Abstract
Objective: To determine the extent and causes of iodine deficiency among women during pregnancy and lactation in the southeastern plains of Nepal.
Design, Setting and Subjects: Urinary iodine (UI) was assessed as an indicator of iodine status in spot urine samples of women participating in a field trial in three rural communities in the plains of southeastern Nepal. Samples were collected during pregnancy (n=1021) and during lactation at 3–4 months postpartum (n=1028) at a central clinic; 613 women were assessed at both times. Salt iodine (SI) content was assessed semiquantitatively at 6–7 months postpartum in households (n=1572).
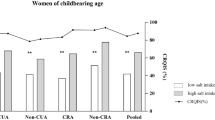
Results: During pregnancy and lactation, median UI concentrations were 0.756 and 0.483 μmol/l, respectively, indicating mild iodine deficiency. UI and SI concentrations covaried markedly by season and were highest during hot, dry, premonsoon months and lowest during and following the humid monsoon season. Within women who contributed urine samples during both pregnancy and the postpartum period, iodine status determined by UI was not correlated. The percentage of households with adequately iodized salt (30 ppm) ranged from 85 to 44% from the hot, dry to the humid seasons, respectively.
Conclusions: In the rural southern plains of Nepal, iodine deficiency remains a mild-to-moderate public health problem among pregnant and lactating women despite the availability of iodized salt. Marked seasonality in SI content may account for the lack of intraindividual correlation between maternal iodine status during pregnancy and postpartum periods and contribute to periodicity in the risk of iodine deficiency.
Sponsorship: This study was funded by Cooperative Agreement HRN-A-00-97-00015-00 between Office of Nutrition, US Agency for International Development (USAID), Washington, DC, USA, and the Center for Human Nutrition (CHN), Department of International Health, the Bill and Melinda Gates Foundation, Seattle, WA, USA, and the Sight and Life Research Institute, Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, USA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Aboul-Khair SA, Crooks J, Turnbull AC & Hytten FE (1964): The physiological changes in thyroid function during pregnancy. Clin. Sci. 27, 195–207.
Azizi F, Kalani H, Kimiagar M, Ghazi A, Sarshar A, Nafarabadi M, Rahbar N, Noohi S, Mohajer M & Yassai M (1995): Physical, neuromotor and intellectual impairment in non-cretinous schoolchildren with iodine deficiency. Int. J. Vitam. Nutr. Res. 65, 199–205.
Bohles H, Aschenbrenner M, Roth M, Loewenich Vv, Ball F & Usadel KH . (1993): Development of thyroid gland volume during the first 3 months of life in breast-fed versus iodine-supplemented and iodine-free formula-fed infants. Clin. Invest. 71, 13–20.
Brabant G, Bergmann P, Kirsch CM, Kohrle J, Hesch RD & von zur Muhlen A (1992): Early adaptation of thyrotropin and thyroglobulin secretion to experimentally decreased iodine supply in man. Metabolism 10, 1093–1096.
Brown-Grant K (1961): Extrathyroidal iodine concentrating mechanisms. Physiol. Rev. 41, 189–213.
Caron P, Hoff M, Bazzi S, Dufor A, Faure G, Ghandour I, Lauzu P, Lucas Y, Maraval D, Mignot F, Ressigeac P, Vertongen F & Grange' V (1997): Urinary iodine excretion during normal pregnancy in healthy women living in the Southwest of France: correlation with maternal thyroid parameters. Thyroid 7, 749–754.
Chaouki ML & Benmiloud M (1994): Prevention of iodine deficiency disorders by oral administration of lipiodol during pregnancy. Eur. J. Endocrinol. 130, 547–551.
Clugston GA, Dulberg EM, Pandav CS & Tilden RL (1987): Iodine deficiency disorders in South East Asia. In BS Hetzel, JT Dunn & JB Stanbury, eds, The Prevention and Control of Iodine Deficiency Disorders, Amsterdam: Elsevier Science Publishers B.V. (Biomedical Division).
Cobra C, Muhilal, Rusmil K, Rustama D, Djatnika, Suwardi SS, Permaesih D, Muherdiyantiningsih M, Martuti S & Semba RD (1997): Infant survival is improved by oral iodine supplementation. J. Nutr. 127, 574–578.
Dahal BR (1993): Goitre and iodine nutriture status of primary school children in Ilam District, Nepal. J. Nep. Med. Assoc. 31, 340–347.
