Abstract
We have previously shown that the protein kinase C (PKC) signal transduction pathway regulates cell death by the DNA damaging agent cis-diamminedichloroplatinum(II) (cDDP). In the present study we have investigated how PKC influences the sequence of events that are triggered by cDDP-induced DNA damage. cDDP caused activation of caspases-8, -9, -3, -7 and cleavage of PKCδ. Rottlerin, a selective inhibitor of novel PKCδ, blocked activation of caspases, proteolytic activation of PKCδ and cell death induced by cDDP. In contrast, Gö 6976, an inhibitor of conventional PKCα and βI, did not prevent cDDP-induced caspase activation and cDDP cytotoxicity. In HeLa cells, PKCδ was distributed both in the cytosol and heavy membrane (HM) fraction containing mitochondria. While caspase-8 was primarily cytosolic, a small amount of caspases-9, -7 and -3 could be detected in the HM fraction. cDDP caused a time-dependent increase in Cytochrome c release from the mitochondria and processing of both cytosolic and membrane-associated caspases, as well as proteolytic cleavage of PKCδ. Rottlerin attenuated late but not early release of Cytochrome c by cDDP. It, however, inhibited activation of caspases and proteolytic cleavage of PKCδ in both cytosolic and HM fractions. The antiapoptotic effect of rottlerin was evident when it was added together with or following cDDP addition but not when added after cDDP was removed from the medium. Thus, the PKCδ inhibitor acts at an early stage of the cDDP-induced cell death pathway that precedes caspase activation. Cell Death and Differentiation (2001) 8, 899–908
Similar content being viewed by others
Introduction
Caspases are essential for the execution of cell death by apoptotic stimuli.1,2,3,4 The pathway of cell death varies depending on the cell type as well as the apoptotic stimuli. It is generally believed that binding of Fas ligand or tumor necrosis factor-α (TNF) to their receptors causes activation of the initiator caspase-8 followed by the activation of a caspase cascade to execute cell death.2,5 In contrast, DNA damaging agents are known to induce release of mitochondrial Cytochrome c, which facilitates the interaction of apoptotic protease activating factor (Apaf-1) with procaspase-9 to initiate the activation of downstream effector caspases, such as caspases-3 or -7 to cause cell death.3 Both receptor-mediated and anticancer drug-induced apoptosis may, however, involve more than one pathway and there may be cross-talk between these two pathways.6,7,8
cis-Diamminedichloroplatinum(II) (cDDP or cisplatin) is one of the most important anticancer agents used for the treatment of solid tumors.9 Although the antitumor activity of cDDP is believed to be due to its interaction with chromosomal DNA, only a small fraction of cDDP actually interacts with DNA and inhibition of DNA replication cannot solely account for its biological activity.10 The efficacy of chemotherapeutic drugs not only depends on their ability to induce DNA damage but also on the cell's ability to detect and respond to DNA damage.11 cDDP, like other chemotherapeutic drugs, causes activation of caspases although the sequence of events that follow cDDP-induced DNA damage and lead to apoptosis remains to be unraveled.
We and others have shown that the PKC signal transduction pathway regulates cell death by cDDP.12,13,14,15,16,17 PKC is a family of 11 isozymes that are classified as the conventional PKCs (α, βI, βII and γ), novel PKCs (δ, ε, η, and θ), atypical PKCs (ζ and λ/ι) and novel/atypical PKCμ.18 PKCδ is a substrate for caspase-3 and the catalytic fragment of PKCδ has been directly associated with apoptotic cell death.19,20 We have, however, demonstrated that downregulation of PKC that decreased the abundance of PKCδ catalytic fragment was associated with increased cellular sensitivity to cDDP.17 These results raise the possibility that PKC acts upstream of caspases to regulate cell death by cDDP. It is not known which PKC isozyme regulates activation of caspases and which step(s) of the cisplatin-induced cell death pathway is regulated by PKC.
Mitochondria play a pivotal role in the decision making process of a cell's life and death.21 It is believed that once Cytochrome c is released from mitochondria, cells are committed to die.22 An inability to induce release of Cytochrome c from mitochondria has been associated with cellular resistance to anticancer agents, including cDDP.23 In the present study, we have investigated how PKC regulates release of Cytochrome c and activation of caspases that emanate from mitochondria. Our results show that in HeLa cells, PKCδ was localized not only in the cytosol but also in the mitochondrial fraction and cDDP induced processing of both cytosolic and membrane-associated PKCδ. Rottlerin, a specific inhibitor of PKCδ, blocked cDDP-induced activation of caspases and proteolytic cleavage of PKCδ in both cytosolic and HM fractions but inhibited only late but not early release of Cytochrome c. Furthermore, inhibition of nPKCδ, but not of cPKCs, protected cells against cDDP-induced cell death. Taken together, these results demonstrate that PKCδ influences cDDP-induced cell death by acting at an early step of the mitochondrial cell death pathway that precedes activation of caspases.
Results
Effects of PKC inhibitors on cDDP-induced cell death
We have previously shown that the PKC signal transduction pathway regulates cell death by cDDP.14,15,16 To examine the involvement of a specific PKC isozyme in cDDP-induced cell death, we compared the effects of several PKC inhibitors that exhibit distinct specificities towards PKC isozymes on the cytotoxic effect of cDDP. Bisindolylmaleimide (BIM) inhibits all PKC isozymes with a rank order of potency of α>βI>ε>δ>ζ.24 As shown in Figure 1, 1 μM BIM did not influence cDDP sensitivity whereas 10 μM BIM increased the IC50 of cDDP by twofold. In contrast, Gö 6976, an inhibitor of cPKCs,24 increased cDDP sensitivity by twofold, however it decreased HeLa cell proliferation by almost 50%. In addition, the effect of Gö 6976 on cDDP sensitivity was similar at both 1 and 10 μM concentrations. Rottlerin, a specific inhibitor of nPKCδ,25 decreased cellular sensitivity to cDDP in a concentration-dependent manner; the IC50 of cDDP was increased from 10.3 to 28.5 μM by 10 μM rottlerin and to greater than 40 μM when cells were pretreated with 20 μM rottlerin.
