Abstract
The elevation of soluble Fas (sFas) in the sera of patients with liver disease suggests a role for sFas in the disease process; whether it is protective or not is controversial. To determine the effects of sFas on Fas-induced liver apoptosis, we manipulated mice to produce sFas by transfecting them in vivo with different amounts of an adenovirus that produces mouse sFas driven by the CMV promoter (AdsFas). Fas-mediated apoptosis was induced by administration of anti-mouse Fas (Jo2; 10 μg/mouse) one week later. The administration of AdsFas (103, 107, or 109 pfu/mouse), which was associated with only minimal side-effects, resulted in a significant reduction in the liver transaminase levels and mortality of the mice on challenge with Jo2, as compared to control mice treated with AdLacZ. However, the protective effect of AdsFas was not complete. The possibility that Jo2-induction of TNF-α in the Kupffer cells of the liver contributes to the pathology was therefore tested. Although administration of soluble TNF receptor (sTNFRI) alone did not protect the mice from the lethal effects of Jo2, administration of sTNFRI (200 μg/mouse) after infection with AdsFas (109 pfu/mouse) resulted in 100% survival of the mice on challenge with Jo2. To confirm that the production of TNF-α by Kupffer cells produce the lethal effects of Jo2 that remained after treatment with AdsFas, these cells were selectively ablated by treatment of the mice with gadolinium chloride prior to challenge with Jo2. This treatment greatly reduced early mortality and hepatocellular damage as well as TNF-α production 6 h after injection of Jo2. These results indicate that: (1) AdsFas prevents Jo2-induced apoptosis of hepatocytes; (2) In addition to mediating Fas-mediated apoptosis of hepatocytes, Jo2 can separately induce TNF-α production by Kupffer cells resulting in early mortality, and (3) Optimal protection from Jo2-induced mortality can be achieved by protection of liver cells by pretreatment with both AdsFas and sTNFRI.
Similar content being viewed by others
Introduction
Fas/APO-1 (CD95), an apoptosis-signaling receptor molecule, is expressed on the surface of a number of cell types including liver parenchymal,1 endothelial,2,3 and Kupffer cells.4,5 The molecular biology of Fas-mediated apoptosis is now well described. Fas triggers apoptosis through a 90-amino acid cytoplasmic death domain (amino acids 201–292).6,7 Upon trimerization of the receptor by its ligand (FasL), this death domain forms a death inducing signaling complex (DISC). This complex acts to dock adapter and signaling molecules that signal apoptosis, including the Fas-associated protein with death domain (FADD or MORT1),8,9,10,11 which then recruits FADD-like ICE (FLICE; now referred to as caspase 8)12,13 that triggers the cascade of events that results in programmed cell death.
The process of apoptosis is regulated tightly through a variety of mechanisms, one of which is postulated to be the production of soluble forms of Fas (sFas) that normally binds to FasL, thus blocking the signaling of the membrane-bound form of Fas.14 In humans, sFas is normally present at serum levels of 0.1–1.0 ng/ml.14,15 Molecular cloning and nucleotide sequence analyses have revealed several Fas mRNA splice variants that encode the soluble forms of the Fas molecule.16 The most abundant of these is FasΔTM, which encodes the sFas molecule that exhibits alternative splicing and deletion of exon 6 of the transmembrane domain.14,17 It has been shown in vitro that supernatants from cells transfected with FasΔTM block apoptosis induced by either FasL or Fas antibody.14,17 The role of sFas in protection of cells from apoptosis in vivo has not yet been established.
The cells of the liver, including the parenchymal and Kupffer cells, constitutively express Fas and are highly sensitive to apoptosis induced by anti-Fas antibody.18,19 Fas-mediated apoptosis has been implicated as a contributing factor in liver damage. It has been established that FasL is elevated in the sera of patients with liver diseases, including chronic hepatitis B and hepatitis C, autoimmune hepatitis, and cirrhosis, and in patients with hepatocellular damage resulting from liver transplantation or toxins.18,19,20,21,22,23,24 Biopsy samples show high levels of apoptosis in the livers of patients with chronic hepatitis B and hepatitis C.20,25,26 It also has been established that sFas is elevated in the sera of patients with these liver diseases or hepatocellular damage.18,19,20,21,22,2324 Additionally, we have observed high levels of sFas in the sera of patients with SLE,15,16 and these high levels showed a significant correlation with elevated levels of indicator liver enzymes15 as well as the Systemic Lupus International Collaborative Clinics/American College of Rheumatology Damage Index (SLICC/ACR).27 In all of the above studies, it is notable that the elevations in the levels of sFas are seen in situations in which there is ongoing liver damage. Consequently, it remains controversial as to whether or not sFas, either produced naturally or administered exogenously, is capable of protecting the liver from Fas-mediated apoptosis.
This issue has proven difficult to resolve due, in part, to the lack of an informative experimental animal model. Mice do not produce sFas. Therefore, we investigated the effects of sFas by infecting mice with adenovirus expressing sFas (AdsFas). Infection with AdsFas and consequent production of sFas abrogated the liver damage typically induced by administration of the anti-mouse Fas antibody, Jo2, but did not completely prevent the associated mortality. The observation that administration of Jo2 is associated with an increase in the levels of tumor necrosis factor-α (TNF-α) in the sera, suggested the existence of a pathological mechanism in addition to Fas-mediated apoptosis of the parenchymal cells, which was confirmed by the finding that co-administration of soluble tumor necrosis factor (sTNFRI) with AdsFas provided efficient protection. The source of the Jo2-induced TNF-α was identified as the Kupffer cells by ablation of these cells by pretreatment with gadolinium chloride (GdCl3).28,29 In summary, these data suggest that the Fas-associated liver damage and mortality elicited by Jo2, is mediated by two separate mechanisms. One of these, the Fas-mediated apoptosis of the parenchymal cells, can be readily prevented by sFas. In contrast, Fas-induced TNF-α production by Kupffer cells, is less readily prevented by sFas but is amenable to treatment with sTNFRI.
