Abstract
Monthly intravenous pegylated liposomal doxorubicin (PLD) 50 mg m−2, although well tolerated, showed almost no activity in this phase II study of 16 patients with advanced hepatocellular carcinoma with a response rate of 0%, stable disease 19%, median time to progression of 2.4 months, 1-year survival of 25% and median survival of 6.5 months.
Similar content being viewed by others
Main
Surgery, currently the only treatment offering long-term cure, is possible in a minority of patients with hepatocellular carcinoma (HCC) (Llovet et al, 2003). In selected patients with unresectable, liver-only, disease hepatic embolisation or chemoembolisation confers a survival advantage compared with conservative management (Llovet et al, 2002; Lo et al, 2002). However, in the recent meta-analysis, this effect may be limited to chemoembolisation but not embolisation (Llovet and Bruix, 2003). Chemotherapy for inoperable and extrahepatic disease is relatively ineffective; the current ‘standard’, doxorubicin, has a response rate of 16% (range 0–35%) in a review of eight trials including 475 evaluable patients (Engstrom et al, 1993). It is associated with a small survival advantage over supportive care alone in a randomised study of 106 chemotherapy-naïve patients at the expense of significant toxicity (mucositis, alopecia, myelosuppression and cardiotoxicity) (Lai et al, 1988).
Liposomes, capable of encapsulating anticancer agents without chemical modulation, accumulate preferentially in the reticuloendothelial system (Weinstein, 1984). This uptake may be evaded by ‘stealth’ liposomes (formed by altering the liposome lipid composition), which preferentially exit the circulation via leaky capillaries and are predicted to accumulate in tumours exhibiting extensive neo-vascularisation (such as HCC) leading to higher concentrations and enhanced antitumour activity (Wu et al, 1993). Pegylated liposomal doxorubicin (PLD), an intravenous preparation of doxorubicin hydrochloride encapsulated in long-acting pegylated ‘stealth’ liposomes, can avoid rapid hepatic uptake resulting in a prolonged circulation time. Compared to conventional doxorubicin, intratumoural doxorubicin levels in tumour-bearing mice were substantially higher when using PLD. Moreover, enhanced cytotoxicity of an HCC cell line has been demonstrated using ‘stealth’ liposomes compared to conventional doxorubicin (Shimizu et al, 1996).
Dose-limiting toxicities of PLD include reversible neutropaenia, stomatitis and plantar-palmar erythrodysaesthesia. Alopecia and emesis are infrequent (Uziely et al, 1995). A phase I study in 33 patients with advanced HCC determined neutropaenia as the dose-limiting toxicity at 60 mg m−2 and recommended 50 mg m−2 every 28 days as the phase II dosing regimen (Schering Plough – data on file). Endomyocardial biopsies have shown PLD to have a superior cardiac safety profile compared to nonliposomal doxorubicin (Berry et al, 1998).
Materials and methods
Patient selection
An open-label, phase II study was performed. Chemotherapy-naïve patients (including chemotherapy as part of chemoembolisation procedures) with histologically proven HCC, aged ⩾18 years, with measurable disease by CT/MRI scan (WHO criteria), WHO performance score (PS) of ⩽2, life expectancy ⩾3 months, left ventricular ejection fraction (LVEF) ⩾50% (by MUGA or echocardiography), haemoglobin >9 g dl−1, white blood cells ⩾3.0 × 109 l−1, neutrophils ⩾1.5 × 109 l−1 and platelets ⩾100 000 mm−3, serum creatinine <1.5 × upper limit of normal (ULN), bilirubin <1.5 × ULN and AST/ALT <2 × ULN (unless related to primary disease when value <5 × ULN) were eligible. Patients with New York Heart Association⩾Class II cardiac disease, patients who were pregnant, lactating or were unwilling to use contraception during the study were excluded. The appropriate Local Research Ethics Committees at each institution approved the study and all patients gave written informed consent prior to study entry.
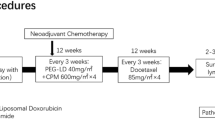
Treatment
Patients received PLD (Caelyx®/Doxil®, Schering-Plough headquarters, Kenilworth, NJ, USA) 50 mg m−2 in 250–500 ml of 5% dextrose i.v. over 1 h on day 1 of each 28-day cycle. Retreatment occurred upon recovery of platelets to ⩾75 000 mm−3, ANC to ⩾1.5 × 109 l−1 and skin toxicity or stomatitis to grade ⩽1. A 25% dose reduction was permitted for delayed recovery from toxicity or grade ⩾2 toxicity. Patients were withdrawn from the study for a deferral of a treatment cycle (for toxicity) by more than 2 weeks.
