Abstract
Background:
Bladder cancer is the second most common cancer of the urinary system. Early diagnosis of this tumour and estimation of risk of future progression after initial transuretherial resection have a significant impact on prognosis. Although there are several molecular markers for the diagnosis and prognosis for this tumour, their accuracy is not ideal. Previous reports have shown that UHRF1 (ubiquitin-like with PHD and ring-finger domains 1) is essential for cellular proliferation. In this study, we examined whether UHRF1 can be a novel molecular marker of bladder cancer.
Methods:
We performed real-time TaqMan quantitative reverse transcription–PCR and immunohistochemistry to examine expression levels of UHRF1 in bladder and kidney cancers.
Results:
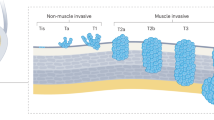
Significant overexpression of UHRF1 was observed in bladder cancer. The overexpression was correlated with the stage and grade of the cancer. Although UHRF1 expression in muscle-invasive cancer was greater than in non-invasive (pTa) or superficially invasive (pT1) cancers, UHRF1 could still be detected by immunohistochemistry in these early-stage cancers. Overexpression of UHRF1 in bladder cancer was associated with increased risk of progression after transurethral resection. High expression of UHRF1 in kidney cancer was also observed. But the increased levels of UHRF1 in kidney cancer were less significant compared with those in bladder cancer.
Conclusion:
Our result indicates that an immunohistochemistry-based UHRF1 detection in urine sediment or surgical specimens can be a sensitive and cancer-specific diagnostic and/or prognosis method, and may greatly improve the current diagnosis based on cytology.
Similar content being viewed by others
Main
Bladder cancer is the second most common cancer of the urinary system. Approximately 356 600 new cases of bladder cancer are diagnosed each year worldwide and, in terms of overall cancer frequency, it is ranked as ninth (International Agency for Research on Cancer, The GLOBOCAN 2002 database, http://www-dep.iarc.fr/). According to Cancer Research UK (http://www.cancerresearchuk.org/), bladder cancer is the fourth most common cancer in males in the United Kingdom. The highest rates of bladder incidence are found in industrially developed countries, particularly in North America and Western Europe (Parkin et al, 2005). In these countries, approximately 90% of bladder tumours are transitional cell carcinomas (TCCs), whereas the remaining 10% are squamous cell carcinomas and adenocarcinomas (Stein et al, 2001).
There are several potential biomarkers for diagnosis and prognosis for bladder cancer, including nuclear matrix protein-22 (NMP-22), human complement factor H-related protein, telomerase, fibrin degradation product, and hyaluronic acid (Dey, 2004). Among these, only two biomarkers, NMP-22 and human complement factor H-related protein, are in clinical use. Although these two markers are in clinical use, sensitivity and specificity of these markers are not perfect (van Rhijn et al, 2005); NMP-22 staining shows false-positivity reactions in patients with haematuria, and the BTA stat/BTA TRAK assay, which detects human complement factor H-related protein, shows false-positivity reactions in patients with urinary tract inflammation, recent genitourinary tumours and in cases of bladder stone (Dey, 2004). Cytology is still the most accurate diagnosis method, although sensitivity is not enough high (van Rhijn et al, 2005). Thus, discovery of a novel biomarker, which is sensitive and specific for bladder cancer, is an urgent subject.
Kidney cancer, which accounts for 2–3% of all adult malignant neoplasms, is the most lethal of the urologic cancers. Traditionally, more than 40% of patients with kidney cancer have died of their cancer, in contrast with the 20% mortality rates associated with prostate and bladder carcinomas (Pantuck et al, 2001). In 2007, two molecular targeting drugs, sorafenib and sunitinib, were approved by the Food and Drug Administration of the United States Department of Health and Human Service, and are in clinical use. These two drugs are tyrosine kinase inhibitors that have antitumor activity in advanced renal cell carcinoma. They may improve the mortality rates of this cancer, although these drugs have side effects, such as hand–foot syndrome, rash, fatigue, hypertension, and diarrhoea (Grandinetti and Goldspiel, 2007). Current diagnosis mainly relies on ultrasound and computed tomographic-scan. There are no good diagnostic and prognostic markers for kidney cancer.
