Key Points
-
Describes current clinical practice for managing periodontal diseases in primary care in Scotland.
-
Highlights the variation in periodontal treatments provided by practitioners.
-
Provides an overview of the challenges faced by practitioners when managing patients with periodontal conditions.
-
Illustrates how practitioner-led research can inform the scope of a evidence-based guidance publication.
Abstract
Aims To understand current practice and the beliefs of dentists and hygienists towards factors which may influence the management of patients with periodontal diseases in primary dental care in Scotland. To inform the scope of a guidance publication and the future development of diagnostic analyses tools.
Methods A qualitative approach of semi-structured telephone interviews with a randomly selected sample of dentists and hygienists was used. Interviews continued until saturation was reached and were audio-recorded and transcribed verbatim. The data were analysed using the method of framework analysis. To increase the participation of hygienists the topic guide was adapted into a self-reporting questionnaire and posted to all hygienists in Scotland.
Results Eighteen dentists and three hygienists were interviewed. Key themes identified were extent of control over working environment, capabilities to treat appropriately and changing patients' oral hygiene behaviour. Factors which facilitated the management of patients with periodontal diseases were 'access to a hygienist' and 'beliefs about capabilities', while 'routine and habit', 'motivation of patients' and 'time and money' were perceived as barriers. Some evidence of variation in treatment provision and of varying levels of confidence among practitioners about treating more advanced periodontal conditions was identified. Two hundred and thirty-seven hygienists returned the postal questionnaire. Agreement was found with the views of the interviewed hygienists on beliefs about capabilities and routine record-keeping.
Conclusion To improve the periodontal health of patients requires consideration of both extrinsic and intrinsic factors present in primary dental care. Practitioners would find having guidance on managing patients with basic periodontal examinations of three and four, referral criteria to secondary care, record-keeping and techniques to change patients' oral hygiene behaviour particularly useful. Applying the evaluative framework pre-publication indicated where knowledge translation interventions may be required in the future.
Similar content being viewed by others
Introduction
Epidemiological evidence suggests a high prevalence of periodontal disease in the general population in the UK. In the 2009 Adult Dental Health survey,1 45% of dentate adults in England, Wales and Northern Ireland had evidence of pocketing exceeding 4 mm, which is indicative of current periodontal disease, and 54% had gingival bleeding, which has been acknowledged as a risk factor for periodontitis.2 In the 1998 UK Adult Dental Health Survey,3 the most recent survey to include Scotland, it was estimated that 54% of the dentate adult population had pocketing greater than 3.5 mm. The results were broadly similar when comparing across countries in the survey. While these findings for Scotland are over ten years old, there is no recent evidence to suggest that the periodontal health of the population in Scotland differs from other areas of the UK.
There is also evidence from both the UK and other countries of variation in the diagnosis and treatment of periodontal diseases by dentists in primary dental care.4,5,6 Explanations of variation in practice include a lack of knowledge and skills, as reported by an Australian study that adopted a day log approach,4 and a lack of interest in the aetiology of periodontal diseases, as determined from a survey of dentists in Northern Ireland.5 In England, Sharpe et al.6 reported that treatment was heavily influenced by the NHS remuneration system, resulting in a high number of referrals to specialists.
In 2012–2013, of the 1.99 million NHS items of service claims7 for adult periodontal treatments in Scotland, approximately 93% were for 'scaling, polishing and simple periodontal treatment, including oral hygiene instruction' (Statement of Dental Remuneration [SDR] item 10a).8 Fewer than 7% of claims were for 'treatment of periodontal disease requiring more than one visit, including oral hygiene instruction, scaling, polishing and marginal correction of fillings' (item 10b).8 For 'non-surgical treatment of chronic periodontal disease, including oral hygiene instruction' (item 10c),8 the quantity claimed equated to less than 1% of the total.
