Cues: Underlying Mechanisms and Applications in Daily Life
Current Addiction Reports (2017)
-
Effect of Ghrelin Administration on Serum Corticostrone, T3, T4 and Some Biochemical Indices in the Turkey (Meleagridis gallopova)
International Journal of Peptide Research and Therapeutics (2017)