Effects of PKC inhibitors on cell death by cDDP. HeLa cells were pretreated without or with BIM, Gö 6976 or rottlerin for 1 h and then treated with different concentrations of cDDP for 2 h. The cell survival was determined after 24 h by an MTT assay as described in Materials and Methods. Qualitatively similar results were obtained when cells were treated continuously with cDDP. The results are representative of at least three experiments performed in quadruplicate. ○, control; Δ, 1 μM BIM; ▴, 10 μM BIM; ▿, 1 μM Gö 6976; ▾, 10 μM Gö 6976; □, 10 μM rottlerin; ▪, 20 μM rottlerin
To examine if rottlerin specifically inhibits PKCδ activity in HeLa cells, we immunoprecipitated PKCδ from HeLa cells and determined its activity in vitro using myelin basic protein (MBP) as the substrate. Figure 2 shows that TPA caused significant phosphorylation of MBP and rottlerin blocked MBP phosphorylation by TPA, suggesting that rottlerin inhibits PKCδ activity. To check for the specificity of rottlerin, we examined the effect of rottlerin on cPKCα activity. As shown in Figure 2, 10 μM rottlerin had only a slight effect on Ca2+-, PS/TPA-dependent phosphorylation of MBP by cPKCα although Gö 6976 completely inhibited cPKCα activity. Gö 6976 also appears to decrease MBP phosphorylation by PKCδ. The amount of PKCδ was, however, less in the reaction mixture as evident by the PKCδ immunoblot.
Effect of rottlerin and Gö 6976 on PKC activity. PKCα or -δ was immunoprecipitated from HeLa cells using an antibody to PKCα or δ. Cells were treated with or without 10 μM rottlerin or 5 μM Gö 6976 and/or 0.2 mg/ml phosphatidylserine and 100 nM TPA. 0.5 mM CaCl2 was also added with PKC activators in PKCα immunokinase assay. PKC activity was determined using MBP as the substrate and SDS–PAGE was performed as described under Materials and Methods. Autoradiography was performed with the dried gel and Western blot analyses were performed with PKCα and -δ antibodies following transfer of proteins to PVDF membrane. Results are representative of 2–4 individual experiments
cDDP, like most chemotherapeutic drugs, is known to induce cell death by apoptosis.10 Figure 3 shows that when cells were treated with 10 μM cDDP, cells rounded up and detached from the tissue culture dish; the number of floating cells increased further by 20 μM cDDP. Rottlerin by itself had no effect on cellular morphology but it reversed the effect of cDDP. In contrast, Gö 6976 was unable to block the effect of cDDP. These results suggest that inhibition of nPKCδ rather than cPKCs was responsible for the attenuation of cDDP-induced cell death.
Effects of PKC inhibitors on the proteolytic activation of PKCδ
Proteolytic cleavage of PKCδ by caspase-3 results in the generation of the catalytic fragment of PKCδ, thereby activating it.19 Figure 4 shows that cDDP caused cleavage of full-length PKCδ as evident by the decrease in 78-kDa full-length PKCδ with a concomitant increase in the 40-kDa catalytic fragment of PKCδ. Pretreatment of HeLa cells with 10 μM rottlerin decreased proteolytic cleavage of PKCδ, whereas the cPKC inhibitor Gö 6976 was unable to block cDDP-induced proteolytic activation of PKCδ, suggesting that cPKC inhibitor had no effect on the proteolytic activation of PKCδ in intact cells even at 10 μM concentrations.
Effects of PKC inhibitors on cDDP-induced caspase activation and proteolytic cleavage of PKDδ. HeLa cells were pretreated with or without 10 μM Gö 6976 or rottlerin for 30 min and then with 20 μM cDDP for 8 h. Western blot analysis was performed with antibody to caspases-8, -9, -3 and PKCδ. The arrows indicate the processed forms. Results are representative of 3–7 experiments
Since caspase-3 may be cleaved both by caspases-8 and -9, we examined the effect of rottlerin on cDDP-induced activation of caspases-8 and -9. As shown in Figure 4, an 8 h exposure of HeLa cells to cDDP had little effect on the activation of caspase-8 but did induce processing of caspases-9 and -3. Rottlerin but not Gö 6976 blocked cDDP-induced activation of these caspases. These results suggest that inhibition of caspase-9 by rottlerin blocks activation of caspase-3 and thus proteolytic cleavage of PKCδ.
Since cDDP caused proteolytic cleavage of PKCδ, we examined the effect of the PKCδ-specific inhibitor rottlerin on cDDP-induced activation of PKCδ. Figure 5 shows that a 12 h exposure to 20 μM cDDP caused almost twofold stimulation of MBP phosphorylation in the absence of any lipid cofactors, suggesting that the catalytic fragment generated by cDDP was constitutively active. Rottlerin completely blocked activation of PKC by cDDP. These results suggest that rottlerin inhibits cDDP-induced activation of PKCδ.