Available evidence suggests an apparent reluctance to treat advanced periodontal disease in primary care. Recognising the need for accessible guidance in this area, the Scottish Dental Clinical Effectiveness Programme (SDCEP) initiated the development of a guidance document, Prevention and treatment of periodontal diseases in primary care, in 2012. Operating within NHS Education for Scotland (NES), SDCEP is a national guidance development initiative for dentistry. SDCEP's primary aim is to support dental professionals to deliver the best possible care for their patients by providing user-friendly, evidence-based guidance in priority areas for dentistry.9
It is well documented that the translation of best practice recommendations into clinical practice may not simply result from the passive publication of evidence-based guidance.10,11,12 To bridge the gap between dissemination of guidance recommendations and implementation into practice, NES established the Translation Research in a Dental Setting (TRiaDS) initiative in 2008. TRiaDS is a multi-disciplinary research collaboration that has developed a theoretically driven evaluative framework to support the translation of SDCEP guidance recommendations into practice.13 This study applies the TRiaDS evaluative framework to explore practitioners' current practice and beliefs when diagnosing and managing patients with periodontal diseases in primary dental care in Scotland.
Materials and methods
Design, sample and setting
A qualitative approach comprising semi-structured telephone interviews with dentists and dental hygienists was used. Random samples of 50 dentists and 40 hygienists practising within NHS primary dental care in Scotland were invited to participate in a telephone interview via a letter which outlined the aims of the study. All non-responders received a reminder letter after two weeks. If required, a follow-up telephone call was made to dentists only as the telephone contact details of hygienists were not available. Participants included Rapid Evaluation Practitioners (REPs), a group of dentists who contribute to the Scottish Dental Practice Based Research Network14 (SDPBRN).
Semi-structured interviews
The telephone interviews were conducted using a topic guide focusing on (1) current management of patients with periodontal diseases, (2) prevalence of periodontal diseases among their patients, and (3) practitioners' beliefs towards management of periodontal diseases. A conversational style of interview was employed to discuss the topics with opportunities given for the participants to ask questions. Questions in the topic guide were informed by a literature search and discussion with clinical colleagues. Based on these topics, the researcher conducting the interviews used additional prompts to help with further probing for views. The topic guide was dentist-specific or hygienist-specific and the sequence of questions was flexible, in that topics could be discussed as raised by the interviewee rather than in a rigid order. Interviewees were encouraged to discuss topics which they felt were most meaningful or salient to them. The interviews were audio recorded and transcribed verbatim before the analysis being conducted. The duration of the interviews ranged from 12–43 minutes (mean: 22 minutes). One interview was not transcribed due to a recording equipment malfunction, but as notes were taken during the interview it was included in the study.
Analysis
The qualitative method used to analyse the data was framework analysis developed by Ritchie et al.15 which is described as a matrix based method using a thematic framework to organise and classify data according to key themes, concepts and emerging themes. Some themes may relate directly to the questions asked and others may emerge from issues raised by participants. A coding index, developed from reading the transcripts, was used to identify themes from the text. A sorting process collated the coded text from within and across all interviews under each theme. QSR International's NVivo 9 software was used to assist in the data management of the transcripts.
The reliability of the theme identification was checked within the research team to ensure coding consistency for subsequent analysis; team members are experienced dental health service researchers. After 18 interviews with dentists, it was judged that saturation had been achieved as no new themes had emerged from the previous three interviews.16 Consequently, further recruitment of dentists was discontinued.
Recruitment of hygienists was hampered by the lack of telephone contact details and therefore relied on their response to the first and reminder invitational letters. With only three hygienists agreeing to be interviewed, the topic guide was adapted into a self-reporting questionnaire using both a 7-point Likert agreement scale (1 = strongly disagree, 7 = strongly agree) and a 4-point categorical compliance scale (1 = never, 4 = always). The questionnaire was posted to all of the 499 hygienists registered in Scotland excluding the three interviewees.
Ethical considerations
Under the Governance Arrangements for Research Ethics Committees17 (GAfREC), no ethical review is required for NHS staff recruited as research participants by virtue of their professional role.
