Abstract
OBJECTIVE:
This study was designed to identify risk factors for nosocomial infections among infants admitted into eight neonatal intensive care units in Colombia. Knowledge of modifiable risk factors could be used to guide the design of interventions to prevent the problem.
STUDY DESIGN:
Data were collected prospectively from eight neonatal units. Nosocomial infection was defined as culture-proven infection diagnosed after 72 hours of hospitalization, resulting in treatment with antibiotics for >3 days. Associations were expressed as odds ratios. Logistic regression was used to adjust for potential confounders.
RESULTS:
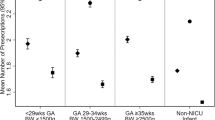
From a total of 1504 eligible infants, 80 were treated for 127 episodes of nosocomial infection. Logistic regression analysis identified the combined exposure to postnatal steroids and H2-blockers, and use of oral gastric tubes for enteral nutrition as risk factors significantly associated with nosocomial infection.
CONCLUSION:
Nosocomial infections in Colombian neonatal intensive care units were associated with modifiable risk factors including use of postnatal steroids and H2-blockers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD. Neonatal Research Network. Pediatrics 2002;110:285–291.
Beck-Sague CM, Azimi P, Fonseca SN, et al. Bloodstream infections in neonatal intensive care unit patients: results of a multicenter study. Pediatr Infect Dis J 1994;13:1110–1116.
Gaynes RP, Edwards JR, Jarvis WR, et al. and the National Nosocomial Infections Surveillance System. Nosocomial infections among neonates in high risk nurseries in the United States. Pediatrics 1996;98:357–361.
Sohn AH, Garrett DO, Sinkowitz-Cochran RL, et al. and the Pediatric Prevention Network. Prevalence of nosocomial infections in neonatal intensive care unit patients: results from the first national point-prevalence survey. J Pediatr 2001;139:821–827.
Weinsten RA . Nosocomial infection update. Emerg Infect Dis 1998;4:416–420.
Mahieu LM, Buitenweg N, Beutels, De Dooy JJ . Additional hospital stay and charges due to hospital-acquired infections in a neonatal intensive care unit. J Hosp Infect 2001;47:223–229.
Moro ML, De Toni A, Stolfi I, Carrieri MP, Braga M, Zunin C . Risk factors for nosocomial sepsis in newborn intensive and intermediate care units. Eur J Pediatr 1996;155:315–322.
Bilal NE, Gedebou M, Al-Ghamdi . Endemic nosocomial infections and misuse of antibiotics in a maternity hospital in Saudi Arabia. APMIS 2002;110:140–147.
Efird M, Rojas MA, Lozano JM, et al. Epidemiology of nosocomial infection in selected neonatal intensive care units in Colombia S-A Colombian Neonatal Research Network. J Perinatol 2005;25:531–536.
Rubin DB, Schenker N . Multiple imputation in health-care databases: an overview and some applications. Stat Med 1991;10:585–598.
Mäki M, Ruuska T, Kusuusela AL, Karikoski-Leo R, Ikonen RS . High prevalence of asymptomatic esophageal and gastric lesions in preterm infants in intensive care. Crit Care Med 1993;21:1863–1867.
Garvey BM, McCamblley JA, Tuxen DV . Effects of gastric alkalinization on bacterial colonization in critically ill patients. Crit Care Med 1989;17:211–216.
Apte NM, Karnad DR, Medhekar TP, Tilve GH, Morye S, Bhave GG . Gastric colonization and pneumonia in intubated critically ill patients receiving stress ulcer prophylaxis: a randomized, controlled trial. Crit Care Med 1992;20:590–593.
Dinsmore JE, Richard JJ, Smith SD . The protective role of gastric acidity in neonatal bacterial translocation. J Pediatr Surg 1997;32:1014–1016.
Cothran DS, Borowitz SM, Sutphen JI, Dudley SM, Donowitz LG . Alteration of normal gastric flora in neonates receiving ranitidine. J Perinatol 1997;17:383–388.
Stark AR, Carlo WA, Tyson JE, et al. Adverse effects of early dexamethasone treatment in extremely low birth weight infants. N Engl J Med 2001;344:95–101.
O’Neil EA, Chwals WJ, O’Shea MD, Turner CS . Dexamethasone treatment during ventilator dependency: possible life threatening gastrointestinal complications. Arch Dis Child 1992;67:10–11.
Harrison H . Preemies on steroids: a new iatrogenic disaster? Birth 2001;28:57–59.
Mayall CG, Lamb VA, Bitar CM . Nosocomial infection in a neonatal unit. Risk factors for gastrointestinal colonization. Infect Control 1980;1:239–246.
Avila-Figueroa C, Golman DA, Richardson DK, Gray JE, Ferrari A, Freemann J . Intravenous lipid emulsions are the major determinant of cagulase-negative staphylococcal bacteremia in very low birth weight newborns. Pediatr Infect Dis J 1998;17:10–17.
Nagata E, Brito AS, Matsuo T . Nosocomial infections in a neonatal intensive care unit: incidence and risk factors. Am J Infect Control 2002;30:26–31.
Grupo Collaborativo Neocosur. Low-birth-weight infant outcomes in 11 South American NICUs. J Perinatol 2002;22:2–7.
Kawagoe JY, Segre CA, Pereira CR, Cardoso MF, Silva CV, Fukushima JT . Risk factors for nosocomial infections in critically ill newborns: a 5-year prospective cohort study. Am J Infect Control 2001;20:109–114.
McCormack JC, Barnes M . Nosocomial infection in a developing Middle East hospital. Infect Control 1983;4:33–36.
Acknowledgements
This study was supported by Forest Pharmaceuticals, Inc., The Institute of Latin American Studies, University Center for International Studies (UCIS) and The Tinker Foundation of the University of North Carolina. We thank physicians and nurses involved in data collection from Hospital Universitario San Ignacio, Fundacíon Santa Fe de Bogotá, Clínica San Pedro Claver, Fundacíon Valle de Lilli, Hospital Universitario Clínica San Rafael, Clínica del Country, Hospital Simon Bolivar and Centro Policlínico del Olaya. Our gratitude to Esperanza Peña RN, MSc., for the coordination of this study.
Author information
Authors and Affiliations
Consortia
Additional information
Research supported in part by Forest Pharmaceuticals, Inc., The Institute of Latin American Studies (ILAS), University Center for International Studies (UCIS), and The Tinker Foundation of the University of North Carolina, Chapel Hill
Rights and permissions
About this article
Cite this article
Rojas, M., Efird, M., Lozano, J. et al. Risk Factors for Nosocomial Infections in Selected Neonatal Intensive Care Units in Colombia, South America. J Perinatol 25, 537–541 (2005). https://doi.org/10.1038/sj.jp.7211353
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211353
This article is cited by
-
Epidemiology of neonatal infections in hospitals of Nepal: evidence from a large- scale study
Archives of Public Health (2020)
-
Molecular epidemiology of carbapenem resistant gram-negative bacilli from infected pediatric population in tertiary - care hospitals in Medellín, Colombia: an increasing problem
BMC Infectious Diseases (2016)
-
International collaborative research: a Colombian model that promotes infant health and research capacity
Journal of Perinatology (2007)