UHRF1 (ubiquitin-like with PHD and ring-finger domains 1), also known as ICBP90, was identified as a protein, whose expression is only detectable in proliferating cells, not in quiescent cells (Hopfner et al, 2000; Unoki et al, 2004). Recently, it was revealed that UHRF1 plays a central role in transferring DNA methylation status from mother cells to daughter cells. Its SET and RING finger-associated (SRA) domain recognises hemimethylated DNA that appears in newly synthesised daughter DNA strands during duplication of DNA strands through the S phase (Arita et al, 2008; Avvakumov et al, 2008; Hashimoto et al, 2008). The UHRF1 recruits DNA methyltransferase 1 (DNMT1) to the site with proliferating cell nuclear antigen (PCNA) and methylates the newly synthesised strands (Sharif et al, 2007; Achour et al, 2008). The UHRF1 promotes G1/S transition (Arima et al, 2004; Jeanblanc et al, 2005) and is a direct target of E2F transcription factor 1 (E2F1) (Mousli et al, 2003; Unoki et al, 2004; Abbady et al, 2005). The tumour suppressor p53, which is deficient in 50% of all human cancers (Hussain and Harris, 2000), indirectly downregulates UHRF1 through the upregulation of p21/WAF1 and subsequent deactivation of E2F1 (Arima et al, 2004). Expression of UHRF1 is upregulated in various cancers, including breast, prostate, lung, astrocytomas, pancreatic cancers, and cervical cancer (Mousli et al, 2003; Unoki et al, 2004; Crnogorac-Jurcevic et al, 2005; Jenkins et al, 2005; Lorenzato et al, 2005; Oba-Shinjo et al, 2005). Overexpression of UHRF1 in these cancers may be partially due to the inactivation of p53, although there are most probably several pathways which regulate UHRF1. Knockdown of UHRF1 expression in cancer cells suppressed cell growth significantly, indicating that UHRF1 is essential for progression of cancers (Unoki et al, 2004).
Here, we report that the overexpression of UHRF1 in bladder tumour is associated with malignant potential of the cancers as defined by the stage and grade (Lopez-Beltran, 2008). The UHRF1 can be detected in tissue samples and urine sediment from patients with bladder cancer, and thus can be a diagnostic and/or prognostic marker.
Materials and methods
Tissue samples and RNA preparation
A total of 124 surgical specimens of primary urothelial carcinoma were collected (Table 1), either by cystectomy or transurethral resection of bladder tumour (TURBT), and snap-frozen in liquid nitrogen. Twenty-one specimens of normal bladder urothelial tissue were collected from the areas of macroscopically normal bladder urothelium in patients with no evidence of malignancy. Five sequential sections of 7 μm thick were cut from each tissue and stained using Histogene staining solution (Arcturus, Oxnard, CA, USA) following the manufacturer's protocol, and assessed for cellularity and tumour grade by an independent consultant urohistopathologist. Slides were then transferred for microdissection using a Pix Cell II laser capture microscope (Arcturus). This technique uses a low-power infrared laser to melt a thermoplastic film over the cells of interest, to which the cells become attached.
Approximately 10 000 cells were microdissected from both stromal and epithelial/tumour compartments in each tissue. RNA was extracted using an RNeasy Micro Kit (Qiagen, Crawley, UK). Areas of cancer or stroma containing significant inflammatory cell infiltration were avoided to prevent contamination (Wallard et al, 2006). Total RNA was treated with DNase and then quantitative reverse transcription–PCR (qRT–PCR) was performed as described below. Given the low yield of RNA from such small samples, NanoDrop quantification was not performed, but correction for the endogenous 18S cycle threshold (CT) value was used as an accurate measure of the amount of intact starting RNA. To validate the accuracy of microdissection, primers and probes for Vimentin and Uroplakin were sourced, and qRT–PCR was performed according to the manufacturer's instructions (Assays on demand, Applied Biosystems, Warrington, UK). Vimentin is primarily expressed in mesenchymally derived cells, and was used as a stromal marker. Uroplakin is a marker of urothelial differentiation and is preserved in up to 90% of epithelially derived tumours (Olsburgh et al, 2003).
Seventy-two kidney tumours (Supplementary Table 1), 6 oncocytomas, and 21 normal kidneys were collected from the Department of Urology in Addenbroke's hospital. Complementary DNAs (cDNAs) from 12 normal tissues and paraffin-embedded tissue slides for immunohistochemistry described below were purchased from BioChain Institute (Hayward, CA, USA). A paraffin-embedded tissue slide (Case 1 in Figure 2) is obtained from Iwate Medical University with written informed consent (Takata et al, 2007). Detailed information of clinical samples on the slides is shown in Supplementary Table 2–4. Use of tissues for this study was approved by Cambridgeshire Local Research Ethics Committee (Ref 03/018). We have removed the possibility of genomic DNA contamination by PCR using a primer set that can amplify genomic DNA (data not shown).