Effect of cDDP and rottlerin on the activation of PKC. Cells were pretreated with 10 μM rottlerin for 1 h and then treated with or without 20 μM cDDP for another 12 h. PKC activity was determined using MBP as the substrate as described under Materials and Methods. Results are representative of two experiments performed in duplicates
Effect of cDDP and rottlerin on the activation of cDDP-induced caspase cascade
It is generally believed that caspases-8 and -9 are the apical caspases for receptor- and drug-induced apoptosis, respectively.3,5 It has recently been shown that both receptor and chemical-induced apoptosis can involve more than one pathway. For example, the anticancer agent etoposide caused activation of caspases-8, -9, -3 and -7 simultaneously.6 Furthermore, although the formation of the apoptosome complex and activation of caspase-9 and its downstream caspases are known to take place in the cytoplasm,21 little is known about compartmentalized activation of caspases in response to apoptotic stimuli. Since mitochondria play an important role in drug-induced apoptosis, we compared the effect of cDDP on the activation of caspases in both cytosolic and mitochondrial compartments. Although caspases are primarily localized in the cytoplasm, a small amount of caspase-9 could be detected in the crude mitochondrial fractions (Figure 6). A 6 h treatment with cDDP caused proteolytic cleavage of the 48-kDa procaspase-9 to 37- and 35-kDa processed forms in the cytosolic fraction. When duration of exposure to cDDP was increased, processing of procaspase-9 was evident in both cytosolic and membrane fractions.
Effect of cDDP and rottlerin on the compartmentalized activation of caspases and PKCδ. HeLa cells were pretreated with or without 10 μM rottlerin and then treated with or without 20 μM cDDP for 6, 9 or 12 h. Cells were fractionated into cytosol and heavy membrane fraction containing mitochondria and immunoblot analyses were performed using indicated antibodies as described under Materials and Methods. The arrows indicate the processed forms. Results are representative of 3–6 experiments
Caspase-8 was primarily cytosolic and a 6 h exposure of HeLa cells to cDDP had no effect on the processing of procaspase-8. Processing of the 55-kDa procaspase-8 to 14- and 10-kDa fragments was apparent after 9 h but the active forms of caspase-8 were present exclusively in the cytosol of cDDP-treated cells. Since caspase-8 acts primarily through the receptor-mediated pathway and it has been reported that the membrane death receptor CD95 (Apo-1/Fas) is upregulated after cDDP exposure in HeLa cells,26 we also examined the effect of neutralizing anti-FasL antibody on cDDP-induced cell death. A 16 h exposure to 20 μM cDDP caused 70% cell death as determined by the appearance of a sub-G1 peak in FACS analysis. Preincubation with 5 μg/ml of FasL neutralizing antibody for 30 min prior to cDDP addition resulted in 76% cell death. In addition, the neutralizing anti-FasL antibody had no effect on caspase activation (data not shown).
In HeLa cells, caspase-3 was present primarily in the cytosol. A 6 h exposure to cisplatin had little effect on the processing of procaspase-3 although faint bands could be detected near the 20-kDa region. The distribution and processing of caspase-7 was essentially similar to caspase-3 and with increasing duration of exposure to cDDP, the presence of active fragments could be detected in the HM fractions. We also determined the effect of rottlerin on cDDP-induced activation of caspases by measuring the cleavage of the fluorometric substrate Ac-DEVD-AFC. As indicated in Figure 6, the majority of DEVDase activity was present in the cytosolic fraction although a small DEVDase activity could be detected in the HM fraction. cDDP caused a time-dependent increase in DEVDase activity both in the cytosol and HM fractions and rottlerin inhibited DEVDase activity in both fractions. Thus, the caspase activity assay corroborated our results with Western blot analyses.
Since rottlerin blocked activation of the apical caspase-9, which was present both in the cytosol and HM fraction, we determined the subcellular distribution of PKCδ following treatment with cDDP. As shown in Figure 6, PKCδ was distributed both in the cytosol and HM fractions. A 6 h exposure of HeLa cells to cDDP caused cleavage of PKCδ in the cytosolic fraction, and by 12 h both cytosolic and mitochondrial PKCδ were processed almost completely. Rottlerin by itself had no effect on the subcellular distribution of PKCδ but it inhibited proteolytic cleavage of PKCδ in both fractions. These results suggest that rottlerin blocked proteolytic activation of PKCδ by inhibiting activation of caspase-9 and its downstream caspases.
Effect of cDDP and rottlerin on Cytochrome c release
Since release of mitochondrial Cytochrome c is believed to be one of the early events following DNA damage, we examined whether rottlerin inhibits the egress of Cytochrome c from the mitochondria. As shown in Figure 7A,B, cDDP caused a time-dependent increase in Cytochrome c release. Pretreatment of HeLa cells with rottlerin decreased release of Cytochrome c following an exposure to cDDP for ⩾9 h but not when cells were treated with cDDP for less than 9 h. We consistently found that rottlerin by itself caused a small release of Cytochrome c. We probed the blot with anti-human Cytochrome oxidase subunit II (Cox-II) and Apaf-1 as markers for mitochondria and cytosol, respectively. The low abundance of Cox-II in the HM fractions following exposure to cDDP for 3 h could explain the decreased levels of Cytochrome c in those fractions. We also performed a parallel experiment to monitor cell death by FACS analysis. Without any cDDP treatment, 2–3% of cells appeared in the sub-G1 peak and treatment with cDDP for 3 and 6 h had little effect on cell death. The fraction of cells undergoing apoptosis increased to 10 and 26% following exposure to cDDP for 9 and 12 h, respectively, and rottlerin reduced the fraction of cells undergoing apoptosis to 4 and 6%, respectively. Since activation of caspase-9 appears to be important for cDDP induced cell death and Cytochrome c is believed to activate caspase-9, we also monitored processing of procaspase-9 following exposure to cDDP. cDDP induced a time-dependent activation of caspase-9 and rottlerin inhibited cDDP-induced activation of caspase-9 in both cytosolic and mitochondrial fractions even though it did not prevent Cytochrome c release completely. Thus, the effect of rottlerin on cDDP-induced cell death correlated with its effect on caspase activation rather than on Cytochrome c release.
