Abstract
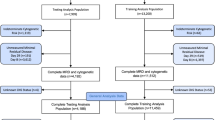
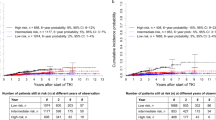
The purpose of the paper was to define clinical or biological features associated with the risk for treatment failure for children with acute myeloid leukemia. Data from 560 children and adolescents with newly diagnosed acute myeloid leukemia who entered the Pediatric Oncology Group Study 8821 from June 1988 to March 1993 were analyzed by univariate and recursive partitioning methods. Children with Down syndrome or acute promyelocytic leukemia were excluded from the study. Factors examined included age, number of leukocytes, sex, FAB morphologic subtype, cytogenetic findings, and extramedullary disease at the time of diagnosis. The overall event-free survival (EFS) rate at 4 years was 32.7% (s.e. = 2.2%). Age ⩾2 years, fewer than 50 × 109/l leukocytes, and t(8;21) or inv(16), and normal chromosomes were associated with higher rates of EFS (P value = 0.003, 0.049, 0.0003, 0.031, respectively), whereas the M5 subtype of AML (P value = 0.0003) and chromosome abnormalities other than t(8;21) and inv(16) were associated with lower rates of EFS (Pvalue = 0.0001). Recursive partitioning analysis defined three groups of patients with widely varied prognoses: female patients with t(8;21), inv(16), or a normal karyotype (n = 89) had the best prognosis (4-year EFS = 55.1%, s.e. = 5.7%); male patients with t(8;21), inv(16) or normal chromosomes (n = 106) had an intermediate prognosis (4-year EFS = 38.1%, s.e. = 5.3%); patients with chromosome abnormalities other than t(8;21) and inv(16) (n = 233) had the worst prognosis (4-year EFS = 27.0%, s.e. = 3.2%). One hundred and thirty-two patients (24%) could not be grouped because of missing cytogenetic data, mainly due to inadequate marrow samples. The results suggest that pediatric patients with acute myeloid leukemia can be categorized into three potential risk groups for prognosis and that differences in sex and chromosomal abnormalities are associated with differences in estimates of EFS. These results are tentative and must be confirmed by a large prospective clinical trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Smith M, Arthur D, Camitta B, Carroll AJ, Crist W, Gaynon P, Gelber R, Heerema N, Korn ML, Link M, Murphy S, Pui CH, Pullen J, Reamon G, Sallan SE, Sather H, Shuster J, Simon R, Trigg M, Tubergen D, Uckun F, Ungerleider R . Uniform approach to classification and treatment assignment for children with acute lymphoblastic leukemia J Clin Oncol 1996 14: 18–24
Weinstein HJ, Mayer RH, Rosenthal DS, Coral FS, Camitta EM, Gelber RD . Chemotherapy for acute myelogenous leukemia in children and adults: VAPA update Blood 1983 62: 315–319
Steuber CP, Civin C, Krisher J, Culbert S, Ragab A, Ruymann FB, Ravindranath Y, Leventhal B, Wilkinson R, Vietti TJ . A comparison of induction and maintenance therapy for acute nonlymphocytic leukemia in childhood: results of a Pediatric Oncology Group study J Clin Oncol 1991 9: 247–258
Creutzig U, Ritter J, Schellong G . Identification of two risk groups in childhood acute myelogenous leukemia after therapy intensification in the study AML-BFM-83 as compared with study AML-BFM-78. AML-BFM Study Group Blood 1990 75: 1932–1940
Creutzig U, Harbott J, Sperling C, Ritter J, Zimmermann M, Loffler H, Riehm H, Schellong G, Ludgwig WD . Clinical significance of surface antigen expression in children with acute myeloid leukemia: results of study AML-BFM-87 Blood 1995 86: 3097–3108
Woods WG, Kobrinsky N, Buckley J, Neudorf S, Sander J, Miller L, Barnard D, Benjamin D, DeSwarte J, Kalousek D . Intensively timed induction therapy followed by autologous or allogeneic bone marrow transplantation for children with acute myeloid leukemia or myelodysplastic syndrome: a Children's Cancer Group pilot study J Clin Oncol 1993 11: 1448–1457