Immunohistochemical staining of UHRF1 in 13 bladder tumour cases. (A) Expression of UHRF1 in 11 transitional cell carcinomas and two adenocarcinomas with the different stage and grade. High expression of UHRF1 was detected only in nucleus of cancer cells, not in stromal cells. (B) Expression of UHRF1 in normal tissues including the bladder, lung, liver, heart, and kidney. No expression was observed in these normal tissues. Original magnifications, × 200 (top), and × 400 (bottom). (C) Representative images of normal IgG staining as a negative control (Case 11 used for Figure 2A). Original magnifications, × 200 (top), and × 400 (bottom).
TaqMan real-time qRT–PCR
For TaqMan real-time qRT–PCRs, specific primers and probes, which strictly amplify only cDNA not genomic DNA, for human UHRF1 and β2-microglobulin were purchased from Applied Biosystems (Carlsbad, CA, USA; ID: Hs00273589_m1, and 4333766F, respectively). The PCRs were performed using the ABI Prism 7700 Sequence Detection System (Applied Biosystems) following the manufacturer's protocol. Amplification conditions were 2 min at 50 °C, 10 min at 95 °C and then 40 cycles each consisting of 15 s at 95 °C and 1 min at 60 °C. The CT value obtained by UHRF1 amplification was compared among the samples after normalisation using β2-microglobulin expression levels as an endogenous control.
Statistical analysis
Kruskal–Wallis test was performed for comparison of the UHRF1 expression levels among three or more different groups. Mann–Whitney U-test nonparametric analysis was performed for comparison of the UHRF1 expression levels between two groups. P-value of 0.05 or less was considered significant.
Immunohistochemical staining analysis
The expression patterns of UHRF1 and p53 in bladder tumours, and normal human tissues were examined by immunohistochemistry as described previously (Unoki et al, 2004). Briefly, slides of paraffin-embedded bladder tumour specimens and normal human tissues (the bladder, heart, liver, kidney, and lung) were processed under high pressure (125 °C, 30 s) in antigen-retrieval solution, high pH 9 (S2367, Dako Cytomation, Carpinteria, CA, USA), treated with peroxidase blocking regent, and then treated with protein blocking regent (K130, X0909, Dako Cytomation). Tissue sections were incubated with the mouse anti-UHRF1 monoclonal antibody (1 : 400, BD Bioscience, Franklin Lakes, NJ, USA) or mouse p53 antibody (DO-1, 1 : 100, Santa Cruz), or normal mouse IgG (1 : 100, Santa Cruz, Santa Cruz, CA, USA) followed by HRP-conjugated secondary antibody (Dako Cytomation). Antigen was visualised with substrate chromogen (Dako liquid DAB chromogen; Dako Cytomation). Finally, tissue specimens were stained with Mayer’s haematoxylin (Muto pure chemicals Ltd, Tokyo, Japan) for 20 s to discriminate the nucleus from the cytoplasm.
Results
UHRF1 mRNA was highly expressed in urinary system tumours, but not in a benign neoplasm of kidney and several other normal tissues
Expression levels of UHRF1 in six oncocytomas (benign neoplasm in kidney), 71 kidney tumours (Supplementary Table 1), and 124 bladder tumours (Table 1) including 11 upper tract TCCs from UK patients were examined by TaqMan real-time qRT—PCR. As controls, 21 normal kidneys, 21 normal bladders, and other 12 normal tissues (the brain, breast, colon, oesophagus, eye, heart, liver, lung, pancreas, rectum, spleen, and stomach) were examined. The UHRF1 was significantly overexpressed in bladder tumours (P<0.0001, Mann–Whitney's U-test, Figure 1), especially in 12 upper tract TCCs (P<0.0001, Kruskal–Wallis test, Figure 1): 10 percentile of the upper tract TCCs is higher than 50 percentile of the bladder-origin bladder cancers. The stages of the upper tract TCCs were as follows: four patients with pT1, one patient with pT2, four patients with pT3, two patients with pT4, and one of unknown stage. The grade of the upper tract TCC was as follows: eight patients with grade II and four patients with grade III. Because all four patients with pT1 also showed high expression of UHRF1, this high expression of UHRF1 may correlate with the origin of anatomic sites, besides the levels of malignancies as we described below. Base line characteristics of the bladder tumour patients are shown in Table 1. Next, we compared UHRF1 expression in bladder tumours with that in 12 normal tissues, 21 normal kidneys, 6 oncocytomas, and 72 kidney tumours (Figure 1). Expression levels of UHRF1 in the oncocytomas and in normal kidney were not different statistically (P=0.9535). In contrast, expression of UHRF1 in kidney tumours was significantly increased compared with in normal kidney and in oncocytomas (P<0.0001 and 0.0206, respectively). However, the levels of upregulation of UHRF1 in bladder tumours were much higher than that in kidney tumours (P<0.0001), suggesting that UHRF1 might be a sensitive tool for detection of bladder tumours, especially the upper tract TCCs, which are currently often found in advanced stages.