Effect of cDDP and rottlerin on the release of Cytochrome c from mitochondria. Cells were pretreated with or without 10 μM rottlerin for 30 min and then treated with or without 20 μM cDDP. (A) At indicated time intervals, cells were processed and immunoblot analyses were performed with cytosolic and HM fractions using indicated antibodies. (B) Cytochrome c released in the cytosol was quantified by scanning immunoblots with a laser densitometer and the values are the mean±standard error of 3–5 individual experiments
Effect of rottlerin incubation time on cDDP-induced cell death
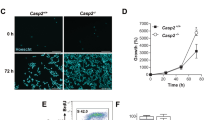
To examine if rottlerin acts at an early or late stage of the cDDP-induced cell death pathway, we added rottlerin either before, together with, or after cDDP addition. The apoptotic cells were monitored by their appearance in the subG0/G1 peak in a flow cytometer. When cells were treated with 15 μM cDDP for 16 h, 54% cells appeared in the subG0/G1 phase (Figure 8A). Pretreatment of cells with rottlerin for 1 h prior to cDDP addition decreased the number of apoptotic cells to 12%. The effect of rottlerin on cDDP-induced apoptosis was similar when rottlerin was added together with or 1 h following cDDP treatment. When rottlerin was added 2 or 4 h subsequent to cDDP treatment, the fraction of cells in the subG0/G1 peak increased to 23 and 45%, respectively. There was a good correlation between the ability of rottlerin to inhibit caspase activation and to block cDDP-induced cell death (data not shown). Furthermore, when rottlerin was added after cDDP treatment was initiated, its ability to prevent Cytochrome c release decreased (Figure 8B). These results suggest that rottlerin acts at an early stage of the cDDP-induced cell death pathway.
Effect of time of addition of rottlerin on cDDP induced cell death and Cytochrome c release. HeLa cells were treated with 15 μM cDDP for 16 h. The time of cDDP addition was considered 0 h. Rottlerin (10 μM) was added either 1 h prior to cDDP addition (−1 h), concomitantly with cDDP (0 h) or 1, 2 or 4 h after cDDP addition. (A) Cells were stained with propidium iodide and analyzed using a flow cytometer. The results are representative of 2–3 individual experiments. (B) Immunoblot analysis was performed with cytosolic extracts using antibody against Cytochrome c or actin as described under Materials and Methods
Discussion
Although it is well-established that the PKC signal transduction pathway regulates cell death mediated by a variety of apoptotic stimuli, including the DNA damaging agent cDDP, it is not clear how PKC influences cell death by these agents. While activation of caspases is necessary to execute cell death, it is also important to inactivate the regulatory proteins that otherwise block caspase activation. Several intracellular signaling molecules, including Akt/PKB and MEK kinase, have been shown to regulate activation of caspases.3 It is believed that PKC acts at a late stage of the cell death pathway since PKCδ and -θ are substrates for caspase-319,27 and the catalytic fragment of these PKCs may induce apoptotic morphology.19,20 We have provided evidence that the PKC signal transduction pathway in fact acts upstream of caspase-3.17 The results of the present study demonstrate that in HeLa cells PKCδ is constitutively associated with the HM fraction containing mitochondria and cisplatin induced proteolytic activation of PKCδ in both fractions. Furthermore, while inhibition of PKCδ only partially influences cDDP-induced Cytochrome c release, it inhibits cDDP-induced activation of caspases in both the cytosol and mitochondria. Thus, PKCδ acts at an early stage of the mitochondrial cell death pathway that precedes activation of caspase-9 to regulate cell death triggered by cDDP.
In the present study, we have used PKC inhibitors that exhibit distinct selectivity towards PKC isozymes to establish the involvement of a particular PKC isozyme in the regulation of cell death by cDDP. Bisindolylmaleimide inhibits all PKC isozymes, albeit with different potencies; cPKCs are the most sensitive and their IC50 values are in the nanomolar range in in vitro kinase assays, nPKCs can be inhibited in the submicromolar range whereas aPKCs are least sensitive to BIM.24 We have shown that 1 μM BIM that was sufficient to inhibit cPKCs in intact cells had no effect on cDDP-induced cell death whereas 10 μM BIM decreased cDDP cytotoxicity, suggesting that inhibition of nPKCs or aPKCs was responsible for protection against cDDP cytotoxicity by BIM. Rottlerin inhibits PKC isozymes with IC50 values for PKCδ, 3–6 μM, cPKCs, 30–40 μM and PKCε, -η and -ζ, 80–100 μM.25 We have shown that rottlerin at concentrations ⩽20 μM inhibited cDDP-induced cell death significantly, suggesting that inhibition of nPKCδ rather than inhibition of cPKCs, nPKCε or aPKCs was important for the decrease in cellular sensitivity to cDDP by rottlerin. This is further corroborated by the observation that Gö 6976, which inhibits cPKCα and βI at nanomolar concentrations but has little effect on nPKCs or aPKCs,24 failed to block cDDP-induced cell death even at 10 μM concentrations. In fact, it increased cDDP cytotoxicity by twofold. We have found that even 1 μM Gö 6976 by itself inhibited HeLa cell proliferation by almost 50%. Therefore, the increase in cellular sensitivity to cDDP by Gö 6976 could be secondary to its toxic side effect. In addition, rottlerin, but not Gö 6976, inhibited proteolytic cleavage of PKCδ by cDDP. These results suggest that nPKCδ rather than cPKCs influenced activation of caspase-3 and thus proteolytic activation of PKCδ by cDDP. This is consistent with the report that inhibition of nPKCδ by rottlerin partially or totally blocked all parameters of etoposide-induced apoptosis although inhibition of cPKCα and -βI by Gö 6976 had a slight effect on caspase-3 activation and apoptotic morphology in salivary gland acinar cells.28
It is generally believed that caspase-8 is activated by the receptor-mediated pathway whereas caspase-9 is activated in response to DNA damage although there is cross-talk between these two pathways.6,29 We have found that cDDP caused significant activation of caspase-9 in the absence of any activation of caspase-8, suggesting that cDDP exerts its effect primarily through activation of the initiator caspase-9. Rottlerin blocked activation of caspase-9 whereas Gö 6976 was unable to prevent cDDP-induced activation of caspase-9 and its downstream target, caspase-3. These results suggest that rottlerin acts upstream of caspase-9.