Results
AdsFas can enhance the survival of mice after administration of anti-Fas antibody (Jo2)
We have previously produced a Fas-Fc fusion protein to produce high levels of soluble Fas-extracellular domain (sFas) to bind to Fas ligand (FasL) and prevent Fas apoptosis in vitro and in vivo.14 For the present studies, the Fas-Fc was cloned into the E1A site of an adenovirus to enable expression of sFas by liver cells in vivo. We first determined whether sFas can protect mice from the lethal effects of administration of anti-Fas antibody, mice were infected with AdsFas (109, 107 and 103 pfu/mouse) or control AdLacZ (109 pfu/mouse) administered i.v. One week later, the mice were challenged with 10 μg/mouse of the anti-Fas antibody Jo2, administered i.p. (Figure 1a). The administration of the Jo-2 antibody was uniformly and rapidly fatal in mice that were untreated or treated with control AdLacZ (109 pfu/mouse), as well as mice treated with the lowest dose of AdsFas (103 pfu/mouse) (Figure 1b). Pretreatment of the mice with either 109 or 107 pfu/mouse of AdsFas enhanced survival significantly (Figure 1b), with the survival rate of mice being higher in the group of mice administered 109 pfu/mouse of AdsFas as compared to mice administered 107 pfu/mouse. It is noteworthy that, in the absence of challenge with Jo2, administration of AdsFas or AdLacZ did not cause the death of any mice (Figure 1b) or any overt signs of adverse effects.
(a) The time-course of the experiment. Mice were pretreated with AdsFas or AdLacZ 1 week before anti-Fas (Jo2) injection. The survival of mice was determined 24 h after Jo2 challenge. (b) Enhanced survival after anti-Fas challenge of mice pretreated with AdsFas. Mice pre-treated with 107, or 109 pfu/mouse of AdsFas show higher survival rates than mice pre-treated with 103 pfu/mouse of AdsFas, 109 pfu/mouse of AdLacZ, or no pre-treatment (all of which died within 6 h of anti-Fas injection). No deaths occurred in the groups of AdsFas- or AdLacZ-treated mice that were not challenged with anti-Fas. Comparisons of the survival among groups were accomplished using Fisher's exact test
AdsFas can prevent hemorrhagic hepatitis induced by administration of anti-Fas antibody (Jo2)
Previously, it has been shown that intravenous injection of anti-Fas antibody results in hemorrhagic liver damage.18 Consistent with this report, histologic analysis of the liver showed that within 3 h of administration of Jo2, the control AdLacZ pre-treated mice exhibited extensive hemorrhagic liver damage (Figure 2a). To determine if the protective effect of AdsFas is associated with amelioration of the hemorrhagic liver damage, mice were pretreated with either 109 or 107 pfu/mouse of AdsFas (Figure 2b,c) one week prior to administration of 10 μg/mouse of Jo2. The histology of the liver was evaluated 6 h later. In contrast to the extensive hemorrhagic hepatitis observed in mice receiving Jo2 without pretreatment, there was greatly reduced hepatitis in the mice that had received pretreatment with AdsFas 1 week prior to receiving Jo2. To determine if the infection with either AdsFas or AdLacZ contributes to the cytopathic effects in the liver, 109 pfu/mouse of AdsFas or 109 pfu/mouse of AdLacZ were injected i.v. in 6-week-old B6 female mice, and the mice were sacrificed 1 week later. Histologic analysis of the liver tissue confirmed that the administration of 109 pfu/mouse of AdLacZ or AdsFas did not result in any significant cytopathic effects (Figure 2d, other results not shown).
Histologic examination of apoptosis in the liver. Sections of formalin-fixed, paraffin-embedded liver were examined by hematoxylin and eosin (H&E) staining (a–d) and Hoechst staining (e–f). Typical features of hemorrhagic liver damage (a) and nuclear condensation (e) were observed in the livers of mice treated with AdLacZ 109 pfu/mouse 1 week prior to i.p. injection with 10 μg/mouse of Jo2. Examination of liver specimens of surviving mice pre-treated with AdsFas at 109 (b,f) and 107 (c,g) pfu/mouse prior to Jo2 challenge revealed either no change or only slight changes 6 h after Jo2 injection. The livers of control mice pretreated with AdLacZ 109 pfu/mouse followed by administration of saline only exhibited no abnormalities (d,h). All livers were obtained 3–6 h after Jo2 or control treatment. Magnification=100×
AdsFas can prevent apoptosis of hepatocytes induced by anti-Fas antibody (Jo2) in vivo
We next addressed the question as to whether the protective effects of AdsFas are mediated through inhibition of apoptosis of liver cells. It has been shown previously that soluble Fas can protect cells from apoptosis in vitro.14 To determine if sFas can protect cells from apoptosis in vivo, nuclear condensation was evaluated in the livers of the mice.30 Extensive nuclear condensation was observed in the livers of mice administered Jo2 after pretreatment with control AdLacZ, confirming that the anti-Fas antibody does induce apoptosis in the liver (10 μg/mouse) (Figure 2e). Pre-treatment with 109 pfu/mouse (Figure 2f) or 107 pfu/mouse (Figure 2g) of AdsFas prior to challenge with mouse Jo2 (10 μg/mouse) resulted in a reduction in the extent of apoptosis with slight nuclear condensation being observed in surviving mice 6 h after the administration of Jo-2. In mice pre-treated with 109 pfu/mouse of AdLacZ or AdsFas that were not challenged with Jo2, nuclear condensation was not observed (Figure 2h, other data not shown). These results indicate that sFas can prevent apoptosis in vivo and suggest that, in these mice, AdsFas is protecting the liver, at least in part, by inhibiting Fas-mediated apoptosis. Notably, even 107 pfu/mouse of AdsFas was effective in inhibiting Fas-mediated apoptosis, as well as the associated hemorrhagic liver damage and death (Figures 1, 2c,g).