Ravindranath Y, Steuber CP, Krischer J, Civin CI, Ducore J, Vega R, Pitel P, Inoue S, Bleher R, Sexauer C . High-dose cytarabine for intensification of early therapy of childhood acute myeloid leukemia: a Pediatric Oncology Group study J Clin Oncol 1991 9: 572–580
Ravindranath Y, Yeager AM, Chang MN, Steuber CP, Krischer J, Graham-Pole J, Carroll A, Inoue S, Camitta B, Weinstein HJ . Autologous bone marrow transplantation versus intensive consolidation chemotherapy for acute myeloid leukemia in childhood New Engl J Med 1996 334: 1428–1434
Woods WG, Kobrinsky N, Buckley JD, Lee JW, Sanders J, Neudorf S, Gold S, Barnard DR, DeSwarte J, Dusenbery K, Kalousek D, Arthur DC, Lange BJ . Timed-sequential induction therapy improves postremission outcome in acute myeloid leukemia: a report from Children's Cancer Group Blood 1996 87: 4979–4989
Hann I, Stevens RF, Goldstone AH, Rees JK, Wheatley K, Gray RG, Burnett AK . Randomized comparison of DAT versus ADE as induction chemotherapy in children and adults with acute myeloid leukemia. Results of the Medical Research Council's AML trial (MRC AML-10). Adult and Childhood Working Parties of the Medical Research Council Blood 1997 89: 2311–2318
Ravindranath Y, Abella E, Krischer JP, Wiley J, Inoue S, Harris M, Chauvenet A, Alvarado CS, Dubowy R, Pitchery AK . Acute myeloid leukemia (AML) in Down's syndrome is highly responsive to chemotherapy: experience on Pediatric Oncology Group AML Study 8498 Blood 1992 80: 2210–2214
Degos L, Dombret H, Chomianne C, Daniel MT, Miclea JM, Chastang C, Castaigne S, Fenaux P . All-trans-retinoic acid as a differentiating agent in the treatment of acute promyelocytic leukemia Blood 1995 85: 2643–2653
Bloomfield CD, Lawrence D, Byrd JC, Carrol A, Pettenati MJ, Tantravahi R, Patil SR, Davey PR, Berg DT, Schiffer CA, Arthur DC, Mayer RJ . Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype Cancer Res 1998 58: 4173–4179
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A . The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML, 10 trial. The Medical Research Council Adult and Children's Leukemia working Parties Blood 1998 7: 2322–2333
Raimondi SC, Chang MN, Ravindranath Y, Behm FG, Gresik MV, Steuber CP, Weinstein HJ, Carroll AJ for the Pediatric Oncology Group . Chromosomal abnormalities in 478 children with acute myeloid leukemia: clinical characteristics and treatment outcome a cooperative Pediatric Oncology Group study – POG 8821 Blood 1999 94: 3707–3716
Ciampi A, Hogg SA, Kates L . Stratification by stepwise regression, correspondence, analysis, and recursive partitioning: a comparison of three methods of survival analysis with covariates Comput Stat Data Anal 1986 4: 183–204
Shuster JJ, Falletta JM, Pullen DJ, Crist WM, Humphrey GB, Dowell BL, Wharam MD, Borounitz M . Prognostic factors in children with T-cell acute lymphoblastic leukemia: a Pediatric Oncology Group study Blood 1990 75: 166–173
Harris MB, Shuster JJ, Carroll A, Look AT, Borowitz MJ, Crist WM, Nitschke R, Pullen J, Steuber CP, Land VJ . Trisomy of leukemic cell chromosomes 4 and 10 identifies children with B-progenitor cell acute lymphoblastic leukemia with a very low risk of treatment failure: a Pediatric Oncology Group study Blood 1992 79: 3316–3324
Cox DR . Regression models and life-tables JR Stat Sec B 1992 34: 187–220
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations J Am Stat Assoc 1958 53: 475–481
Lie SO, Jonmundsson G, Mellander L, Silimes MA, Yssing M, Gustafsson G . A population-based study of 272 children with acute myeloid leukemia treated on two consecutive protocols with different intensity: best outcome in girls, infants and children with Down's syndrome. Nordic Society of Paediatric Haematology and Oncology (NOPHO) Br J Haematol 1996 94: 82–88
Zittoun RA, Mandelli F, Willemze R, de Witte T, Labar B, Resegotti L, Leoni F, Damasio E, Visani G, Papa G . Autologous or allogeneic bone marrow transplantation compared with intensive chemotherapy in acute myelogenous leukemia. European Organization for Research and Treatment of Cancer (EORTC) and the Gruppo Italiano Malattie Ematologiche Maligne del'Adulto (GIMEMA) Leukemia Cooperative Groups New Engl J Med 1995 332: 217–223