We have detected a small amount of procaspases-9, -3 and -7 in the HM fraction. The presence of procaspase-3 in the mitochondria of HeLa cells has been demonstrated both by immunohistochemistry as well as by biochemical fractionations.30 In addition, several investigators have reported that caspases-2, -3 and -9 zymogens may associate with heavy membrane fraction containing mitochondria.30,31,32,33,34 It is believed that these zymogens are released into the cytosol prior to their activation by Cytochrome c and Apaf-1.30,31,32,33,34 The regulation of the membrane-associated caspase-3 was, however, distinct from that of cytosolic caspase-3; for example, membrane-associated caspase-3 was regulated by Bcl-2 but was insensitive to exogenous Cytochrome c whereas cytoplasmic caspase-3 was directly activated by Cytochrome c.31 We have also seen a decrease in procaspases-9, -7 and -3 in the HM membrane fraction following exposure to cDDP but a decrease in proform was associated with an increase in processed forms, suggesting that processing of caspases may in fact take place in the membrane fraction. This was substantiated by the increase in DEVD cleavage activity in the HM fraction as well as cleavage of the substrate PKCδ. It has been reported that during Fas-induced apoptosis, active caspase-7 associates with the mitochondrial and microsomal fractions and cleaves endoplasmic reticular-specific substrate.35 Thus, if active fragments of caspases associate with mitochondria, it can explain the cleavage of these caspases and PKCδ in the membrane fraction. Alternatively, a caspase activation complex could form within the mitochondrial intermembrane space as has been speculated.36 Another way to account for the presence of active caspases-9, -7 and -3 in the heavy membrane fraction is that the large apoptosome containing Apaf-1, caspases-9, -3 and -7 was precipitated with the mitochondria. Although we were unable to detect any Apaf-1 in the membrane fraction, we cannot rule out the possibility that a small amount of Apaf-1 that escaped our detection was in fact associated with the membrane fraction.
The observation that PKCδ is also localized and processed in the mitochondria is intriguing. It has been reported that PKCα may regulate Bcl-2 function in the mitochondria.37 We have shown that inhibition of PKCδ prevents activation of the apical caspase-9. Since release of Cytochrome c is critical for the activation of the caspase cascade, one way to prevent caspase activation is to block Cytochrome c release. In fact, abrogation of mitochondrial Cytochrome c release has been associated with cellular resistance to multiple drugs, including cDDP.23 In addition, mitochondrial translocation of PKCδ has been associated with apoptotic cell death in several cell types, including keratinocytes,38 U-937 and MCF-7 cells.39 Furthermore, PKC activator induced release of Cytochrome c and rottlerin attenuated Cytochrome c release by PKC activators.39 Rottlerin by itself, however, contributed to a detectable release of Cytochrome c.39 This is consistent with our observation that rottlerin caused a small release of Cytochrome c even without any cDDP treatment and that it inhibited Cytochrome c release when cells were exposed to cDDP for a prolonged period. It has been proposed that an initial small amount of Cytochrome c release induced by genotoxic stress is enough to trigger activation of caspase-9 but late Cytochrome c release is a consequence of activated caspases since caspase-3 can cause Cytochrome c release in isolated mitochondria.40 Since activation of mitochondrial PKCδ has been shown to induce release of Cytochrome c,39 we speculate that a small release of Cytochrome c induced by DNA damage causes activation of caspases in the cytosol followed by proteolytic activation of PKCδ in the mitochondria, resulting in more release of Cytochrome c from the mitochondria, thus forming a positive feedback loop. Therefore, while initial release of Cytochrome c by cDDP may not be affected by rottlerin, subsequent release of Cytochrome c that results from activated PKCδ may be inhibited by rottlerin. Recently, however, it has been reported that release of Cytochrome c is kinetically invariant and is not affected by caspase inhibitors.22 Furthermore, it remains to be seen whether rottlerin influences the activity of other mitochondrial apoptogenic factors, such as apoptosis-inducing factor32 or second mitochondria-derived activator protein.41 Nevertheless, we have demonstrated that while release of only a small fraction of Cytochrome c by cDDP was enough to cause caspase activation, no caspase activation was noted when rottlerin was present, suggesting that rottlerin not only prevents Cytochrome c release but also inhibits caspase activation. As has been observed with etoposide-induced cell death,28 we found that rottlerin blocked the entry of damaged cells to the apoptotic pathway rather than affecting cisplatin-induced DNA damage because when cells treated with rottlerin and cDDP were washed and incubated in drug-free media, cells underwent apoptosis. In addition, when cells were continuously exposed to cDDP and rottlerin was added at different times during the cDDP incubation period, the ability of rottlerin to prevent cell death correlated with its ability to block caspase activation and to inhibit late-stage Cytochrome c release. However, when rottlerin was added after cDDP was removed from the medium, it failed to block cDDP-induced cell death. Since DNA damage and caspase activation are coupled, rottlerin may have to be present prior to DNA damage in order to inhibit caspase activation. Thus, rottlerin acts at a step subsequent to DNA damage but prior to caspase-9 activation to regulate cell death by cDDP.