Results
Eighteen dentists (including nine REPs) and three hygienists participated in the telephone interviews. One dentist responded to the first invitational letter with the remainder receiving a reminder. Follow-up telephone calls were made until a sufficient number of dentists were recruited. Seven dentists declined from the outset, stating that they were 'too busy', three were no longer at the address provided and two dentists who agreed to participate later declined because of time restrictions. The participation of hygienists was low (3/40 invited). As follow-up calls were not possible for hygienists, no information is available about their reasons for declining to participate in the study. Thirteen of the dentists were male; all three hygienists were female. The level of clinical experience was three to 37 years (mean = 18 years).
Hygienist questionnaire
After the first mailing and two reminders, a total of 238 questionnaires were returned including 44 which were 'gone away' (n = 22) or declining to participate (n = 22). The response rate was 41% (194/477). All respondents were female with a clinical experience mean of 21 years.
Current management of patients with periodontal diseases
All dentists assessed the periodontal status of their patients at routine examinations. Five dentists stated they used the Basic Periodontal Examination (BPE) and five stated they used the Community Periodontal Index for Treatment Needs (CPITN), either on its own or in combination with the BPE. All three interviewed hygienists stated that they used the BPE and two of the hygienists stated that they would always repeat the examination in order to confirm the dentist's assessment. In the questionnaire, the hygienists (DHqus) reported that the BPE was used mostly in their practice (61%). Five percent of DHqus stated that the practice used the CPITN only or a combination with the BPE (7%). These responses may reflect that some practitioners continue to use CPITN to describe the BPE screening tool and a belief among a few that the CPITN and BPE are two different indices. The diverse responses may reflect various means of describing periodontal screening within the profession.
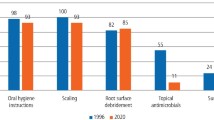
All practitioners were asked to describe the different types of treatments they would provide for patients with a BPE score of 1, 2, 3 or 4. Table 1 shows the variation of treatments provided according to patients' BPE score as reported by dentists and interviewed hygienists. The percent of DHqus reporting that patients with a BPE of 3 or 4 would receive a 10b and 10c (SDR items),8 as per the treatment plan was for a BPE of 3–57% and 18% and for a BPE of 4–35% and 44% respectively. This is illustrated in Figure 1.
The percent of DHqus reporting patients receiving a 10b and 10c (SDR items) as per the BPE score in the treatment plan8
Referrals to secondary care were rare and primarily led by the periodontal condition of the patient, namely, treatment did not achieve the expected results, a new patient with BPE score of 3 or 4, or if more advanced surgical treatment was considered necessary. Non-clinical factors that negatively influenced secondary care referrals were long waiting times to obtain an appointment (one dentist stated a waiting time of up to 42 weeks), travelling distance to the dental hospital, time and cost implications to the patient and the patient's motivation to attend. One dentist reported performing periodontal surgery, with the remainder stating that they had insufficient training or had no desire to do so.
Prevalence of periodontal diseases among their patients
All practitioners saw patients with varying levels of periodontal disease. The proportion of patients in each BPE group differed across practitioners, for example, when asked how many of their last ten patients were assessed with a BPE of 3, responses ranged between one and five.
Practitioners' beliefs and attitudes towards managing periodontal disease
The key themes were (1) the extent of control over their working environment (2) capabilities to treat appropriately and (3) improving patients' oral hygiene behaviour. Both dentists and hygienists stated that changes to some or all of these key themes were fundamental for improving the management of patients with periodontal diseases. Each of the key themes consists of one or more sub-theme which acts as either a facilitator or a barrier to managing patients with periodontal diseases.
Control over working environment
Access to dental hygienists
Hygienists felt that it is their responsibility to treat patients with periodontal diseases, with one commenting 'dentists know that perio treatment is needed, but leave the fine detail up to us'. All DHqus confirmed their professional responsibility was to treat periodontal diseases and 97% rated 'strongly agree' that providing periodontal treatment is an opportunity to determine the appropriate care.