AdsFas limits the elevation of liver enzymes in the sera induced by anti-Fas antibody (Jo2) in vivo
Elevated levels of the liver enzymes aspartate amino transferase (AST) and alanine amino transferase (ALT) in the sera are markers of liver damage and have been reported previously in association with Jo2 hepatotoxicity.18 Sera were obtained from the mice at 24 h before and 3 h after injection of Jo2. Twenty-four h before challenge with Jo2, there was no significant difference in the sera levels of either AST or ALT among the three groups of mice that had been pretreated with AdsFas (107 or 109 pfu/mouse) or control AdLacZ (Figure 3a,b, open bars). At 3 h after administration of 10 μg/mouse of Jo2, the levels of both AST and ALT in the sera were increased (Figure 3a,b, closed bars). Mice that were pre-treated with AdsFas (109 pfu/mouse) 1-week prior to Jo2 (10 μg/mouse) challenge exhibited significantly lower levels of AST and ALT compared to mice receiving Jo2 without AdsFas pretreatment. Although the sera from mice pretreated with 107 pfu/mouse of AdsFas exhibited lower levels of AST and ALT compared to mice without pre-treatment, there was no statistical significant difference between these groups. Pre-treatment of mice with 103 pfu/mice of AdsFas and Jo2 resulted in increased levels of both AST and ALT equivalent to that observed in control mice (data not shown). Taken together, these results suggest that pretreatment with AdsFas can enhance resistance to the cytopathic and lethal effects of administration of anti-Fas antibody. The effect is dose-dependent, with 107 pfu/mouse of AdsFas affording some protection. However, not all mice were protected even at a higher dose (109 pfu/mouse).
Serum AST (a) and ALT (b) levels before, and 3 h after, administration of Jo2 anti-Fas antibody. Groups of mice (n=5) were pre-treated with AdsFas (109 or 107 pfu/mouse) or were not pre-treated. Blood samples were collected by eye bleeding before and 3 h after administration of Jo2. The results are presented as the mean±S.E.M. of the results of five different mice in each group. Significant differences in the levels of AST or ALT were observed in AdsFas (109 pfu/mouse) treated mice compared to control-treated mice (P<0.05)
Evaluation of sFas levels in the liver and sera
In an effort to evaluate the levels of sFas after administration of AdsFas, sera were collected and livers obtained from the mice one week after administration of AdsFas (107, 109, or 1010 pfu/mouse) and the levels of sFas quantitated using an ELISA assay. As expected, higher levels of sFas were observed in the liver compared to the sera. The liver is the primary target of adenoviral vectors. One week after administration of 1010 of AdsFas, the levels of AdsFas in the liver and serum were 290±25 ng/ml and 112±8.6 ng/ml, respectively (Figure 4). One week after administration of 109 of AdsFas, the liver and serum concentrations of sFas were 11.0±0.65 ng/mg and less than 1 ng/ml, respectively, and 1 week after administration of 107 of AdsFas, sFas was not detectible in either the liver lysate or the sera (Figure 4). This approach provides an approximate level for sFas in the liver and sera after administration of higher pfu of AdsFas, but the values of sFas in the liver and the sera after administration of lower pfu of AdsFas can only be approximated since they were below the limit of detection by the mouse sFas ELISA assay.
Levels of sFas in the serum and the liver after AdsFas treatment. One week after treatment with AdsFas (1010, 109, or 107 pfu/mouse), the levels of sFas in the sera and the liver lysates were quantitated by ELISA. The results are presented as the mean±S.E.M. of duplicate assays with three mice in each group. *The levels of sFas were below the limit of detection (1.0 ng/ml) of the assay in liver lysates from mice that received 107 pfu of AdsFas, and in the sera of mice that received 109 pfu or 107 pfu of AdsFas
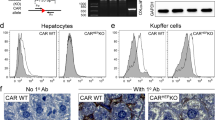
As an alternative approach to evaluating the production of sFas on infection with AdsFas, we assessed the percentage of liver cells that produced sFas as examined by immunohistochemical staining of the liver to determine if many liver cells produce low levels of sFas or if few liver cells produce relatively high levels of sFas. Mice (3 mice/group) were administered AdsFas (109 and 107 pfu/mouse) i.v. One week later, the liver was analyzed for the production of sFas using an anti-human IgG Ab, to detect the Fc portion of the intracellular domain of human IgG1 that is fused with a mouse Fas extracellular domain (Fas-Fc) in the sFas used to produce the AdsFas. In mice treated with 109 pfu of AdsFas, the percentage of cells expressing Fas-Fc was 5% of all liver cells (Figure 5a). In mice treated with 107 pfu of AdsFas, lower numbers of liver cells produced Fas-Fc compared to those treated with 109 pfu (Figure 5b), and were estimated to be approximately 0.05% of all the cells in the liver. Cells expressing Fas-Fc were undetectable in the liver of AdLacZ-treated mice (Figure 5c). These results indicate that relatively low levels of sFas in the liver can partially protect the mice from Jo-2 apoptosis.
Immunohistochemical analysis of sFas expression in the liver. One week after the treatment of mice with AdsFas or AdLacZ, liver tissue was harvested. The sFas expressed by AdsFas, which carries a Fas-Fc construct, was detected in frozen sections by immunoperoxidase (brown) staining using an anti-human IgG antibody. Representative sections are from mice treated with 109 pfu AdsFas (a), 107 pfu AdsFas (b) and 109 pfu AdLacZ (c) are shown. Magnification=100×
Treatment with sTNFRI in combination with AdsFas protects the mice from the lethal effects of Jo2
To determine if pathological processes other than Fas-mediated apoptosis contribute to the liver damage and lethality associated with administration of Jo2, we assessed the levels of TNF-α in the sera. One potential contributory mechanism is liver injury associated with the adenovirus transduction with the major cause of liver injury subsequent to adenovirus transduction being apoptosis mediated by the TNF-α/TNF receptors.31,32 As described above, only minimal evidence of damage was observed using equivalent pfu of control AdLacZ. A slight elevation in the levels of TNF-α in the sera was observed in mice pre-treated with 109 pfu/mouse of AdsFas and this elevation was slightly greater than that in those mice treated with 107 pfu/mouse of AdsFas or those that were not administered the adenoviral vector (Figure 6b, open bars). Notably, a further increase of TNF-α in the sera was observed in mice after Jo2 injection, and this occurred regardless of whether or not the mice had been pretreated with AdsFas (Figure 6b, hatched bars and open bars).