Materials and Methods
Materials
Bisindolylmaleimide, rottlerin and Gö 6976 were purchased from LC Service Corporation (Woburn, MA, USA). MTT and MBP were from Sigma (St. Louis, MO, USA). Polyclonal antibodies to PKCδ and PKCα were from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA) and polyclonal antibody to caspase-8 was from R&D Systems (Minneapolis, MN, USA). Polyclonal antibodies to caspases-3, -9 and Apaf-1, monoclonal antibody to caspase-7 and FasL neutralizing antibody NOK-1 were from Pharmingen (San Diego, CA, USA). Horseradish peroxidase conjugated goat anti-mouse and donkey anti-rabbit antibodies were obtained from JacksonImmuno Research Lab. Inc. (West Grove, PA, USA). Poly(vinylidene difluoride) membrane was from Millipore (Bedford, MA, USA) and enhanced chemiluminescence detection kit was from Amersham (Arlington Heights, IL, USA). Caspase-3 fluorometric assay kit was obtained from BioVision (Palo Alto, CA, USA) and cDDP was a generous gift from Bristol-Myers Squibb Co. (Wallingford, CT, USA).
Cell culture
Human cervical carcinoma HeLa cells were maintained in Dulbecco's modified minimal essential medium supplemented with 10% heat-inactivated fetal bovine serum and 2 mM glutamine, and kept in a humidified incubator at 37°C with 95% air and 5% CO2.
Assessment of cell viability by MTT assay
Exponentially growing cells were plated in microtiter plates and incubated at 37°C in 5% CO2. The following day, cells were pretreated without or with PKC inhibitors and then with different concentrations of cDDP as indicated in the text. The number of viable cells was determined using the dye MTT as previously described.14
Assessment of apoptosis by flow cytometric analysis
Cells were treated with PKC modulators and cDDP as described in the text. At the end of the incubation, cells were harvested and washed with phosphate-buffered saline. Nuclei were isolated, stained with propidium iodide and DNA content was analyzed by a flow cytometer (Coulter Epics).42
PKCδ kinase assay
HeLa cells were lysed in 20 mM Tris-HCl, pH 7.5, 0.1 M NaCl, 1 mM EDTA, 1 mM EGTA, 1% Triton X-100, 0.2 mM Sodium vanadate, 10 mM NaF and protease inhibitors. PKCα or -δ was immunoprecipitated with 1.0 μg antibody and 50 μl of protein A/G agarose. The immunecomplex was washed four times in ice-cold lysis buffer and then with kinase buffer (50 mM Tris-HCl, pH 7.5, 50 mM NaCl, 10 mM MgAc, 0.5 mM EGTA, 0.1 mM DTT). An aliquot of the immunoprecipitate was incubated with assay buffer containing 20 μM ATP, 5 μCi ATP, 0.2 mg/ml MBP in the presence and absence of 10 μM rottlerin and/or 0.2 mg/ml phosphatidylserine and 100 nM TPA. In the PKCα immunokinase assay, 0.5 mM CaCl2 was added with lipid activators to determine Ca2+-dependent cPKCα activity. The reaction mixture was incubated at 30°C for 15 min and the assay was terminated by the addition of SDS–PAGE sample buffer. Proteins were separated by SDS–PAGE and autoradiography was performed. A duplicate gel was run and Western blot analysis was performed with antibody to PKCδ to check for the amount of PKCδ in each assay. To determine the effect of cDDP on PKCδ activity, cells were pretreated with 10 μM rottlerin for 1 h and then treated with or without 20 μM cDDP for another 12 h. MBP phosphorylation was determined with cell extracts in the absence of any lipid cofactors as described before.19
Preparation of cytosolic and mitochondrial extracts
Following treatment with or without rottlerin and cDDP, cells were collected, washed twice with phosphate-buffered saline and subcellular fractionation was performed as described previously.43 Briefly, the pellet was washed with PBS and then swelled in buffer containing 3 mM imidazole, pH 7.4, 0.25 mM sucrose and 10 μg/ml each of leupeptin, aprotinin and soybean trypsin inhibitor for 30 min. Cells were homogenized with 20 strokes of a B-type pestle using a Dounce homogenizer. Nuclei and cell debris were removed by centrifugation at 300×g for 5 min and heavy membrane containing mitochondria were collected by centrifugation at 10 000×g for 15 min. The mitochondrial pellet was washed with isotonic lysis buffer, the supernatant was centrifuged at 150 000×g for 30 min and the resulting supernatant was used as the soluble cytosolic fraction.
Immunoblot analysis
Equivalent volumes of mitochondrial and cytosolic fractions were electrophoresed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred electrophoretically to poly(vinylidene difluoride) membrane. Immunoblot analyses were performed as described before.17 Intensities of immunoreactive proteins were quantified by laser densitometry. In each experiment, the same blot was probed with several antibodies to account for any loading differences.
Caspase assay
DEVDase activity of mitochondrial and cytosolic fractions (equivalent volume) of cells treated with or without cDDP and rottlerin was determined at 37°C using an Ac-DEVD-AFC assay kit and the manufacturer's protocol. The fluorescence liberated from DEVD-AFC was measured using a SpectraMax GeminiXS fluorometer and SOFTmax PRO 3.1.1 software (Molecular Devices, Sunnyvale, CA, USA) with an excitation wavelength of 400-nm and emission wavelength of 505 nm.