All dentists with access to a hygienist stated that it was the primary role of the hygienist to treat patients with periodontal diseases and believed that hygienists' were better skilled and trained to perform this role. One dentist said 'hygienists are key' and added 'dentists get fed up doing it. Possibly hygienists do too'. Other dentists commented 'my hygienist is much better at it than me', 'hygienists are specially trained' and 'I let the hygienist make all the decisions herself'.
Dentists with a hygienist often had a more positive attitude towards treating patients with periodontal diseases, as they could refer these patients to the hygienist for treatment. They reported that this allowed them to treat patients they considered to be more 'clinically challenging'.
Routine and habit
All practitioners interviewed considered the treatment of periodontal diseases to be an accepted part of their daily routine. However, its considerable prevalence is not always acknowledged as something that needs to be dealt with, and at times not always discussed within dentistry. One dentist expressed this by saying 'It is the one big area in dentistry, I think is the 'elephant in the room' that no-one will talk about.'
Some examples of the phrases used to describe periodontal diseases were 'confusing', 'not exciting', 'nothing changes' and 'frustrating'; this illustrates the dentists' attitudes towards these diseases. These descriptions are underpinned by a belief that the management of periodontal diseases requires long-term repetitive treatments and that a positive outcome is often not always attainable, especially when patients are not motivated or able to maintain good oral hygiene.
As part of their daily routine, all three of the hygienists expressed concerns about the level of information provided in treatment plans for both the diagnosis and the treatment required, with one describing it as 'brief and basic'. The DHqus agreed with these comments with only 24% rating a diagnosis is 'always' written in the treatment plan.
Time and money
A salient theme in the narrative data was the relationship between time and remuneration. Both dentists and hygienists repeatedly mentioned that the Statement of Dental Remuneration (SDR) did not adequately reimburse for the actual time needed to give appropriate treatments to patients with periodontal diseases. One comment summarised the views of many.
'You have set fees and you have to cover a lot in an examination and a visit to the hygienist...you have a limited length of time, you know, your check-up – ten minutes and hygienist appointment – 20 minutes; there is only so much you can cover.'
The time available was highlighted also by the DHqu's who 'strongly agree' that it was limited for assessing patients (55%), giving oral hygiene instructions (48%) and providing treatments (54%).
Capabilities to treat appropriately
Despite the management of periodontal diseases being an everyday occurrence, some concerns were raised regarding appropriate treatment and skill requirements. One dentist expressed the view 'I think people are frightened of perio, sometimes of what they can and cannot do'. This was supported by another comment from one dentist who experienced challenges with more chronic periodontal disease and who stated 'it's hard for [BPE] 3's and 4's'.
These concerns about what treatment is appropriate were noted to be more relevant among the younger dentists. One young dentist expressed low confidence about knowing when to refer patients to secondary care. The same dentist also demonstrated some reluctance to refer to secondary care by saying 'I don't want to be seen to be sending referrals that are seen as inappropriate and annoying people in the service'.
In contrast, the three hygienists interviewed were confident about providing treatment and perceived referrals to secondary care as being unnecessary as 'dental hospitals are inundated with patients, they are not interested in maintenance, and they can't do more than I can do'. The DHqus were 100% confident in treating patients with periodontal diseases and scored the number of patients being 'rarely' referred to secondary care as 75% for BPE 3's and 53% for BPE 4's.
Changing patients' oral hygiene behaviour
All participants believed that one of the key factors which contributed to successful treatment of periodontal diseases was the involvement of a motivated patient. In instances where the patient was not motivated to maintain good oral hygiene, treatment was seen as 'futile' and 'frustrating'.