Effect of combined treatment with AdsFas and sTNFRI. (a) The time course of the experiment. Groups of mice (n=5) were pre-treated with AdsFas (109, 107 or 0 pfu/mouse) 1 week before administration of anti-Fas (Jo2) with soluble TNFRI being injected (200 μg) i.p. simultaneously with Jo2. (a) Survival was determined 24 h after Jo2 challenge. (b) Serum TNF-α levels. Serum samples were obtained by eye bleeding at 24 h before, and 3 h after, Jo2 injection. The results represent the mean±S.E.M. of five mice per group. (c) Improved survival of mice pretreated with AdsFas on administration of sTNFRI. The survival of mice administered sTNFRI (n=5) was compared with the survival of mice that did not receive sTNFRI (n=13, 15 and 5 in AdsFas 109 pfu/mouse, 107 pfu/mouse and control group, respectively as in Figure 1b). (d,e) Serum AST (d) and ALT (e) levels at 3 h after anti-Fas injection. The results are presented as the mean±S.E.M. from five different mice in each group with sTNFRI treatment. The levels of AST and ALT in the sera of mice that received sTNFRI (n=5) were compared with the levels of AST and ALT in the sera of mice that did not receive sTNFRI (n=13, 15 and 5 in AdsFas 109 pfu/mouse, 107 pfu/mouse and control group, respectively, as in Figure 3a,b)
These results suggested that Jo2-induced TNF-α may contribute to the liver cell damage and lethality associated with administration of Jo2. Therefore, we administered sTNFRI (200 μg/mouse) i.p. at the same time as the Jo2 was injected (Figure 6a). A statistically significant reduction in the levels of TNF-α in the sera was observed 3 h after Jo2 injection in the mice treated with sTNFRI compared to those without sTNFRI treatment in each group of AdsFas pre-treated mice (Figure 6b, closed bars and hatched bars). After Jo2 and sTNFRI injection, the levels of TNF-α were lowest in those mice that had been pre-treated with 109 pfu/mouse of AdsFas. Furthermore, the survival rate after Jo2 challenge was increased in the mice that had been pre-treated with 109 pfu/mouse of AdsFas, but not in mice pre-treated with 107 pfu/mouse of AdsFas (Figure 6c) with all of the mice pre-treated with 109 pfu/mouse of AdsFas and sTNFRI surviving (Figure 6c). The serum levels of AST and ALT at 3 h after Jo2 injection were lower in those mice treated with sTNFRI compared to mice treated without sTNFRI (Figure 6d,e). Although the survival at 24 hours after Jo2 and sTNFRI injection were different among three groups (Figure 6c), there was no difference in the AST and ALT levels between the three groups at 3 h after Jo2 and sTNFRI injection (Figure 6d,e, closed bars). Thus, inhibition of both the TNF-α/TNFRI and Fas/FasL-mediated apoptotic pathways is necessary for optimal protection against Jo2-induced liver injury in vivo.
GdCl3 protected mice from Jo2-induced TNF-α production and early death
To directly determine if Jo2 can signal TNF-α production by Kupffer cells in the liver and induce mortality, mice were treated with gadolinium chloride (GdCl3) to ablate Kupffer cells, and then treated with Jo2 (10 μg/mouse) 30 h later. In the absence of pre-treatment with GdCl3, the mice exhibited 90% mortality within 4–6 h (Figure 7a), whereas pretreatment with GdCl3 resulted in delayed death with the mortality being 40% at 4–6 h and 50% at 10–24 h, reaching 90% at 24 h after anti-Fas antibody injection. Thus, pretreatment with GdCl3 protected the mice from the early lethal effects of Jo2. Treatment of GdCl3 alone did not cause lethal effects to mice (data not shown).
Decreased early mortality and reduced production of TNF-α after administration of Jo2 in GdCl3-treated mice. (a) Decreased early mortality after treatment with GdCl3. Mice were administered with Jo-2 after pre-treatment with vehicle or GdCl3. Mortality was assessed at different time points after administration of Jo-2 (n=10 for each group). (b) TNF-α production by Kupffer cells in vivo. Mice were treated with Jo2 or GdCl3 plus Jo2 (n=10 for each group). Sera were collected 3 h and 6 h after Jo2 injection. Asterisks indicate that sera levels of TNF-α were below the detectable range. (c) Hepatocellular damage in the mice was evaluated by H&E staining. Representative sections from control mice that received vehicle only (upper left), received GdCl3 but not Jo2 (lower left), received Jo2 but not GdCl3 (upper right), and experimental mice that received GdCl3 treatment followed by Jo2 challenge (lower right) are presented. Magnification=80×
To determine whether the increased early survival of GdCl3-pretreated mice is associated with a reduction of TNF-α, the level of TNF-α produced by Jo2 stimulation of Kupffer cells in the liver was determined in vivo. There was high induction of serum TNF-α levels after treatment with Jo2 in control treated mice. Pre-treatment of mice with GdCl3, which ablates Kupffer cells in the liver, greatly reduced Jo2-induced serum levels of TNF-α (Figure 7b). These results indicate that Jo2 can stimulate TNF-α production by Kupffer cells in vivo. This correlates with a greatly diminished hepatocellular damage and intra-hepatic hemorrhage in GdCl3 pre-treated mice 6 h after Jo2 injection, compared to mice-treated with Jo2 alone (Figure 7c). There were no detectable levels of TNF-α in sera of control-treated or GdCl3 alone-treated mice (data not shown). There was also no evidence of hepatocellular damage in control-treated mice, or in mice treated with GdCl3 alone (Figure 7c).