Abbreviations
- Ac-DEVD-AFC:
-
Acetyl-Asp-Glu-Val-Asp-7-amino-4-trifluoromethylcoumarine
- Apaf-1:
-
apoptotic protease activating factors
- BIM:
-
bisindolylmaleimide
- cDDP:
-
cis-diamminedichloroplatinum(II)
- CF:
-
catalytic fragment
- Cox-II:
-
cytochrome oxidase subunit II
- HM:
-
heavy membrane
- MBP:
-
myelin basic protein
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- PDBu:
-
phorbol 12,13-dibutyrate
- PKC:
-
protein kinase C
- aPKC:
-
atypical PKC
- cPKC:
-
conventional PKC
- nPKC:
-
novel PKC
- PS:
-
phosphatidylserine
- Rot:
-
rottlerin
- TNF:
-
tumor necrosis factor-α
- TPA:
-
12-O-tetradecanoylphorbol 13-acetate
References
Salvesen GS, Dixit VM . 1997 Caspases: Intracellular signaling by proteolysis Cell 91: 443–446
Cohen GM . 1997 Caspases: the executioners of apoptosis Biochem. J. 326: 1–16
Nunez G, Benedict MA, Hu Y, Inohara N . 1998 Caspases: the proteases of the apoptotic pathway Oncogene 17: 3237–3245
Thornberry NA, Lazebnik Y . 1998 Caspases: enemies within Science 281: 1312–1316
Ashkenazi A, Dixit VM . 1998 Death receptors: signaling and modulation Science 281: 1305–1308
Sun X-M, MacFarlane M, Zhuang J, Wolf BB, Green DR, Cohen GM . 1999 Distinct caspase cascades are initiated in receptor-mediated and chemical-induced apoptosis J. Biol. Chem. 274: 5053–5060
Scaffidi C, Schmitz I, Zhar J, Korsmeyer SJ, Krammer PH, Peter ME . 1999 Differential modulation of apoptosis sensitivity in CD95 Type I and Type II cells J. Biol. Chem. 274: 22532–22538
Bossy-Wetzel E, Green DR . 1999 Caspases induce Cytochrome c release from mitochondria by activating cytosolic factors J. Biol. Chem. 274: 17484–17490
Chu G . 1994 Cellular responses to cisplatin: the roles of DNA-binding proteins and DNA repair J. Biol. Chem. 269: 787–790
Eastman A . 1990 Activation of programmed cell death by anticancer agents: cisplatin as a model system Cancer Cells 2: 275–279
Kerr JFR, Winterford CM, Harmon BV . 1994 Apoptotis: Its significance in cancer and cancer therapy Cancer 73: 2013–2026
Hofmann J, Doppler W, Jakob A, Maly K, Posch L, Uberall F, Grunicke HH . 1988 Enhancement of the antiproliferative activity of cis-diamminedichloroplatinum(II) and nitrogen mustard by inhibitors of protein kinase C Int. J. Cancer 42: 382–388
Isonishi S, Andrews PA, Howell SB . 1990 Increased sensitivity to cis-diamminedichloroplatinum(II) in human ovarian carcinoma cells in response to treatment with 12-O-tetradecanoylphorbol 13-acetate J. Biol. Chem. 265: 3623–3627
Basu A, Teicher BA, Lazo JS . 1990 Involvement of protein kinase C in phorbol ester-induced sensitization of HeLa cells to cis-diamminedichloroplatinum(II) J. Biol. Chem. 265: 8451–8457
Basu A, Kozikowski AP, Sato K, Lazo JS . 1991 Cellular sensitization to cis-diamminedichloroplatinum (II) by novel analogs of protein kinase C activator lyngbyatoxin A Cancer Res. 51: 2511–2514
Basu A, Lazo JS . 1992 Sensitization of human cervical carcinoma cells to cis-diamminedichloroplatinum (II) by bryostatin 1 Cancer Res. 52: 3119–3124
Basu A, Akkaraju GR . 1999 Regulation of caspase activation and cis-diamminedichloroplatinum(II)-induced cell death by protein kinase C Biochemistry 38: 4245–4251
Basu A . 1993 The potential of protein kinase C as a target for anticancer treatment Pharmac. Ther. 59: 257–280
Emoto Y, Manome Y, Meinhardt G, Kisaki H, Kharbanda S, Robertson M, Ghayur T, Wong WW, Kamen R, Weichselbaum R, Kufe D . 1995 Proteolytic activation of protein kinase C δ by an ICE-like protease in apoptosis cells EMBO J. 14: 6148–6156
Ghayur T, Hugunin M, Talanian RV, Ratnofsky S, Quinlan C, Emoto Y, Pandey P, Datta R, Huang Y, Kharbanda S, Allen H, Kamen R, Wong W, Kufe D . 1996 Proteolytic activation of protein kinase C δ by an ICE/CED 3-like protease induces characteristics of apoptosis J. Exp. Med. 184: 2399–2404
Green DR, Reed JC . 1998 Mitochondria and apoptosis Science 281: 1309–1312
Goldstein JC, Waterhouse NJ, Juin P, Evan GI, Green DG . 2000 The coordinate release of cytochrome c during apoptosis is rapid, complete and kinetically invariant Nature Cell Biol. 2: 156–162
Kojima H, Endo K, Moriyama H, Tanaka Y, Alnemri ES, Slapak CA, Teicher B, Kufe D, Datta R . 1998 Abrogation of mitochondrial Cytochrome c release and caspase-3 activation in acquired multidrug resistance J. Biol. Chem. 273: 16647–16650
Martiny-Baron G, Kazanietz MG, Mischak H, Blumberg PM, Kochs G, Hug H, Marme D, Schachtele C . 1993 Selective inhibition of protein kinase C isozymes by the indolocarbazole Gö 6976 J. Biol. Chem. 268: 9194–9197
Gschwendt M, Muller H-J, Kielbassa K, Zang R, Kittstein W, Rincke G, Marks F . 1994 Rottlerin, a novel protein kinase inhibitor Biochem. Biophys. Res. Commun. 199: 93–98
Eichholtz-Wirth H, Marx K . 1998 Clonal variability of radiation-induced cisplain resistant HeLa cells Anticancer Res. 18: 2989–2992
Datta R, Kojima H, Yoshida K, Kufe D . 1997 Caspase-3-mediated cleavage of protein kinase C θ in induction of apoptosis J. Biol. Chem. 272: 20317–20320