Getting the oral health message across to patients was seen as a challenge by some dentists. Often the dentists with access to a hygienist felt that the hygienist was better trained to give oral hygiene instruction to patients and therefore delegated this responsibility to them. The hygienists confirmed this view by saying that their training was more suited to giving the appropriate oral hygiene instruction. Eighty-eight percent of DHqus reported dentists 'always' expect hygienists to give oral hygiene instructions to patients, but 64% of DHqus thought that dentists should also be doing it.
Scope of periodontal guidance
Through the interviews and questionnaires the areas identified as requiring particular attention in the periodontal guidance were (1) managing patients with BPE's of 3 and 4; (2) referral criteria to secondary care; (3) appropriate diagnosis and treatment plans and (4) techniques to motivate patients to improve oral hygiene.
Discussion
This study explores practitioners' current practice when diagnosing and managing patients with periodontal diseases in primary dental care in Scotland. The results show variation in the management of periodontal diseases, including decisions about treatment provision based on BPE scores and criteria for secondary referrals. Emerging from the thematic analysis of the narrative data were the most frequently mentioned beliefs about practitioners' current practice and how these influence their management of patients with periodontal diseases. The interviews identified three key themes (1) extent of control over their working environment (2) capabilities to treat appropriately and (3) changing patients' oral hygiene behaviour. This extrinsic factor of control was seen as either a barrier or a facilitator depending on the participant's perceived capacity to change patients' behaviour to maintain good oral hygiene and also if a hygienist was present in the practice. Both dentists and hygienists acknowledged that the balance of time and fees was fundamental to best practice but felt the remuneration system under the NHS in Scotland was time constraining and so acted as a barrier.
One of the facilitating factors was the level of confidence with which some dentists individually reported beliefs about capabilities to diagnose. However, some concluded that there is less confidence across the profession to treat more advanced periodontal diseases. This is consistent with other qualitative studies which found high proportions of dentists were confident in their ability to diagnose periodontal disease but less so in treating it.18,19,20
Some of the barriers identified, such as motivation of patients and time and money, are also reflected in previous studies,6,21 with dentists reporting the treatment provided was significantly influenced by the NHS remuneration system.22 Habit and routine was highlighted as a barrier in a series of audits of a system23 designed to assist dentists by giving them prompts to conduct a periodontal examination. In the first audit 62% of patients' records included a BPE score and this increased to 80% at the second audit. Interestingly, the outcome of breaking the dentists' habit and routine by introducing a simple prompt was sufficient to bring about changes in dentists' behaviours regarding carrying out the BPE.
In this study, an overall impression emerged that dentists view treatment of periodontal disease differently from hygienists. More positive views came from hygienists and those dentists who have access to a hygienist. Dentists without a hygienist in their practice just accepted having to treat periodontal diseases; some found it burdensome and all voiced that when managing periodontal diseases the main issues were time, remuneration and the motivation of patients. Previous findings suggest that practices employing a hygienist are more periodontal-orientated, with hygienists acting to complement the services of dentists in the provision of periodontal treatment, rather than as a substitute for the dentist.24
In addition to the information gathered by the SDCEP as part of the scoping process, this study was able to provide a valuable insight for the SDCEP periodontal guidance development working group. This practitioner-led research identified managing patients with BPE's of 3 and 4, referral criteria to secondary care, appropriate diagnosis and treatment plans and techniques to improve patient's oral hygiene behaviour as areas of concern and guidance on these topics would be particularly useful.
Conclusion
The extent of control over the working environment, capability to treat appropriately and capacity to change patient behaviour regarding their oral hygiene were perceived to be paramount in managing periodontal diseases in primary care. There is some evidence to suggest that dentists and hygienists perceive there to be varying levels of confidence within the dental profession when treating patients with more advance periodontal conditions and some variation in the treatment provided for periodontal conditions. The topics of particular concern to practitioners to be addressed by the guidance were identified by the study. As a consequence of this insight, oral hygiene TIPPS, a behavioural change strategy which shows patients how to achieve effective plaque removal was included in the SDCEP guidance published in 2014.25 The use of the evaluative framework has elucidated the need for a guidance document and, more importantly from a knowledge translation perspective, informed TRiaDS on the future research and possible training required to support evidence-based clinical management of periodontal diseases in primary dental care.