Discussion
The results of the present study indicate that sFas is capable of inhibiting Fas-mediated apoptosis of liver cells in vivo. This inhibitory effect ameliorates the liver enzyme elevation, the tissue damage as evaluated by histologic analysis, and the liver failure leading to death that is associated with administration of anti-Fas antibody. In mice receiving 107 pfu of AdsFas i.v., less than 0.05% of liver cells produced sFas, as revealed by histologic analysis after staining with labeled anti-human IgG1 that specifically recognizes the sFas produced by the AdsFas. These cells were located randomly in the liver and the distribution did not appear to conform to any known pattern, such as a periarteriolar pattern. The expression of sFas was confirmed by immunohistochemical analysis in liver (Figure 5) and the secretion of sFas by the liver cells that produced sFas was further indicated by the location of sFas binding beyond the borders of these cells. The targeting of AdsFas was highly specific for the liver since sFas binding was detectable in the liver, but not in the lung (Figure 5 and data not shown). The sFas was detectable by ELISA assay in the sera and lysates of the liver of mice that received 109 or 1010 of AdsFas. However, sFas was not detectable by ELISA in the sera or liver lysates of mice receiving 107 pfu of AdsFas (Figure 4). The higher levels of sFas in the liver tissue compared to the sera may indicate that sFas accumulates intracellularly, or that sFas is secreted by the liver cells but sequestered by the liver stroma. Together, these results indicate that very low levels of sFas produced by a very small percentage of liver cells can provide significant protection of mice from the liver damage associated with administration of the anti-Fas antibody, Jo2.
Our results demonstrate that serum TNF-α is elevated after Jo2 challenge and this induction of TNF-α may well contribute to the Jo2-induced liver damage as TNF receptors are expressed on hepatocytes. It is well established that TNF-α interacts with TNFRI and mediates an apoptotic signal via the TNFRI-associated death domain (TRADD), which triggers the same down-stream signals as Fas/FasL pathway, including FADD and caspase 8. Elevation of serum TNF-α is seen as host response during conditions such as fulminant hepatic failure as well as endotoxin-induced shock.33 Our study supports the concept that TNF-α plays a significant role in the fatal response to Jo2 as treatment with sTNFRI together with AdsFas protected the mice completely from Jo2-mediated liver damage. Moreover, ablation of the Kupffer cells had a similar effect, indicating that the Kupffer cells, rather than a response to the adenovirus transduction, are the main source the TNF-α.
Our results therefore suggest (Figure 8) that AdsFas can protect hepatocytes partially from Jo2-mediated Fas apoptosis signaling, but Jo2 can still bind to the cell of the liver and, importantly, induces TNF-α production by the Kupffer cells. The TNF-α subsequently exacerbates the hepatocellular damage and, most probably triggers circulatory shock, leading to the death of the mice. Thus, this study suggests a model in which Jo2-mediated hepatocellular damage and its associated lethality reflect a complex two-step process involving Fas signaling to both hepatocytes and Kupffer cells, with the subsequent production of TNF-α playing a key role in the hepatocellular damage as well as the shock response, which is the primary cause of death in Jo2-treated mice. In the absence of the TNF-α effect (due to treatment with sTNFRI or ablation of Kupffer cells), Jo2 is capable of inducing Fas-mediated apoptosis of the liver with the associated damage being sufficient to cause death.
A model of Jo2-induced lethality in mice. We propose that Jo2-mediated hepatocellular damage and lethality reflects a complex two-step process involving Fas signaling in both hepatocytes and Kupffer cells in the liver. The subsequent production of TNF-α plays a key role in both hepatocellular damage and a shock response that serves as the primary cause of mortality associated with administration of Jo2. This model is supported by our present findings that AdsFas can partially protect hepatocytes from Jo2-mediated Fas apoptosis signaling and that AdsFas plus sTNFRI treatment rescues mice from Jo2-induced lethality. Elimination of TNF-α produced by Kupffer cells delayed Jo2-induced mortality
Materials and Methods
Mice
C57BL/6J +/+ female mice were purchased from The Jackson Laboratory (Bar Harbor, ME, USA). All mice were housed in a room equipped with an air filtering system. The cages, bedding, water, and food were sterilized, and the mice were handled with sterile gloves. Experiments were carried out using 6-week-old mice. All animal experiments were performed in accordance with the guidelines set forth by the NIH and the studies were approved by the Institution of Animal Care and Use Committee of the University of Alabama at Birmingham.
Construction and administration of AdsFas and AdLacZ
A recombinant replicative-defective adenovirus capable of producing soluble Fas (AdsFas) was produced by cloning a murine Fas containing the extracellular domain of Fas linked to the Fc and hinge portion of a human IgG1 (Fas-Fc) into the E1A site of adenovirus.34 Briefly The Fas-Fc was cloned into the E1A deletion site of adenovirus of pAdTRACKCMV in which Fas-Fc expression is driven by the CMV promoter. A recombinant adenovirus was produced by co-transfection of pAdTRACKCMVAkt-DN with pAdEasy-1 in BJ5183.
A recombinant adenovirus was produced by co-infection of sFas vector with pJM17 in the 293 cell line. The recombinant adenovirus expressing sFas was selected and purified using standard procedures.30 The correct orientation and cloning of the sFas in recombinant AdsFas was confirmed by PCR sequence analysis. To obtain a large quantity of recombinant AdsFas, 293 cells were infected and grown for 48 h at 37°C prior to harvest and centrifugation using a table-top centrifuge at 4000 r.p.m. for 20 min. The infected cells were resuspended in PBS buffer, then lysed using three freeze-thaw cycles. The released virus was purified through two CsCI gradients and the purified recombinant AdsFas was titrated by plaque assay,35 aliquoted, and stored at −80°C until use. Mice were injected intravenously with 109, 107 or 103 pfu/mouse of AdsFas in PBS. Control mice were injected with 109 pfu/mouse of AdLacZ in PBS or PBS alone.