Keating MJ, Smith TL, Kantarjian H, Cork A, Walters R, Trujillo JM, McCredie KB, Gehan EA, Freireich EJ . Cytogenetic pattern in acute myelogenous leukemia: a major reproducible determinant of outcome Leukemia 1998 2: 403–412
Lange BJ, Kobrinsky N, Barnard DR, Arthur DC, Buckley JD, Howells WB, Gold S, Sanders J, Neudorf S, Smith FO, Woods WG . Distinctive demography, biology, and outcome of acute myeloid leukemia and myelodysplastic syndrome in children with Down syndrome: Children's Cancer Group studies 2861 and 2891 Blood 1998 91: 608–615
Lowenberg B, Downing JR, Burnett A . Acute myeloid leukemia New Engl J Med 1999 341: 1051–1062
Wang J, Hoshino T, Redner R, Kajigaya S, Liu J . ETO, fusion partner in t(8;21) acute myeloid leukemia, represses transcription by interaction with the human N-Cor/mSin3/HDACI complex Proc Natl Acad Sci USA 1998 95: 10860–10865
Shurtleff SA, Buijs A, Behm FG, Rubinitz JE, Raimondi SC, Hancock ML, Chan GC, Pui CH, Grosveld G, Downing JR . Tel/AML1 fusion resulting from cryptic t(12;21) is the most common genetic lesion in pediatric ALL and defines a subgroup of patients with an excellent prognosis Leukemia 1995 9: 1985–1989
Taub J, Huang X, Matherly L, Stout M, Buck S, Massey G, Becton D, Chang M, Weinstein H, Ravindranath Y . Expression of chromosome 21-localized genes in acute myeloid leukemia: differences between down syndrome and non-down syndrome blast cells and relationship to in vitro sensitivity to cytosine arabinoside and daunorubicin Blood 1999 94: 1383–1400
Wang J, Saunthararajah Y, Redner R, Liu J . Inhibitors of histone deacetylase relieve ETO-mediated repression and induce differentiation of AMLI-ETO leukemia cells Cancer Res 1999 59: 2766–2769
Kosugi H, Towatari M, Hatano S, Kitamura K, Kiyo H, Kinoshita T, Tanimoto M, Murate T, Kawashima K, Saito H, Naoe T . Histone deacetylase inhibitors are the potent inducer/enhancer of differentiation in acute myeloid leukemia: a new approach to anti-leukemia therapy Leukemia 1999 13: 1316–1327
Acknowledgements
We thank JC Jones for editorial assistance and, Julie Nucci, Martha Sopfe and Pearl Barber for secretarial assistance. The participating Pediatric Oncology Group (POG) institutions and their Principal Investigators are listed in the appendix. This work was supported in part by Grants from the National Institute of Health and the National Cancer Institute, Bethesda, MD (CA-30969, CA-29139, CA-31566, CA-29691, CA-25408, CA-32053, CA-03161, CA-29293, CA-41573, CA-21765) and the American Lebanese Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Chang, M., Raimondi, S., Ravindranath, Y. et al. Prognostic factors in children and adolescents with acute myeloid leukemia (excluding children with Down syndrome and acute promyelocytic leukemia): univariate and recursive partitioning analysis of patients treated on Pediatric Oncology Group (POG) Study 8821. Leukemia 14, 1201–1207 (2000). https://doi.org/10.1038/sj.leu.2401832
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2401832
Keywords
This article is cited by
-
Epigenetic heterogeneity affects the risk of relapse in children with t(8;21)RUNX1-RUNX1T1-rearranged AML
Leukemia (2018)
-
Hemophagocytic syndrome in children with acute monoblastic leukemia—another cause of fever of unknown origin
Supportive Care in Cancer (2013)
-
Identification and characterization of novel AML1-ETO fusion transcripts in pediatric t(8;21) acute myeloid leukemia: a report from the Children's Oncology Group
Oncogene (2008)
-
Recent advances in management of acute myeloid leukemia (AML)
The Indian Journal of Pediatrics (2008)
-
Postremission therapy for children with acute myeloid leukemia: the children's cancer group experience in the transplant era
Leukemia (2005)