Abstract
Aim To determine the ability of frequency doubling technology (FDT) perimetry to detect visual field defects of neurological origin.
Methods A total of 15 eyes of nine patients who all had complete hemianopias or quadrantanopias underwent the FDT 20-5 screening mode test and Humphrey 24-2 SITA Fast visual field test (HFA). The FDT results were scored according to the number of abnormal test locations (out of a maximum of 4) in each affected quadrant. FDT locations showing a defect of P<2% were considered abnormal.
Results Of the 15 eyes, six showed complete superior quadrantanopic and nine complete hemianopic field defects on HFA. Of 96 FDT test locations in these quadrants or hemifields only 38 were abnormal on FDT testing (40%). For the quadrantanopic field defects, five out of 24 locations were abnormal (21%). For the hemianopic field defects, 33 out of 72 locations were abnormal (49%). In three eyes (two with quadrantanopias and one with complete hemianopia), FDT perimetry failed to demonstrate any corresponding abnormality.
Conclusions The FDT screening test can fail to demonstrate complete hemianopic and quadrantanopic field defects. Users should be aware of this deficiency when using FDT to screen for field defects.
Similar content being viewed by others
Introduction
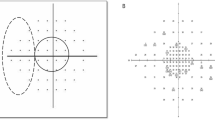
The frequency-doubling technology (FDT) instrument is a recently introduced visual field test for glaucoma. It utilises the frequency-doubling illusion, in which a sine wave grating of low spatial frequency undergoing counterphase flicker at high temporal frequency appears to the observer to have double the number of bars than are actually present.1 This psychophysical ‘illusion’ is thought to be mediated by My ganglion cells that are a subset of the magnocellular system.2 The FDT has shown high sensitivity and specificity in identifying patients with glaucomatous visual field loss and has been advocated as a suitable screening test for glaucoma3,4 (Figure 1).
We have seen a number of cases where dense visual field defects of ‘neurological’ origin have not been detected by FDT. We are not aware of any reports of this in the literature. This study therefore aimed to assess the ability of the FDT to detect visual field defects of ‘neurological’ rather than glaucomatous origin.
Subjects and methods
Informed consent was obtained from each patient after a full explanation of the test. Subjects with known field defects secondary to cerebral vascular events or cerebral tumours were recruited. The type of lesion and location of the lesion were diagnosed by computed tomography of the head. Each had repeatable and reliable field defects demonstrable with the Humphrey 24-2 SITA Fast visual field test (HFA). All had complete quadrantanopias or hemianopias confirmed by Humphrey 24-2 visual field testing and had intraocular pressures less than 22 mmHg, healthy optic discs and no significant retinal or other ocular pathology. A total of 15 eyes of nine patients underwent the FDT C20-5 screening mode test. The remaining three eyes had limited visual acuity from other causes and could not perform the tests.
The FDT C20-5 screening mode tests four locations in each quadrant and one central location, giving a total of 17 locations within the central 20° of visual field. Each test stimulus is a series of white and black bands that flicker at 25 Hz. The FDT results were scored according to the number of abnormal test locations (out of 4) in each quadrant and were compared with the corresponding quadrantanopia or hemianopia seen on HFA. FDT locations with P<2% were considered abnormal.
Results
Of the 15 eyes tested, six showed complete superior temporal quadrantanopic and nine had complete homonymous hemianopic field defects on HFA (Table 1) (Figure 2 and Figure 3). The field defects all extended to the centre of fixation, ie within the area being tested by the HFA and FDT. Of a possible maximum of 96 test locations within these quadrants and hemifields, only 38 showed a significant defect (40%). For the quadrantanopias, only five out of a possible 24 locations (21%) showed a defect. For the eyes with hemianopias, 33 out of a possible 72 locations (49%) showed a defect on the FDT. In three eyes (two eyes with complete quadrantanopias and one eye with complete hemianopia), no corresponding abnormal test locations were present. All the tests done met the manufacturer's criteria for reliability.
Discussion
This study demonstrated that FDT perimetry is poor at detecting field defects of neurological origin as less than half of the FDT locations analysed detected defects seen on HFA. While many of the patients showed some degree of defect on FDT, it was worrying that others with complete quadrantanopias confirmed by threshold perimetry showed no defect at all on FDT.
The most likely reason for the failure of these defects to be demonstrated is that the large flickering stimuli used by the FDT extend as far as the vertical and horizontal axis rather than being offset as in the Humphrey-2 programmes. Scattered light from these stimuli could thus be seen by the patient on the edge of the normally functioning visual field. This is suggested by the fact that Woodward and co-workers5,6 found that the sensitivity of detecting such field defects was improved by offsetting the stimulus along the vertical meridian by 3° with no increase in variability in the damaged hemifield compared to the normal one.