Administration of anti-Fas antibody, Jo2
One week after AdsFas administration, mice were injected i.p. with 10 μg/mouse of anti-mouse Fas antibody from clone Jo2 (Pharmingen, San Diego, CA, USA). Control mice were treated with an equivalent volume of normal saline, i.p. Mice were observed closely for signs of clinical compromise, including decreased mobility and tachypnea for 24 h after administration of the Jo2 antibody.
Treatment with sTNFRI
One week after AdsFas pre-treatment, 200 μg/mouse of sTNFRI (Amgen, Thousand Oaks, CA, USA),36 dissolved in 500 μl of PBS, was injected i.p. at the same time as administration of Jo2 (Figure 6a).
Sera collection and analysis
Blood samples were collected by retro-orbital sinus puncture at 24 hours before and 3 hours after injection of anti-Fas antibody. Sera and plasma samples were stored at −20°C until use for measurement of sFas levels, and the plasma levels of the liver enzymes AST, ALT, and TNF-α as described below.
Survival analysis
Immediately after the mice appeared moribund, they were killed by cervical dislocation. Survival of mice was evaluated at 24 h after administration of Jo2. Statistical analysis of survival between the group treated with AdLacZ plus Jo2 and each group was determined by Fisher's exact test.
Preparation of liver lysates
The livers were obtained from the sacrificed mice, 1 week after pretreatment with the adenovirus constructs and a lysate prepared using 0.5 g of the tissue that was homogenized in 1.5 ml of lysis buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1% Triton X-100, 0.5% sodium deoxycholate, 0.1% SDS, and protease inhibitor (aprotinin 1 ng/ml, leupeptin 10 ng/ml, pepstatin A 1 ng/ml, and 1 μM sodium orthovanadate) on ice, then 150 μg of phenylmethylsulfonyl fluoride was added and the lysate incubated on ice for 10 min. To remove the nuclear fraction, the lysate was centrifuged at 2000×g for 5 min at 4°C. The samples were stored at −20°C until use in measurement of soluble Fas levels.
Preparation of sFas
Fas-Fc (sFas) was purified from a serum-free culture supernatant of AdsFas transfected cells. The supernatant was applied to the column of protein G-agarose (Sigma). Soluble Fas was eluted from column with acidic elution buffer (100 mM glycine-HCl, pH 3.0) and neutralized using 1 M Tris-HCl, pH 9.0. The concentration of the purified sFas was determined by measurement of the absorbance at 280 nm using a spectrophotometer (Smart SpecTM 3000, Bio-Rad Laboratories, Hercules, CA, USA) and the binding activity of the purified sFas to anti-Fas antibody was determined by ELISA assay as described previously.14
ELISA for soluble Fas and TNF-α
For measurement of sFas, 96-well ELISA plates were pretreated with 40 μg/ml of poly-L-lysine and coated at 4°C overnight with 4μg/ml of Jo2. The plates were washed and then blocked with 0.25% BSA, 0.05% Tween 20 borate-buffered saline. Standard Fas-Fc, and diluted serum or liver lysate were added to duplicate wells and incubated for 2 h at 37°C. After washing, the secondary antibody, horseradish peroxidase conjugated anti-human IgG (Southern Biotechnology Associates, Inc., Birmingham, AL, USA), was added and the plates incubated for 1 h at 37°C. 3,3′,5,5′-tetramethylbenzidine (Sigma, St. Louis, MO, USA) was added and incubated for 30 min at room temperature. The reaction was stopped by addition of H2SO4, 0.2 N and the absorbance was measured at 450 and 650 nm. A standard curve was derived for detection of sFas and revealed the lower limit for the detection of mouse Fas-Fc as 1.0 ng/ml. The serum levels of TNF-α were measured using the mouse ELISA kit for TNF-α (BioSource International, Inc., Camarillo, CA, USA) according to the instructions provided by the manufacturer.
Histologic analysis
A portion of the excised liver was fixed with 10% buffered-formalin and embedded in paraffin. Sections (4 micron) were obtained from the paraffin-embedded tissue samples and stained with hematoxylin and eosin, and with Hoechst dye 33342 (Molecular Probes, Inc. Eugene, OR, USA). Hoechst staining was performed as follows; after fixation, the sections were incubated with blocking buffer (5% FCS, 0.1% NaN3 in PBS) for 20 min followed by incubation with 20 μg/ml of Hoechst 33342 in blocking buffer for 7 min, and then washed with PBS. Fluorescence was visualized using a standard fluorescence microscope.
Immunohistochemical analysis
A portion of the excised liver was embedded in OCT medium and then snap frozen. After sectioning, the prepared slides were incubated with 3% hydrogen peroxide in distilled water for 5 min. The slides were then rinsed with distilled water prior to treatment with pepsin (4 μg/μl) at room temperature for 30 min. After washing with PBS, the slides were incubated with horseradish peroxidase-conjugated anti-human IgG (Southern Biotechnology Associates, Inc.) at room temperature for 1 h, followed by incubation with 3,3′-diaminobenzidine (Sigma) for 15 min. Finally, the slides were rinsed with distilled water and counter-stained with 0.5% methyl green.