Delange F, Bourdoux P, Chanoine JP & Ermans AM (1988): Physiopathology of iodine nutrition during pregnancy, lactation, and early postnatal life. In Vitamins and Minerals in Pregnancy and Lactation, Nestle' Nutrition Workshop Series, Vol 16, ed H Berger. New York: Raven Press, Ltd.
Dillon JC & Milliez J (2000): Reproductive failure in women living in iodine deficient areas of West Africa. Br. J. Obstet. Gynaecol. 107, 631–636.
Diosady LL, Alberti MG, Manner V & Stone TG (1997): Stability of iodine in iodized salt used for correction of iodine-deficiency disorders. Food Nutr. Bull. 18, 388–396.
Dreyfuss ML, Stoltzfus RJ, Shrestha JB, Pradhan EK, LeClerq SC, Khatry SK, Shrestha SR, Katz J, Albonico M & West Jr KP (2000): Hookworms, malaria and vitamin A deficiency contribute to anemia and iron deficiency among pregnant women in the plains of Nepal. J. Nutr. 130, 2527–2536.
Dunn JT, Crutchfield HE, Gutekunst R & Dunn AD (1993): Two simple methods for measuring iodine in urine. Thyroid 3, 119–123.
Dworkin HJ, Jacquez JA & Beierwaltes WH (1966): Relationship of iodine ingestion to iodine excretion in pregnancy. J. Clin. Endocrinol. 26, 1329–1342.
Elnager B, Eltom A, Wide L, Gebre-Medhin M & Karlsson FA (1998): Iodine status, thyroid function and pregnancy: study of Swedish and Sudanese women. Eur. J. Clin. Nutr. 52, 351–355.
Eltom A, Eltom M, Elnagar B, Elbagir M & Gebre-Medhin M (2000): Changes in iodine metabolism during late pregnancy and lactation: a longitudinal study among Sudanese women. Eur. J. Clin. Nutr. 54, 429–433.
Fierro-Benitez R, Cazar R, Stanbury JB, Rodriguez P, Garces F, Fierro-Renoy F & Estrella E (1988): Effects on school children of prophylaxis of mothers with iodized oil in an area of iodine deficiency. J. Endocrinol. Invest. 11, 327–335.
Gardezi SMA (1994): Iodine Deficiency Disorders Prevalence Survey Azad Jammu & Kashmir. New York: UNICEF.
Glinoer D (1997): The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocrine Rev. 18, 404–433.
Glinoer D & Delange F (2000): The potential repercussions of maternal, fetal, and neonatal hypothyroxinemia on the progeny. Thyroid 10, 871–887.
Glinoer D, DeNayer P, Delange F, Lemone M, Toppet V, Spehl M, Grun J-P, Kinthaert J & Lejeune B (1995): A randomized trial for the treatment of mild iodine deficiency during pregnancy: maternal and neonatal effects. J. Clin. Endocrinol. Metab. 80, 258–269.
Gushurst CA, Mueller JA, Green JA & Sedor F (1984): Breast milk iodide: reassessment in the 1980s. Pediatrics 73, 354–357.
Harris T (1950): Regression using minimum absolute deviations. Am. Statist. 4, 14–15.
Kung AWC, Lao TT, Low LCK, Pang RWC & Robinson JD (1997): Iodine insufficiency and neonatal hyperthyrotropinaemia in Hong Kong. Clin. Endocrinol. 46, 315–319.
Mannar VMG & Dunn JT (eds) (1995): Salt Iodization for the Elimination of Iodine Deficiency, Netherlands International Council for the Control of Iodine Deficiency Disorders. Geneva: World Health Organization.
Marine D & Kimball OP (1920): The prevention of simple goiter in man. Arch. Intern. Med. 25, 661–672.
Micronutrient Deficiency Information System Project, WHO Nutrition Unit (1993): Global Prevalence of Iodine Deficiency Disorders. Geneva: World Health Organization.
Ministry of Health, His Majesty's Government, Nepal (1997): Demographic and Health Surveys: Nepal Family Health Survey 1996. Calverton, MD: Macro International Inc.
Nepal Micronutrient Status Survey (1998): Kathmandu, Nepal: Ministry of Health, Child Health Division, HMG/N, New ERA, Micronutrient Initiative, UNICEF Nepal, and World Health Organization.
Pedersen KM, Laurberg P, Iversen E, Knudsen PR, Gregersen HE, Rasmussen OS, Larsen KR, Eriksen GM & Johannesen PL (1993): Amelioration of some pregnancy-associated variations in thyroid function by iodine supplementation. J. Clin. Endocrinol. Metab. 77, 1078–1083.