Evaluation
Tumour assessments (CT/MRI scan) and cardiac assessments (ECG/LVEF) were made at baseline and after cycles 3, 6 and 9. Patients received PLD until disease progression, unacceptable toxicity, patient choice or physician's discretion. Toxicity (NCI-Common Toxicity Criteria, version 2.0), vital signs and serum biochemistry (including serum AFP) were assessed at baseline and at every cycle with weekly blood counts during the study period. All patients were followed up for survival data.
Results
A total of 16 patients (see Table 1 for patient characteristics) received a total of 47 cycles (median 3, range 1–9) at two institutions (Christie Hospital, Manchester, UK (n=13) and University College Hospital, London, UK (n=3)) between November 1998 and April 2002.
Toxicity
Treatment was well tolerated with most toxicities reported at grade 1. Grade 3–4 toxicity included leucopaenia, neutropaenia, nausea/vomiting and lethargy in 12, 12, 6 and 6% of patients, respectively (and 4, 6, 2 and 2% of cycles, respectively). Dose delays were required on three occasions and a total of three dose reductions were made. One patient with persistent grade 4 neutropaenia was withdrawn from treatment. No cardiac toxicity was observed. Hepatic toxicity was mostly grade 1; grade 2 hyperbilirubinaemia was seen in 27% of patients (9% of cycles) and elevated serum alkaline phosphatase in 9% of patients (3% of cycles). No grade 2 transaminitis or grade 3–4 hepatotoxicity was documented (Table 2 ).
Response and survival
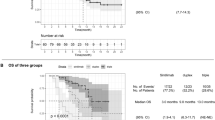
No responses were seen in the first 16 patients and the study was closed to accrual as the minimal threshold of activity had not been reached according to the Simon one sample, two-stage design (Simon, 1989). Three patients (19%) had stable disease after three cycles, with disease progression in the remaining patients (including the three patients with FLHCC). One of the three patients with stable disease had ongoing stable disease after six and nine cycles of treatment. The median time to disease progression in all patients was 2.4 months with 1-year and 2-year survival rates of 25 and 12.5%, respectively. The median survival of all patients was 6.5 months. As expected, patients with FLHCC had a longer median survival (20.5 months) than patients with standard HCC histology (4.3 months).
Second-line chemotherapy was administered to six patients (38%) (gemcitabine alone (n=3) or with cisplatin (n=3)). Two patients receiving cisplatin–gemcitabine achieved disease stabilisation having previously progressed, the remainder had disease progression. One patient with FLHCC achieved a sustained partial response with continuous-infusion 5-FU and interferon having failed PLD followed by cisplatin–gemcitabine and remains alive at 54 months.
Two patients (13%) with disease confined to the liver were deemed suitable for chemoembolisation at first assessment. The choice was made to proceed with PLD in the first instance (prior chemoembolisation would have deemed them ineligible). Both progressed after three cycles of PLD and then underwent chemoembolisation (achieving survivals of 16 and 25 months, respectively). Five patients (31%) received palliative hormone therapy.
Discussion
Doxorubicin, with modest activity, is a toxic agent and patients with advanced HCC are frequently unwell due to their underlying tumour and hepatic dysfunction. There was an expectation that its efficacy could be maintained (or even enhanced) with the better tolerated PLD formulation (Uziely et al, 1995).
A number of studies contemporary to ours (see Table 3 ) have shown, at best, response rates of 10–17% (Ruff et al, 2001; Schmidinger et al, 2001; Hong and Tseng, 2003). Two studies, as in our case, revealed no responses: in the first, no objective responses were seen in 16 patients receiving 30–40 mg m−2 three-weekly. With a median survival of 20 weeks, the authors concluded that PLD was ineffective (Halm et al, 2000). Miller et al (2002) reached the same conclusion with a 0% response rate in a mixed study of 10 HCC (and eight cholangiocarcinoma) patients. Based on a median survival of 1-year, Schmidinger et al (2001) concluded that PLD warranted further studies. However, Ruff et al (2001) who demonstrated a 17% response rate achieved a median survival of only 5.3 months. The difficulty in relying on response rate as a marker of activity was further illustrated by Hong and Tseng (2003): despite 10% of patients responding to treatment and a further 33% achieving stable disease, the median survival was only 3 months.
A favourable toxicity profile has been consistent across all the HCC studies (Halm et al, 2000; Ruff et al, 2001; Schmidinger et al, 2001; Miller et al, 2002; Hong and Tseng, 2003). We found few grade 3–4 toxicities and notably none involving palmar-plantar erythrodysaesthesia, a dose-limiting toxicity seen in early studies along with stomatitis and neutropaenia (Muggia et al, 1997; Ranson et al, 1997). Cardiac toxicity was not seen and dose reductions or dose delays due to toxicity were uncommon. Enhanced activity of PLD was postulated by increased leakage from capillaries in vascular tumours once the drug had evaded rapid hepatic uptake. This reduced uptake may, however, also be responsible for the lack of hepatotoxicity and, ultimately, efficacy.