Expression levels of UHRF1 mRNA in urinary system tumours and normal tissues detected by TaqMan real-time qRT–PCR. Expression of UHRF1 in 12 different normal tissues, 21 normal kidneys, 6 oncocytomas, 71 kidney tumours, 21 normal bladders, and 124 bladder tumours, including 112 bladder located cancers and 12 transitional cell carcinoma occurred in the upper tract, were compared. Expression of UHRF1 differed among the seven groups (P<0.0001, Kruskal–Wallis’ test). Expression of UHRF1 in the kidney tumours was higher than that in the normal kidneys and also in the oncocytomas significantly (P<0.0001 and 0.0206, respectively, Mann–Whitney’s U-test), but expression levels of UHRF1 in the bladder tumours were much higher than those in the kidney tumours (P<0.0001, Mann–Whitney’s U-test). Among the bladder cancers, expression of UHRF1 was significantly high in the upper tract TCCs (n=11) compared with the bladder-origin bladder tumours (n=112) (Mann–Whitney’s U-test; P=0.0042). β2-microglobulin was used for normalisation. Asterisk indicates statistically significant P-values.
Overexpression of UHRF1 was further confirmed in bladder tumours from 36 Japanese patients by microarray analysis (Takata et al, 2005, 2007). Expression of UHRF1 in these bladder tumours was compared with the corresponding adjacent normal tissues from the same patients, and tumour/normal ratio was obtained. In the result, UHRF1 was overexpressed more than twice in 86% of these bladder-cancer cases (data not shown), indicating that overexpression of UHRF1 in bladder cancer is probably common worldwide.
Overexpression of UHRF1 in bladder tumours was verified at the protein level
Overexpression of UHRF1 in bladder tumours was confirmed at the protein level by immunohistochemistry. Thirteen cases of bladder tumours including 11 cases of TCC and two cases of adenocarcinoma were examined. Detailed clinical information of each case is shown in Supplementary Table 2. Expression of UHRF1 was observed only in cancer cells, not in stromal cells (Figure 2A). Expression of UHRF1 was detectable even in bladder tumours at non-advanced stages (grades I and II, pTa/pT1N0M0), although stronger UHRF1 staining was detected in bladder tumours of more advanced stages (pT2–pT4), and grades (grades II and III). No UHRF1 staining was observed in normal tissues including the bladder, lung, liver, heart, and kidney (Figure 2B, Supplementary Table 3). Normal mouse IgG was served as a negative control in each case. Figure 2C shows a representative datum. We also performed immunohistochemistry using the kidney specimens. Staining in kidney tumours was weak compared with bladder tumours (Figure 3A and Supplementary Table 4), although overexpression of UHRF1 at the mRNA level was associated with several characteristics of kidney tumour patients, including 5-year survival rates, pathological staging, and histological grade (Figure 3B and C, Supplementary Table 1).
Expression of UHRF1 in kidney cancer. (A) UHRF1 expression in kidney cancers examined by immunohistochemistry. Clinical information of each individual is shown in Supplementary Table S3. Magnification level is × 400. (B) Expression levels of UHRF1 correlate with 5-year survival rate of kidney tumours detected by TaqMan qRT–PCR. Patients were categorised into two groups by expression levels of UHRF1. The UHRF1 high expression group is a group, which expresses UHRF1 eight or more (⩾8) and the low expression group is a group, which expresses UHRF1 less than eight-fold (<8) compared with average of UHRF1 expression level in normal kidney from 21 individuals as 1.0. In the result of Kaplan–Meier survival analysis, the UHRF1 high expression group showed significantly poor survival rate compared with the UHRF1 low expression group (P=0.0096: Log-rank test). β2-microglobulin was used for normalisation. (C) Expression levels of UHRF1 correlated with histological grade of kidney tumours detected by TaqMan qRT–PCR. Patients were categorised into four groups by histological grade (1 to 4). High expression of UHRF1 correlated with advanced grade (P=0.0093: Kruskal–Wallis’s test). β2-microglobulin was used for normalisation. (D) Expression levels of UHRF1 correlated with pathological staging and histological grade of renal cancers detected by TaqMan qRT–PCR. Patients were categorised into three groups with pathological stages, pT1 to pT3. High expression of UHRF1 correlated with advanced stage (P=0.0005: Kruskal–Wallis’s test). β2-microglobulin was used for normalisation.