Commentary
This interesting paper was written to delve into the attitudes of dentists and hygienist/therapists toward periodontal therapy in general practice and has inadvertently exposed the current unsatisfactory state of affairs.
Fifty dentists and 40 hygienists in Scotland were invited, by letter and follow-up phone calls, to participate in telephone interviews. The interviews were conversational and semi-structured so the results are anecdotal rather than scientific; however, after 18 interviews with dentists no new themes had emerged so no further dentists were recruited. Depressingly, the response was very poor. Only 36% of the dentists and 8% of the hygienists responded and many of those contacted by phone considered themselves to be too busy to participate in this research. What does this say about the commitment and enthusiasm of today's dental practitioners?
When asked about their assessment of periodontal diseases, 55% of dentists said they use the BPE/CPITN. Some said they used both! What are the rest using? Forty-five percent in this admittedly small sample are using no periodontal index or data recording whatsoever. Furthermore, when asked about treatment, only 44% of responders would provide a three-visit periodontal treatment programme (10c) for BPE code four cases. Referrals to secondary care were rare due to long waiting times, time and cost of travelling, and lack of patient motivation.
The paper goes on to consider possible reasons for these deficiencies, including the lack of confidence among younger dentists about when and which patients to refer. Many dentists therefore delegate – or abrogate – responsibility for periodontal management to a hygienist. This is perhaps a sign of changing times; however, it also suggests a deficiency in basic training of periodontics. Poor levels of remuneration for periodontal treatment were also highlighted, not for the first time, as demotivating factors for dentists.
The paper shows that hygienists have a much more positive attitude to periodontal therapy than dentists, no doubt reflecting the increasing confidence engendered by direct access. It is to be hoped that this will lead to improved periodontal therapy in the future, reduction in the high number of periodontal negligence claims, and better periodontal health for our patients.
Philip R. Greene Specialist in periodontics; Dental expert witness The Malt House Dental Centre
Author questions and answers
1. Why did you undertake this research?
This research was conducted as part of the Translation Research in a Dental Setting (TRiaDS) programme, a research collaboration embedded within the Scottish Dental Clinical Effectiveness Programme (SDCEP) guidance development process. The remit was to inform the scope of SDCEP's guidance document Prevention and Treatment of Periodontal Diseases in Primary Care which was published in June 2014. This study enabled us to collect information on how patients with periodontal conditions are assessed and treated in primary care in Scotland. Also, the study assisted in building a picture about the potential facilitators and barriers to implementing evidence-based clinical practice when managing periodontal diseases. This gave an invaluable insight to the SDCEP periodontal guidance development working group on where variations in clinical practice occurred.
2. What would you like to do next in this area to follow on from this work?
The Translation Research in a Dental Setting (TRiaDS) programme framework will be applied to the implementation of SDCEP's guidance document Prevention and treatment of periodontal diseases in primary care. We will build on the work in this study to identify whether a gap exists between current clinical practice and the guidance recommendations. Future work may include designing a theoretically-driven intervention to help practitioners translate the evidence-based guidance into routine clinical practice.
References
Health and Social Care Information Centre. Disease and related disorders - a report from the Adult Dental Health Survey 2009. Leeds: The Health and Social Care Information Centre, 2011.
Kinane D F, Attström R, on behalf of the European Workshop in Periodontology group B. Advances in the pathogenesis of periodontitis. J Clin Periodontol 2005; 32: 130–131.
National Statistics for Department of Health. Adult Dental Health Survey: oral health in the United Kingdom 1998. London: Office for National Statistics for Department of Health, 2000.
Spencer A J, Lewis J M . The provision of periodontal services in general dental practice in Australia. Community Dent Health 1989; 6: 337–347.
Linden G J . Variation in periodontal referral by general dental practitioners. J Clin Periodontol 1998; 25: 655–661.