Despite the ability to deliver doxorubicin more safely to patients, PLD has almost no activity in advanced HCC. This reflects the relative insensitivity of HCC to chemotherapy agents and success may come from alternative treatment modalities aimed at better targeting of the underlying pathological processes involved in HCC carcinogenesis.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Berry G, Billingham M, Alderman E, Richardson P, Torti F, Lum B, Patek A, Martin FJ (1998) The use of cardiac biopsy to demonstrate reduced cardiotoxicity in AIDS Kaposi's sarcoma patients treated with pegylated liposomal doxorubicin. Ann Oncol 9: 711–716
Engstrom PF, Mc Glynn K, Weese JL (1993) Primary neoplasms of the liver. In Cancer Medicine Holland JF, Frei E (eds) pp. 1430–1441. London: Lea and Febiger
Halm U, Etzrodt G, Schiefke I, Schmidt F, Witzigmann H, Mossner J, Berr F (2000) A phase II study of pegylated liposomal doxorubicin for treatment of advanced hepatocellular carcinoma. Ann Oncol 11: 113–114
Hong RL, Tseng YL (2003) A phase II and pharmacokinetic study of pegylated liposomal doxorubicin in patients with advanced hepatocellular carcinoma. Cancer Chemother Pharmacol 51: 433–438
Lai CL, Wu PC, Chan GC, Lok AS, Lin HJ (1988) Doxorubicin versus no antitumor therapy in inoperable hepatocellular carcinoma. A prospective randomized trial. Cancer 62: 479–483
Llovet JM, Bruix J (2003) Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37: 429–442
Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362: 1907–1917
Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart, Sola R, Rodes J, Bruix J (2002) Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359: 1734–1739
Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, Fan ST, Wong J (2002) Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35: 1164–1171
Miller RL, Bowen KE, Chun HG (2002) A phase II study of liposomal doxorubicin (LD, Doxil) in patients with advanced hepatocellular carcinoma (HCC) or cholangiocarcinoma (CC). Proc Am Soc Clin Oncol 21: (abstract 2324)
Muggia FM, Hainsworth JD, Jeffers S, Miller P, Groshen S, Tan M, Roman L, Uziely B, Muderspach L, Garcia A, Burnett A, Greco FA, Morrow CP, Paradiso LJ, Liang LJ (1997) Phase II study of liposomal doxorubicin in refractory ovarian cancer: antitumor activity and toxicity modification by liposomal encapsulation. J Clin Oncol 15: 987–993
Ranson MR, Carmichael J, O’Byrne K, Stewart S, Smith D, Howell A (1997) Treatment of advanced breast cancer with sterically stabilized liposomal doxorubicin: results of a multicenter phase II trial. J Clin Oncol 15: 3185–3191
Ruff P, Moodley SD, Rapoport DA, Vorobiof DA, Maart K, Chasen MR (2001) Long-term follow-up of pegylated liposomal doxorubicin (Caelyx): a well tolerated and effective agent in advanced hepatocellular carcinoma (HCC). Proc Am Soc Clin Oncol 20: (abstract 667)
Schmidinger M, Wenzel C, Locker GJ, Muehlbacher F, Steininger R, Gnant M, Crevenna R, Budinsky AC (2001) Pilot study with pegylated liposomal doxorubicin for advanced or unresectable hepatocellular carcinoma. Br J Cancer 85: 1850–1852
Shimizu H, Kumai K, Uyama I, Shibata S, Tagawa T, Nagaike K, Yasuda T, Kitajima M, Tadakuma T (1996) Improvement of pharmacokinetics and antitumor activity against human hepatoma cell line by using adriamycin-entrapped stealth liposomes. J Surg Oncol 62: 186–193
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10: 1–10
Uziely B, Jeffers S, Isacson R, Kutsch K, Wei-Tsao D, Yehoshua Z, Libson E, Muggia FM, Gabizon A (1995) Liposomal doxorubicin: antitumor activity and unique toxicities during two complementary phase I studies. J Clin Oncol 13: 1777–1785
Weinstein JN (1984) Liposomes as drug carriers in cancer therapy. Cancer Treat Rep 68: 127–135
Wu NZ, Da D, Rudoll TL, Needham D, Whorton AR, Dewhirst MW (1993) Increased microvascular permeability contributes to preferential accumulation of stealth liposomes in tumor tissue. Cancer Res 53: 3765–3770
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Valle, J., Dangoor, A., Beech, J. et al. Treatment of inoperable hepatocellular carcinoma with pegylated liposomal doxorubicin (PLD): results of a phase II study. Br J Cancer 92, 628–630 (2005). https://doi.org/10.1038/sj.bjc.6602394
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602394
Keywords
This article is cited by
-
Radiofrequency ablation of small hepatocellular carcinoma with intravenous pegylated liposomal doxorubicin
Hepatology International (2011)
-
Management of hepatocellular cancer
Current Treatment Options in Oncology (2005)