Expression of UHRF1 correlated with the stage and grade of bladder tumours, and the risk of recurrence and progression after TURBT
Although expression of UHRF1 was not associated with difference of gender, numbers of tumour, tumour size, growth pattern (papillary or solid), incidence of recurrence, survival status after 5 years from surgery, and smoking history (P>0.05, Mann–Whitney's U-test, Supplementary Figure 1), we found that the expression of UHRF1 correlated with stages (pTa–pT4) and grades (grades I–III) (Figure 4A and B). Expression levels of UHRF1 in superficial bladder tumours (pTa and pT1) and invasive bladder tumours (pT2–pT4) were both significantly higher than those in normal bladders by Mann–Whitney's U-test (P=0.0063 and 0.0034, respectively). Although UHRF1 expression in invasive bladder tumours was not significantly higher than that in superficial bladder tumours statistically, expression of UHRF1 differed among the three groups by Kruskal–Wallis test (P=0.0058). Expression of UHRF1 also differed among four groups with the different grade by Kruskal–Wallis test (P=0.0156): although the distribution of UHRF1 expression in each group had a relatively wide range, the median value of UHRF1 expression in each group increased in parallel with increased grade. Expression levels of UHRF1 in tumours of grade-II and grade-III were upregulated compared with normal bladders by Mann–Whitney's U-test (P=0.0033 and 0.0041, respectively). Expression levels of UHRF1 in patients with the high-risk superficial bladder cancer were higher than that found in the low-risk group (Mann–Whitney's U-test: P=0.0350, Figure 4C).
Expression of UHRF1 correlated with the stage, grade, and the risk after TURBT. (A) Expression of UHRF1 in 21 normal bladders, 71 superficial bladder tumours (T-category is pTa and pT1), and 41 invasive bladder tumours (T-category is pT2, pT3, and pT4) detected by TaqMan qRT–PCR. Expression levels of UHRF1 in superficial bladder tumours and in invasive tumours were significantly higher compared with those in normal bladders by Mann–Whitney’s U-test (P=0.0063 and 0.0034, respectively). Although its expression in superficial tumours and invasive tumours did not differ (P=0.2442, Mann–Whitney’s U-test), it differed among the three different groups (P=0.0058, Kruskal–Wallis’ test). β2-microglobulin was used for normalisation. (B) Expression of UHRF1 differed among four groups with the different grade (P=0.0156, Kruskal–Wallis’ test) detected by TaqMan qRT–PCR. Expression of UHRF1 in grades II and III tumour was higher than that in the normal bladders (P=0.0033 and 0.0041). β2-microglobulin was used for normalisation. (C) Significant high expression of UHRF1 in the high-risk group after TURBT (n=23) was observed compared with that in the low-risk group (n=7) by Mann–Whitney’s U-test (P=0.0350). Asterisk indicates statistically significant P-values. β2-microglobulin was used for normalisation.
Disucussion
Ubiquitin-like with PHD and ring-finger domains 1 is a protein which is overexpressed in various cancers (Mousli et al, 2003; Unoki et al, 2004; Crnogorac-Jurcevic et al, 2005; Jenkins et al, 2005; Lorenzato et al, 2005; Oba-Shinjo et al, 2005) and the overexpression is thought to be essential for malignant cancer progression (Hopfner et al, 2000; Arima et al, 2004; Unoki et al, 2004). Thus, we examined expression of UHRF1 in urinary system cancers collected in the United Kingdom and found that UHRF1 was moderately upregulated in the kidney tumours and significantly overexpressed in bladder tumours, especially in the upper tract TCCs at the mRNA level. Overexpression of UHRF1 was further confirmed using Japanese cases, indicating that the overexpression of UHRF1 is not specific for patients in the United Kingdom, but common worldwide.
We verified the overexpression of UHRF1 in bladder tumour tissues at the protein level by immunohistochemistry. Whereas, we did not detect significant overexpression of UHRF1 in kidney tumours at the protein level, although the high expression of UHRF1 in kidney tumours at the mRNA level correlated with poor survival rate, advanced pathological staging, and increasing histological grade. It is probably because of the different sensitivity between the two methods for detecting mRNA and protein (Shariat et al, 2003) or of the different stability between UHRF1 mRNA and UHRF1 protein. Thus, detection of UHRF1 mRNA overexpression in surgical specimen might be useful as a prognosis tool in kidney cancer, but immunohistochemical staining of UHRF1 in the cancer may not be useful.