Pharoah POD (1972): The clinical pattern of endemic cretinism in Papua New Guinea. J. Exp. Med. Biol. 30, 71–82.
Pharoah POD, Buttfield IH & Hetzel BS (1971): Neurological damage to the fetus with severe iodine deficiency during pregnancy. Lancet i, 308–310.
Pharoah POD & Connolly KJ (1987): A controlled trial of iodinated oil for the prevention of endemic cretinism: a long-term follow-up. Int. J. Epidemiol. 16, 68–73.
Pino S, Fang SL & Braverman LE (1996): Ammonium persulfate: a safe alternative oxidizing reagent for measuring urinary iodine. Clin. Chem. 42, 239–243.
Pongpaew P, Tungtrongchitr R, Vudhivai N, Kitjaroentham A, Intarakhao C, Saowakhontha S, Supawan V, Phonrat B, Chantaranipapong Y, Jintaridhi P, Mahaweerawat U & Schelp FP (1999): Urinary iodine excretion as a predictor of the iodine content of breast milk. J. Med. Assoc. Thai. 82, 284–289.
Sandell EB & Kolthoff M (1937): Micro determination of iodine by a catalytic method. Mikrochem. Acta 1, 9–25.
Smyth PPA (1999): Variation in iodine handling during normal pregnancy. Thyroid 9, 637–642.
Smyth PPA, Hetherton AMT, Smith DF, Radcliff M & O'Herlihy C (1997): Maternal iodine status and thyroid volume during pregnancy: correlation with neonatal intake. J. Clin. Endocrinol. Metab. 82, 2840–2843.
Wang GY, Zhou RH, Wang Z, Shi L & Sun M (1999): Effects of storage and cooking on the iodine content in iodized salt and study on monitoring iodine content in iodized salt. Biomed. Environ. Sci. 12, 1–9.
West KP, Katz J, Khatry SK, LeClerq SC, Pradhan EK, Shrestha SR, Connor PB, Dali SM, Christian P, Pokhrel RP & Sommer A (1999): Double blind, cluster randomized trial of low dose supplementation with vitamin A or β carotene on mortality related to pregnancy in Nepal. BMJ 318, 570–575.
WHO/UNICEF/ICCIDD (1994): Indicators for Assessing Iodine Deficiency Disorders and their Control through Salt Iodization. Geneva: World Health Organization (WHO/NUT/94.6).
Xue-Yi C, Xin-Min J, Zhi-Hong D, Rakeman MA, Ming-Li Z, O'Donnell K, Tai M, Amette K, DeLong N & DeLong R (1994): Timing of vulnerability of the brain to iodine deficiency in endemic cretinism. N. Engl. J. Med. 331: 1739–1744.
Acknowledgements
The authors gratefully acknowledge contributions from other members of the study team: Joanne Katz, Parul Christian, Elizabeth Kimbrough-Pradhan, Sharada Ram Shrestha, Ramesh K Adhikari, Samu M Dali, Tirta Shakya, and field and data management staff of the Nepal Nutrition Intervention Project—Sarlahi (NNIPS).
Author information
Authors and Affiliations
Contributions
Guarantor: KP West, Jr.
Contributors: KJS developed urinary iodine assay in Nepal, analyzed data, prepared manuscript. KPW Jr assisted in conceptualization of study and interpretation of data. LAG analyzed samples and maintained quality control of urinary iodine assay in Kathmandu laboratory. MLD managed the recruitment of women into the study and data collection activities in the clinic. SCLC supervised collection of salt iodine samples and interpreted findings. BRD served as iodine-deficiency consultant and regularly oversaw urinary iodine analyses in Kathmandu laboratory. LS-FW managed and assisted in analyzing data and interpreting results. SKK served as national principal investigator of the study, providing medical supervision of field work.
Corresponding author
Rights and permissions
About this article
Cite this article
Schulze, K., West, K., Gautschi, L. et al. Seasonality in urinary and household salt iodine content among pregnant and lactating women of the plains of Nepal. Eur J Clin Nutr 57, 969–976 (2003). https://doi.org/10.1038/sj.ejcn.1601632
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601632
Keywords
This article is cited by
-
Probabilistic Health Risk Assessment of Iodine Exposure in Bangladesh
Biological Trace Element Research (2023)
-
Need for an Individualized and Aggressive Management of Multinodular Goiters of Endemic Zones by Specially Trained Surgeons: Experience in Western Nepal
World Journal of Surgery (2006)