GdCl3 treatment of mice
For transient ablation of Kupffer cells, a protocol described previously37,38 was adapted. GdCl3 was dissolved in H2O, and 10 mg/kg of body weight in a total volume of 400 μl was injected i.p. at 30 and 6 h prior to Jo2. Control animals were injected with 400 μl of saline. To test the phagocytic capacity of the Kupffer cells, colloidal carbon (0.8 ml/kg of body weight; Sigma, St. Louis MO, USA) was injected 30 minutes before sacrifice into untreated mice or mice treated with GdCl3.37 The carbon uptake by liver macrophages, scored by light microscopy of liver sections was reduced by approximately 80% in mice that received the double GdCl3 injection compared to untreated animals. This is consistent with results obtained in previous studies.38
Abbreviations
- sFas:
-
soluble Fas
- pfu:
-
plaque forming unit
- AdsFas:
-
adenovirus capable of producing soluble Fas
- LacZ:
-
gene coded for β-galactosidase
- AdLacZ:
-
adenovirus capable of producing LacZ
- CMV:
-
cytomegalovirus
- TNF-α:
-
tumor necrosis factor-α
- sTNFRI:
-
soluble TNF receptor I
- B6:
-
C57BL/6
- Jo2:
-
anti-mouse Fas antibody
- GdCl3:
-
gadolinium chloride
- Fc:
-
fragment crystallizable region of an immunoglobulin G molecule
- Fas-Fc:
-
The extracellular domain of murine Fas linked to the Fc and hinge portion of a human IgG1 that produces a murine soluble Fas
References
Muschen M, Warskulat U, Douillard P, Gilbert E, Haussinger D . 1998 Regulation of CD95 (APO-1/Fas) receptor and ligand expression by lipopolysaccharide and dexamethasone in parenchymal and nonparenchymal rat liver cells Hepatology 27: 200–208
Rafi AQ, Zeytun A, Bradley MJ, Sponenberg DP, Grayson RL, Nagarkatti M, Nagarkatti PS . 1998 Evidence for the involvement of Fas ligand and perforin in the induction of vascular leak syndrome J. Immunol. 161: 3077–3086
Sata M, Walsh K . 1998 Oxidized LDL activates fas-mediated endothelial cell apoptosis J. Clin. Invest. 102: 1682–1689
Shi J, Gilbert GE, Kokubo Y, Ohashi T . 2001 Role of the liver in regulating numbers of circulating neutrophils Blood 98: 1226–1230
Muschen M, Warskulat U, Peters-Regehr T, Bode JG, Kubitz R, Haussinger D . 1999 Involvement of CD95 (Apo-1/Fas) ligand expressed by rat Kupffer cells in hepatic immunoregulation Gastroenterology 116: 666–677
Itoh N, Nagata S . 1993 A novel protein domain required for apoptosis. Mutational analysis of human Fas antigen J. Biol. Chem. 268: 10932–10937
Tartaglia LA, Ayres TM, Wong GH, Goeddel DV . 1993 A novel domain within the 55 kd TNF receptor signals cell death Cell 74: 845–853
Chinnaiyan AM, Tepper CG, Seldin MF, O'Rourke K, Kischkel FC, Hellbardt S, Krammer PH, Peter ME, Dixit VM . 1996 FADD/MORT1 is a common mediator of CD95 (Fas/APO-1) and tumor necrosis factor receptor-induced apoptosis J. Biol. Chem. 271: 4961–4965
Chinnaiyan AM, O'Rourke K, Tewari M, Dixit VM . 1995 FADD, a novel death domain-containing protein, interacts with the death domain of Fas and initiates apoptosis Cell 81: 505–512
Boldin MP, Goncharov TM, Goltsev YV, Wallach D . 1996 Involvement of MACH, a novel MORT1/FADD-interacting protease, in Fas/APO-1- and TNF receptor-induced cell death Cell 85: 803–815
Medema JP, Scaffidi C, Kischkel FC, Shevchenko A, Mann M, Krammer PH, Peter ME . 1997 FLICE is activated by association with the CD95 death-inducing signaling complex (DISC) EMBO J. 16: 2794–2804
Peter ME, Kischkel FC, Scheuerpflug CG, Medema JP, Debatin KM, Krammer PH . 1997 Resistance of cultured peripheral T cells towards activation-induced cell death involves a lack of recruitment of FLICE (MACH/caspase 8) to the CD95 death-inducing signaling complex Eur. J. Immunol. 27: 1207–1212
Muzio M, Chinnaiyan AM, Kischkel FC, O'Rourke K, Shevchenko A, Ni J, Scaffidi C, Bretz JD, Zhang M, Gentz R, Mann M, Krammer PH, Peter ME, Dixit VM . 1996 FLICE, a novel FADD-homologous ICE/CED-3-like protease, is recruited to the CD95 (Fas/APO-1) death-inducing signaling complex Cell 85: 817–827
Cheng J, Zhou T, Liu C, Shapiro JP, Brauer MJ, Kiefer MC, Barr PJ, Mountz JD . 1994 Protection from Fas-mediated apoptosis by a soluble form of the Fas molecule Science 263: 1759–1762
Al-Maini MH, Mountz JD, Al-Mohri HA, El-Ageb EM, Al-Riyami BM, Svenson KL, Zhou T, Richens ER . 2000 Serum levels of soluble Fas correlate with indices of organ damage in systemic lupus erythematosus Lupus 9: 132–139
Cheng J, Liu C, Koopman WJ, Mountz JD . 1995 Characterization of human Fas gene. Exon/intron organization and promoter region J. Immunol. 154: 1239–1245
Liu C, Cheng J, Mountz JD . 1995 Differential expression of human Fas mRNA species upon peripheral blood mononuclear cell activation Biochem. J. 310: 957–963
Ogasawara J, Watanabe-Fukunaga R, Adachi M, Matsuzawa A, Kasugai T, Kitamura Y et al. 1993 Lethal effect of the anti-Fas antibody in mice Nature 364: 806–809
Ni R, Tomita Y, Matsuda K, Ichihara A, Ishimura K, Ogasawara J, Nagata S . 1994 Fas-mediated apoptosis in primary cultured mouse hepatocytes Exp. Cell. Res. 215: 332–337
Kondo T, Suda T, Fukuyama H, Adachi M, Nagata S . 1997 Essential roles of the Fas ligand in the development of hepatitis Nat. Med. 3: 409–413