Because one of upstream regulators of UHRF1 is p53, we examined correlation between expression of UHRF1, p53, and p21, which is a downstream gene of p53, by immunohistochemistry and TaqMan qRT–PCR, respectively. In the result, we observed accumulation of stabilised p53 protein, which is probably mutated, in cancer tissues at grades II and III except one case (Supplementary Figure 2). However, we did not observe any accumulation of p53 in cancer tissues at grade I, although overexpression of UHRF1 was observed in this grade. There was no relationship between expression levels of UHRF1 and p21 at the mRNA level (data not shown). Thus, UHRF1 is much superior to p53 as a potential diagnostic marker of bladder cancer. This result is concordant with the fact that p53 is mutated only in 10–30% of bladder cancer cases and is rarely mutated in kidney cancer (Tomasino et al, 1994; Berggren et al, 2001; Lorenzo Romero et al, 2004).
Over 75% bladder tumour patients have one or more superficial bladder tumours, and two-thirds of them will develop recurrent disease (Lutzeyer et al, 1982), with 10–20% progressing to an invasive phenotype (Torti and Lum, 1984). The outcome of patients with invasive tumours remains still poor, with distant metastasis occurring in over 50% within 2 years and an average 5-year survival of only 50% (Raghavan et al, 1990).
Thus, diagnosis of bladder cancer at non-advanced stage and also precise estimation of the risk after the TURBT are very important for prognosis of patients. Currently, the risk after the surgery is estimated by a scoring system and risk tables developed by European Organization for Research and Treatment of Cancer (EORTC). The EORTC scoring system was developed based on the six most significant clinical and pathological factors, which are tumour stage, tumour grade, numbers of tumour, tumour size, earlier recurrence rate, and presence of carcinoma in situ. Bladder cancer patients with pTaG1 tumours (50% of all patients) are at very low risk, and those with carcinoma in situ (CIS) or with pT1G3 tumours are at the highest risk (15% of all patients). Intermediate-risk patients are those with pTa/pT1 G1/G2 disease who develop multiple recurrent cancers (35% of all patients). In our result, although expression of UHRF1 was not associated with numbers and size of bladder tumours, high expression of UHRF1 correlated with tumour malignancy defined by the stage and grade. High expression of UHRF1 was also associated with high risk after TURBT, probably because reflecting the association between high expression of UHRF1 and stage, and/or grade. On the basis of these results, detection of UHRF1 in tissue samples after TURBT will be a prognostic marker of future recurrence and may help to determine the risk.
Because UHRF1 was significantly overexpressed in the upper tract TCCs, UHRF1 might be a useful diagnostic marker especially for this type of tumour. The upper tract TCCs are often very malignant when it is diagnosed, partially because it is relatively difficult to find at an early stage. If the cancer is found at an early stage, the prognosis of patients is improved. The development of a sensitive urine-based detection marker is still being sought. Examination of voided urine or bladder barbotage for exfoliated cancer cells is useful for diagnosis of urothelial tumours anywhere in the urinary tract, from the calyx, through the ureters, into bladder and urethra. However, cytological interpretation can be problematic; low cellular yields, atypia, degenerative changes, urinary tract infections, stones and intravesical instillations hamper a correct diagnosis. Because the current two biomarker tests in clinical use, NMP-22 detection and BTA stat/BTA TRAK assay, can be hampered by existence of bleeding, inflammation, recent genitourinary tumours, and bladder stone (Dey, 2004), these markers have not improved the traditional cytology-based bladder cancer diagnosis largely. Thus, cytology is still the mainstay for diagnosing bladder cancer. Because the expression of UHRF1 in peripheral blood mononuclear cells was very low (Supplementary Figure 3), the presence of these cells in urine would not impede the diagnosis. In addition, expression of UHRF1 was not detected in adjacent normal bladder tissues by immunohistochemistry. Thus, contamination of these stromal cells also would not disturb the diagnosis, either. Therefore, in our conclusion, an immunohistochemistry-based UHRF1 detection in urine sediment can be a sensitive and cancer-specific diagnostic method, and may greatly improve the current diagnosis based on cytology.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abbady AQ, Bronner C, Bathami K, Muller CD, Jeanblanc M, Mathieu E, Klein JP, Candolfi E, Mousli M (2005) TCR pathway involves ICBP90 gene down-regulation via E2F binding sites. Biochem Pharmacol 70: 570–579