Reyland ME, Anderson SM, Matassa AA, Barzen KA, Quissell DO . 1999 Protein kinase C δ is essential for etoposide-induced apoptosis in salivary gland acinar cells J. Biol. Chem. 274: 19115–19123
Ferrari D, Stepczynska A, Los M, Wesselborg S, Schulze-Osthoff K . 1998 Differential regulation and ATP requirement for caspase-8 and caspase-3 activation during CD95- and anticancer drug-induced apoptosis J. Exp. Med. 188: 979–984
Mancini M, Nicholson DW, Roy S, Thornberry NA, Peterson EP, Casciola-Rosen LA, Rosen A . 1998 The caspase-3 precursor has a cytosolic and mitochondrial distribution: Implication for apoptotic signaling J. Exp. Med. 140: 1485–1495
Krebs JF, Armstrong RC, Srinivasan A, Aja T, Wong AM, Aboy A, Sayers R, Pham B, Vu T, Hoang K, Karanewsky DS, Leist C, Schmitz A, Wu JC, Tomaselli KJ, Fritz LC . 1999 Activation of membrane-associated procaspase-3 is regulated by Bcl-2 J. Exp. Med. 144: 915–926
Susin SA, Lorenzo HK, Zamzami N, Marzo I, Brenner C, Larochette N, Prevost M-C, Alzari PM, Kroemer G . 1999 Mitochondrial release of caspase-2 and -9 during the apoptotic process J. Exp. Med. 189: 381–393
Narula J, Pandey P, Arbustin E, Haider N, Narula N, Kolodgie FD, Dal Bello B, Semigran MJ, Bielsa-Masdeu A, Dec GW, Israels S, Ballester M, Virmani R, Saxena S, Kharbanda S . 1999 Apoptosis in heart failure: Release of cytochrome c from mitochondria and activation of caspase-3 in human cardiomyopathy Proc. Natl. Acad. Sci. USA 96: 8144–8149
Krajewski S, Krajewska M, Ellerby LM, Welsh K, Xie Z, Deveraux QL, Salvesen GS, Bredesen DE, Rosenthal RE, Fiskum G, Reed JC . 1999 Release of caspase-9 from mitochondria during neuronal apoptosis and cerebral ischemia Proc. Natl. Acad. Sci. USA 96: 5752–5757
Chandler JM, Cohen GM, MacFarlane M . 1998 Different subcellular distribution of caspase-3 and caspase-7 following Fas-induced apoptosis in mouse liver J. Biol. Chem. 273: 10815–10818
Gottlieb RA . 1999 Mitochondria: Ignition Chamber for Apoptosis Molecular Genetics and Metabolism 68: 227–231
Ruvolo PP, Deng X, Carr BK, May WS . 1998 A functional role for mitochondrial protein kinase Cα in Bcl2 phosphorylation and suppression of apoptosis J. Biol. Chem. 273: 25436–25442
Li L, Lorenzo PS, Bogi K, Blumberg PM, Yuspa SH . 1999 Protein kinase Cδ targets mitochondria, alters mitochondrial membrane potential, and induces apoptosis in normal and neoplastic keratinocytes when overexpressed by an adenoviral vector Mol. Cell. Biol. 19: 8547–8558
Majumder PK, Pandey P, Sun X, Cheng K, Datta R, Saxena S, Kharbanda S, Kufe D . 2000 Mitochondrial translocation of protein kinase C δ in phorbol ester-induced cytochrome c release and apoptosis J. Biol. Chem. 275: 21793–21796
Chen Q, Gong B, Almasan A . 2000 Distinct stages of cytochrome c release from mitochondria: evidence for a feedback amplification loop linking caspase activation to mitochondrial dysfunction in genotoxic stress induced apoptosis Cell Death Differ 7: 227–233
Du C, Fang M, Li Y, Li L, Wang X . 2000 Smac, a mitochondrial protein that promotes cytochrome c-dependent caspase activation by eliminating IAP inhibition Cell 102: 33–42
Vindelov LL, Christensen IBJ, Nissen NI . 1983 A detergent-trypsin method for the preparation of nuclei for flow cytometric DNA analysis Cytometry 3: 323–327
Rudick VL, Rudick MJ, Munoz-Medellin DA, Brun-Zinkernagel A-M, Chang I-F . 1994 Routing of a secretory protein to the endocytic compartment in transfected Madin Carby canine kidney cells Cell. and Mol. Biol. Res. 39: 773–788
Acknowledgements
This work was supported by grants CA71727 and CA85682 from the National Cancer Institute. We thank Dr Victoria L Rudick for her advice on subcellular distribution studies, Dr Richard Kitson for help with digital photography and Dr Baohua Sun for FACS analysis and for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by S Martin
Rights and permissions
About this article
Cite this article
Basu, A., Woolard, M. & Johnson, C. Involvement of protein kinase C-δ in DNA damage-induced apoptosis. Cell Death Differ 8, 899–908 (2001). https://doi.org/10.1038/sj.cdd.4400885
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4400885
Keywords
This article is cited by
-
Plk2-mediated phosphorylation and translocalization of Nrf2 activates anti-inflammation through p53/Plk2/p21cip1 signaling in acute kidney injury
Cell Biology and Toxicology (2023)
-
MicroRNAs as the critical regulators of Cisplatin resistance in ovarian cancer cells
Journal of Ovarian Research (2021)
-
Role of microRNAs in epidermal growth factor receptor signaling pathway in cervical cancer
Molecular Biology Reports (2020)
-
Growth Hormone differentially modulates chemoresistance in human endometrial adenocarcinoma cell lines
Endocrine (2017)
-
Modulation of PKC signaling and induction of apoptosis through suppression of reactive oxygen species and tumor necrosis factor receptor 1 (TNFR1): key role of quercetin in cancer prevention
Tumor Biology (2015)