Pensati L, Costanzo A, Ianni A, Accapezzato D, Iorio R, Natoli G et al. 1997 Fas/Apo1 mutations and autoimmune lymphoproliferative syndrome in a patient with type 2 autoimmune hepatitis Gastroenterology 113: 1384–1389
Galle PR, Hofmann WJ, Walczak H, Schaller H, Otto G, Stremmel W, Krammer PH, Runkel L . 1995 Involvement of the CD95 (APO-1/Fas) receptor and ligand in liver damage J. Exp. Med. 182: 1223–1230
Ksontini R, Colagiovanni DB, Josephs MD, Edwards 3rd CK, Tannahill CL, Solorzano CC, Norman J, Denham W, Clare-Salzler M, MacKay SL, Moldawer LL . 1998 Disparate roles for TNF-alpha and Fas ligand in concanavalin A-induced hepatitis J. Immunol. 160: 4082–4089
Krams SM, Martinez OM . 1998 Apoptosis as a mechanism of tissue injury in liver allograft rejection Semin. Liver Dis. 18: 153–167
Seishima M, Takemura M, Saito K, Ando K, Noma A . 1997 Increased serum soluble Fas (sFas) concentrations in HCV-positive patients with liver cirrhosis J. Hepatol. 27: 424–425
Iio S, Hayashi N, Mita E, Ueda K, Mochizuki K, Hiramatsu N et al. 1998 Serum levels of soluble Fas antigen in chronic hepatitis C patients J. Hepatol. 29: 517–523
Gladman DD, Urowitz MB, Goldsmith CH, Fortin P, Ginzler E, Gordon C et al. 1997 The reliability of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index in patients with systemic lupus erythematosus Arthritis Rheum. 40: 809–813
Mosher B, Dean R, Harkema J, Remick D, Palma J, Crockett E . 2001 Inhibition of Kupffer cells reduced CXC chemokine production and liver injury J. Surg. Res. 99: 201–210
Vollmar B, Ruttinger D, Wanner GA, Leiderer R, Menger MD . 1996 Modulation of kupffer cell activity by gadolinium chloride in endotoxemic rats Shock 6: 434–441
Zhang HG, Liu D, Heike Y, Yang P, Wang Z, Wang X et al. 1998 Induction of specific T-cell tolerance by adenovirus-transfected, Fas ligand-producing antigen presenting cells Nat. Biotechnol. 16: 1045–1049
Liu ZX, Govindarajan S, Okamoto S, Dennert G . 2000 Fas- and tumor necrosis factor receptor 1-dependent but not perforin- dependent pathways cause injury in livers infected with an adenovirus construct in mice Hepatology 31: 665–673
Zhang HG, Zhou T, Yang P, Edwards 3rd CK, Curiel DT, Mountz JD . 1998 Inhibition of tumor necrosis factor alpha decreases inflammation and prolongs adenovirus gene expression in lung and liver Hum. Gene Ther 1998 9: 1875–1884
Streetz K, Leifeld L, Grundmann D, Ramakers J, Eckert K, Spengler U et al. 2000 Tumor necrosis factor alpha in the pathogenesis of human and murine fulminant hepatic failure Gastroenterology 119: 446–460
He TC, Zhou S, da Costa LT, Yu J, Kinzler KW, Vogelstein B . 1998 A simplified system for generating recombinant adenoviruses Proc Natl Acad Sci USA 95: 2509–2514
Zhang HG, Huang N, Liu D, Bilbao L, Zhang X, Yang P et al. 2000 Gene therapy that inhibits nuclear translocation of nuclear factor kappaB results in tumor necrosis factor alpha-induced apoptosis of human synovial fibroblasts Arthritis Rheum. 43: 1094–1105
Su X, Zhou T, Yang P, Edwards 3rd CK, Mountz JD . 1998 Reduction of arthritis and pneumonitis in motheaten mice by soluble tumor necrosis factor receptor Arthritis Rheum. 41: 139–149
Lieber A, He CY, Meuse L, Schowalter D, Kirillova I, Winther B et al. 1997 The role of Kupffer cell activation and viral gene expression in early liver toxicity after infusion of recombinant adenovirus vectors J. Virol. 71: 8798–8807
O'Neill PJ, Ayala A, Wang P, Ba ZF, Morrison MH, Schultze AE et al. 1994 Role of Kupffer cells in interleukin-6 release following trauma- hemorrhage and resuscitation Shock 1: 43–47
Acknowledgements
We thank Ms Linda Flurry for excellent secretarial work. This work was supported by NIH grants R01-AG-11653, RO1-AI-46990, RO1-AI-42900, N01 AR 6-2224, a Birmingham VAMC Merit Review Grant and a grant from Sankyo, Inc. Dr Huang-Ge Zhang is supported by a grant from the Arthritis Foundation. Dr Hui-Chen Hsu is supported by a grant from the Center for Aging at the University of Alabama at Birmingham.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by G Nunez
Rights and permissions
About this article
Cite this article
Matsuki, Y., Li, L., Hsu, HC. et al. Soluble Fas gene therapy protects against Fas-mediated apoptosis of hepatocytes but not the lethal effects of Fas-induced TNF-α production by Kupffer cells. Cell Death Differ 9, 626–635 (2002). https://doi.org/10.1038/sj.cdd.4401016
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401016
Keywords
This article is cited by
-
TNFα sensitizes hepatocytes to FasL-induced apoptosis by NFκB-mediated Fas upregulation
Cell Death & Disease (2018)
-
The microbiota regulates susceptibility to Fas-mediated acute hepatic injury
Laboratory Investigation (2014)
-
Protective effects of HFE7A, mouse anti-human/mouse Fas monoclonal antibody against acute and lethal hepatic injury induced by Jo2
Cytotechnology (2010)
-
Primary adenovirus-specific cytotoxic T lymphocyte response occurs after viral clearance and liver enzyme elevation
Gene Therapy (2005)
-
Identification of multiple genetic loci that regulate adenovirus gene therapy
Gene Therapy (2004)