Achour M, Jacq X, Ronde P, Alhosin M, Charlot C, Chataigneau T, Jeanblanc M, Macaluso M, Giordano A, Hughes AD, Schini-Kerth VB, Bronner C (2008) The interaction of the SRA domain of ICBP90 with a novel domain of DNMT1 is involved in the regulation of VEGF gene expression. Oncogene 27: 2187–2197
Arima Y, Hirota T, Bronner C, Mousli M, Fujiwara T, Niwa S, Ishikawa H, Saya H (2004) Down-regulation of nuclear protein ICBP90 by p53/p21Cip1/WAF1-dependent DNA-damage checkpoint signals contributes to cell cycle arrest at G1/S transition. Genes Cells 9: 131–142
Arita K, Ariyoshi M, Tochio H, Nakamura Y, Shirakawa M (2008) Recognition of hemi-methylated DNA by the SRA protein UHRF1 by a base-flipping mechanism. Nature 455: 818–821
Avvakumov GV, Walker JR, Xue S, Li Y, Duan S, Bronner C, Arrowsmith CH, Dhe-Paganon S (2008) Structural basis for recognition of hemi-methylated DNA by the SRA domain of human UHRF1. Nature 455: 822–825
Berggren P, Steineck G, Adolfsson J, Hansson J, Jansson O, Larsson P, Sandstedt B, Wijkstrom H, Hemminki K (2001) p53 mutations in urinary bladder cancer. Br J Cancer 84: 1505–1511
Crnogorac-Jurcevic T, Gangeswaran R, Bhakta V, Capurso G, Lattimore S, Akada M, Sunamura M, Prime W, Campbell F, Brentnall TA, Costello E, Neoptolemos J, Lemoine NR (2005) Proteomic analysis of chronic pancreatitis and pancreatic adenocarcinoma. Gastroenterology 129: 1454–1463
Dey P (2004) Urinary markers of bladder carcinoma. Clin Chim Acta 340: 57–65
Grandinetti CA, Goldspiel BR (2007) Sorafenib and sunitinib: novel targeted therapies for renal cell cancer. Pharmacotherapy 27: 1125–1144
Hashimoto H, Horton JR, Zhang X, Bostick M, Jacobsen SE, Cheng X (2008) The SRA domain of UHRF1 flips 5-methylcytosine out of the DNA helix. Nature 455: 826–829
Hopfner R, Mousli M, Jeltsch JM, Voulgaris A, Lutz Y, Marin C, Bellocq JP, Oudet P, Bronner C (2000) ICBP90, a novel human CCAAT binding protein, involved in the regulation of topoisomerase IIalpha expression. Cancer Res 60: 121–128
Hussain SP, Harris CC (2000) Molecular epidemiology and carcinogenesis: endogenous and exogenous carcinogens. Mutat Res 462: 311–322
Jeanblanc M, Mousli M, Hopfner R, Bathami K, Martinet N, Abbady AQ, Siffert JC, Mathieu E, Muller CD, Bronner C (2005) The retinoblastoma gene and its product are targeted by ICBP90: a key mechanism in the G1/S transition during the cell cycle. Oncogene 24: 7337–7345
Jenkins Y, Markovtsov V, Lang W, Sharma P, Pearsall D, Warner J, Franci C, Huang B, Huang J, Yam GC, Vistan JP, Pali E, Vialard J, Janicot M, Lorens JB, Payan DG, Hitoshi Y (2005) Critical role of the ubiquitin ligase activity of UHRF1, a nuclear RING finger protein, in tumor cell growth. Mol Biol Cell 16: 5621–5629
Lopez-Beltran A (2008) Bladder cancer: clinical and pathological profile. Scand J Urol Nephrol Suppl 218: 95–109
Lorenzato M, Caudroy S, Bronner C, Evrard G, Simon M, Durlach A, Birembaut P, Clavel C (2005) Cell cycle and/or proliferation markers: what is the best method to discriminate cervical high-grade lesions? Hum Pathol 36: 1101–1107
Lorenzo Romero JG, Salinas Sanchez AS, Gimenez Bachs JM, Sanchez Sanchez F, Escribano Martinez J, Hernandez Millan IR, Segura Martin M, Virseda Rodriguez JA (2004) p53 Gene mutations in superficial bladder cancer. Urol Int 73: 212–218
Lutzeyer W, Rubben H, Dahm H (1982) Prognostic parameters in superficial bladder cancer: an analysis of 315 cases. J Urol 127: 250–252
Mousli M, Hopfner R, Abbady AQ, Monte D, Jeanblanc M, Oudet P, Louis B, Bronner C (2003) ICBP90 belongs to a new family of proteins with an expression that is deregulated in cancer cells. Br J Cancer 89: 120–127
Oba-Shinjo SM, Bengtson MH, Winnischofer SM, Colin C, Vedoy CG, de Mendonca Z, Marie SK, Sogayar MC (2005) Identification of novel differentially expressed genes in human astrocytomas by cDNA representational difference analysis. Brain Res Mol Brain Res 140: 25–33