Another possible explanation for the failure of FDT to pick up neurological visual field defects is the phenomenon of blindsight.7 This phenomenon, first described by Riddoch in 1917, is the apparent ability of patients with blind visual fields from cortical lesions to detect movement in their blind visual fields. Blindsight is characterised by a failure to detect targets presented during HFA, while maintaining the ability to detect briefly presented, flickering or moving stimuli.8 Whether or not a patient has blindsight appears to depend on the amount of occipital cortex spared, a total lesion of occipital cortex leading to total blindness.9 However, what is interesting is that, although blindsight patients can ‘see’ in a rudimentary way, they are not consciously aware of having seen anything at all. The magnocellular pathways that project to the superior colliculus and then to extrastriate cortical areas via the pulvinar are commonly assumed to mediate blindsight-type responses.10 That such a pathway may exist in the human brain and that signals presented in the blind field actually reach the cortex is suggested by evidence which shows that, when visual stimuli are presented to the blind field of blindsight patients, evoked potentials can be picked up directly from the cortex.9
It is essential that good fixation is maintained during visual field testing, and one of the weaknesses of the FDT test in the screening mode is that fixation is only tested 3 times during the test. Poor fixation during testing could account for the fact that FDT stimuli could apparently be seen by the blind hemifield. Additionally, Nicholas et al11 found that FDT perimetry in the screening mode was less sensitive at detecting such field defects compared to the full threshold mode. The FDT test in full threshold mode tests for fixation 6 times during the test.
Although the FDT is a useful test for screening for glaucomatous visual field defects, it is clear that in its current form, it does not reliably detect even gross neurological visual field defects extending to fixation. This limitation is potentially important when reporting that a patient has a ‘normal’ field of vision when assessed by the FDT. Both community optometrists and hospital ophthalmic departments should be aware of this limitation when testing patients with possible neurologic disease for glaucomatous field defects.
References
Kelly DH . Frequency doubling in visual responses. J Opt Soc Am A. 1966; 56: 1628–1633.
Johnson CA, Samuels SJ . Screening for glaucomatous visual field loss with frequency-doubling perimetry. Invest Ophthalmol Vis Sci. 1997; 38(2): 413–425.
Alward WLM . Frequency doubling technology perimetry for the detection of glaucomatous visual field loss. Am J Ophthalmol 2000; 129(3): 376–377.
Quigley HA . Identification of glaucoma-related visual field abnormality with the screening protocol of frequency doubling technology. Am J Ophthalmol 1998; 125: 819–828.
Woodward K, Brito CF, Wall M . Variability of FDT perimetry: effect of a 3 degree offset along the vertical in patients with hemianopias and normals. Invest Ophthalmol Vis Sci 2001; 42(4): S150. Abstract 803.
Wall M, Newman S, Johnson C, Fingeret M, Maxner C, Woodward K . Improvement of sensitivity of FDT perimetry to detect hemianopias with a 3 degree stimulus offset along from the vertical. Invest Ophthalmol Vis Sci 2001; 42(4): S153 Abstract 820.
Zeki S . A Vision of the Brain. Blackwell Scientific Publications: Oxford, 1993, pp 347–350.
Morland AB, Jones SR, Finlay AL, Deyzac E, Le S, Kemp S . Visual perception of motion, luminance and colour in a human hemianope. Brain 1999; 122: 1183–1198.
Celesia GG, Bushnell D, Toleikis SC, Brigell MG . Cortical blindness and residual vision: is the ‘second’ visual system in humans capable of more than rudimentary visual perception? Neurology 1991; 41: 862–869.
Weiskrantz L . In: Mackintosh NJ, Shallice T, Schacter D, Treisman A, Weiskrantz L (eds). Blindsight: A Case Study and Implications. Oxford University Press: Oxford, 1986.
Nicholas JA, Wall M, Newman S, Johnson C, Fingeret M, Maxner C et al. Sensitivity of FDT perimetry screening tests compared with full threshold testing in patients with homonymous hemianopias. Invest Ophthalmol Vis Sci 2001; 42(4): S150. Abstract 800.
Acknowledgements
The authors are grateful to Mr Nigel Davies and Dr Tony Morland for their helpful comments on the paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the Oxford Ophthalmological Congress 2001
Rights and permissions
About this article
Cite this article
Fong, K., Byles, D. & Constable, P. Does frequency doubling technology perimetry reliably detect neurological visual field defects?. Eye 17, 330–333 (2003). https://doi.org/10.1038/sj.eye.6700376
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700376
Keywords
This article is cited by
-
Using frequency-doubling perimetry to detect optic neuropathy in patients with Graves’ orbitopathy
Japanese Journal of Ophthalmology (2008)
-
Clinical assessment of optic nerve disorders
Eye (2004)