Sharpe G, Durham J A, Preshaw P M . Attitudes regarding specialist referrals in periodontics. Br Dent J 2007; 202: 218–219.
Information Services Division Scotland. Dental statistics – NHS fees and treatments. Edinburgh: NHS National Services, 2011.
Scottish Executive Health Department. Statement of dental remuneration. Edinburgh: Scottish Executive, 2006.
Scottish Dental Clinical Effectiveness Programme (SDCEP). Online information available at www.sdcep.org.uk (accessed March 2015).
Seddon M E, Marshall M N, Campbell S M, Roland M O . Systematic review of studies of quality of clinical care in general practice in the UK, Australia and New Zealand. Qual Health Care 2001; 10: 152–158.
Grimshaw J M, Thomas R E, MacLennan G et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 2004; 8: 1–84.
Grol R . Improving the quality of medical care. Building bridges among professional pride, payer profit, and patient satisfaction. JAMA 2001; 286: 2578–2585.
Clarkson J, Ramsay C, Eccles M et al. The translation research in a dental setting (TRiaDS) programme protocol. Implem Sci 2010; 5: 57–67.
Scottish Dental Practice Based Network (SDPBRN). Online information available at www.sdpbrn.org.uk (accessed March 2015).
Ritchie J, Spencer L . Qualitative data analysis for applied policy research. In Bryman A, Burgess R G (eds) Analysing qualitative data. pp 172–194. London: Routledge, 1994.
Francis J J, Johnston M, Robertson C et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies, Psychol Health 2010; 25: 1229–1245.
Department of Health. Governance arrangements for research ethics committees: a harmonised edition. 2012. Online information available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213753/dh_133993.pdf (accessed March 2015).
Darby I B, Angkasa F, Duong C et al. Factors influencing the diagnosis and treatment of periodontal disease by dental practitioners in Victoria. Aust Dent J 2005; 50: 37–41.
Ghiabi E, Weerasinghe S . The periodontal examination profile of general dentists in Nova Scotia, Canada. J Periodontol 2011; 82: 33–40.
Chestnutt I G, Kinane D F . Factors influencing the diagnosis and management of periodontal disease by general dental practitioners. Br Dent J 1997; 183: 319–24.
Fardal O . Interviews and assessments of returning non-compliant periodontal maintenance patients. J Clin Periodontol 2006; 33: 216–220.
Chapple I L C . Management of chronic periodontal diseases within the NHS. Br Dent J 2004; 196: 505.
Snoad R . Description of a system designed to assist primary dental care clinicians in decision-making with regard to specialist periodontal referrals and report of two clinical audits using the system. Prim Dent Care 2005; 12: 135–141.
Brown L F, Spencer A J, Keily P A . Service mix in general dental practices employing and not employing dental hygienists. J Clin Periodontol 1994; 21: 684–689.
Scottish Dental Clinical Effectiveness Programme (SDCEP). Prevention and treatment of periodontal diseases in primary care. 2014. Online information available at http://www.sdcep.org.uk/index.aspx?o=3245 (accessed March 2015).
Acknowledgements
This study was conducted as part of the TRiaDS programme of research and was funded by NHS Education for Scotland. We would like to thank the TRiaDS Research Methodology Group and all participating dentists and hygienists.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Forbes, G., Rutherford, S., Stirling, D. et al. Current practice and factors influencing the provision of periodontal healthcare in primary dental care in Scotland: an explorative study. Br Dent J 218, 387–391 (2015). https://doi.org/10.1038/sj.bdj.2015.245
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.245
This article is cited by
-
A dentist's dilemma: sharing wellbeing concerns to safeguard Scotland's children
British Dental Journal (2022)
-
The understanding of the basic periodontal examination amongst final year undergraduate students: a survey
BDJ Team (2021)
-
An explorative study of the current practice and attitude towards the management of chronic periodontitis by general dental practitioners in the West Midlands
British Dental Journal (2020)