Olsburgh J, Harnden P, Weeks R, Smith B, Joyce A, Hall G, Poulsom R, Selby P, Southgate J (2003) Uroplakin gene expression in normal human tissues and locally advanced bladder cancer. J Pathol 199: 41–49
Pantuck AJ, Zisman A, Belldegrun AS (2001) The changing natural history of renal cell carcinoma. J Urol 166: 1611–1623
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global Cancer Statistics, 2002. CA-Cancer J Clin 55: 74–108
Raghavan D, Shipley WU, Garnick MB, Russell PJ, Richie JP (1990) Biology and management of bladder cancer. N Engl J Med 322: 1129–1138
Shariat SF, Roudier MP, Wilcox GE, Kattan MW, Scardino PT, Vessella RL, Erdamar S, Nguyen C, Wheeler TM, Slawin KM (2003) Comparison of immunohistochemistry with reverse transcription-PCR for the detection of micrometastatic prostate cancer in lymph nodes. Cancer Res 63: 4662–4670
Sharif J, Muto M, Takebayashi S, Suetake I, Iwamatsu A, Endo TA, Shinga J, Mizutani-Koseki Y, Toyoda T, Okamura K, Tajima S, Mitsuya K, Okano M, Koseki H (2007) The SRA protein Np95 mediates epigenetic inheritance by recruiting Dnmt1 to methylated DNA. Nature 450: 908–912
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, Skinner E, Bochner B, Thangathurai D, Mikhail M, Raghavan D, Skinner DG (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol 19: 666–675
Takata R, Katagiri T, Kanehira M, Shuin T, Miki T, Namiki M, Kohri K, Tsunoda T, Fujioka T, Nakamura Y (2007) Validation study of the prediction system for clinical response of M-VAC neoadjuvant chemotherapy. Cancer Sci 98: 113–117
Takata R, Katagiri T, Kanehira M, Tsunoda T, Shuin T, Miki T, Namiki M, Kohri K, Matsushita Y, Fujioka T, Nakamura Y (2005) Predicting response to methotrexate, vinblastine, doxorubicin, and cisplatin neoadjuvant chemotherapy for bladder cancers through genome-wide gene expression profiling. Clin Cancer Res 11: 2625–2636
Tomasino RM, Morello V, Tralongo V, Nagar C, Nuara R, Daniele E, Curti M, Orestano F (1994) p53 expression in human renal cell carcinoma: an immunohistochemical study and a literature outline of the cytogenetic characterization. Pathologica 86: 227–233
Torti FM, Lum BL (1984) The biology and treatment of superficial bladder cancer. J Clin Oncol 2: 505–531
Unoki M, Nishidate T, Nakamura Y (2004) ICBP90, an E2F-1 target, recruits HDAC1 and binds to methyl-CpG through its SRA domain. Oncogene 23: 7601–7610
van Rhijn BW, van der Poel HG, van der Kwast TH (2005) Urine markers for bladder cancer surveillance: a systematic review. Eur Urol 47: 736–748
Wallard MJ, Pennington CJ, Veerakumarasivam A, Burtt G, Mills IG, Warren A, Leung HY, Murphy G, Edwards DR, Neal DE, Kelly JD (2006) Comprehensive profiling and localisation of the matrix metalloproteinases in urothelial carcinoma. Br J Cancer 94: 569–577
Acknowledgements
We thank Professor Tomoaki Fujioka for providing us a pTa bladder cancer specimen, and Drs Ryo Takata, Hitoshi Zembutsu, Yoichiro Kato, Shinya Hayami, Masanori Yoshimatsu, Chikako Fukukawa, and Atsushi Takano for very useful advice and discussion. We acknowledge the support of NIHR and the Cambridge Biomedical Research Centre funding in supporting our bio-repository.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Unoki, M., Kelly, J., Neal, D. et al. UHRF1 is a novel molecular marker for diagnosis and the prognosis of bladder cancer. Br J Cancer 101, 98–105 (2009). https://doi.org/10.1038/sj.bjc.6605123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605123
Keywords
This article is cited by
-
AKT1 regulates UHRF1 protein stability and promotes the resistance to abiraterone in prostate cancer
Oncogenesis (2023)
-
UHRF1 overexpression promotes osteosarcoma metastasis through altered exosome production and AMPK/SEMA3E suppression
Oncogenesis (2022)
-
UHRF1-KAT7-mediated regulation of TUSC3 expression via histone methylation/acetylation is critical for the proliferation of colon cancer cells
Oncogene (2020)
-
BSA-bounded p-cresyl sulfate potentiates the malignancy of bladder carcinoma by triggering cell migration and EMT through the ROS/Src/FAK signaling pathway
Cell Biology and Toxicology (2020)
-
UHRF1 depletion and HDAC inhibition reactivate epigenetically silenced genes in colorectal cancer cells
Clinical Epigenetics (2019)