Key Points
-
Describes referral patterns to oral and maxillofacial units for lower third molars.
-
Highlights the association between mesioangular lower third molars and distal caries on the adjacent second molar.
-
Shows the importance of close monitoring and regular bitewing radiographs when a mesioangular third molar is present.
-
Questions whether prophylactic removal of mesioangular third molars may be of benefit to some patients.
Abstract
Introduction Distal caries in lower second molars has been associated with mesioangular third molars. Caries detection and restoration can be difficult. If caries progresses, root canal treatment or extraction of the second molar can be necessary.
Aims To identify the prevalence of caries in lower third molars and the distal aspect of corresponding lower second molars in patients referred for lower third molar assessment.
Methods Analysis of OPG X-rays for 420 consecutive patients (776 third molars) referred to three maxillofacial centres over a five month period.
Results Thirty-four percent of third molars were mesioangular. There was radiographic evidence of distal second molar caries in 42% of these. When unerupted mesioangular third molars were excluded this increased to 54%. There was no difference in age or dental health of these patients compared to the whole group. There was no angulation of the mesioangular third molar for which distal caries in the second molar was more likely.
Conclusion Distal caries in lower second molars related to a mesioangular third molar is a common finding in oral and maxillofacial patients in secondary care, especially if the third molar is fully or partially erupted. If such a third molar is left in situ, close monitoring and regular bitewing radiographs are recommended.
Similar content being viewed by others
Introduction
Mesioangular wisdom teeth which are partially or fully erupted have been implicated in the development of caries in the distal aspect of the corresponding second molar.1,2,3,4 Historically, prophylactic removal of third molars was common but numerous studies have shown there to be insufficient evidence to support this line of management.5,6,7,8,9,10,11 Guidelines from the National Institute for Clinical Excellence were introduced in 2000 and are currently in use in England and Wales.12 As a result of this many mesioangular third molars are not removed and are retained until later life.
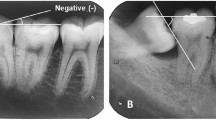
Distal caries in a second molar is more difficult to detect clinically in the presence of a mesioangular third molar. If these lesions remain undetected they will progress, which can lead to the need for root canal treatment or extraction of the second molar (Fig. 1). The clinician therefore faces a dilemma. Do we remove the mesioangular third molar while no disease is present, with the surgical trauma and risks which this involves? Or do we monitor these patients, accepting a risk of caries in the second molar and the possible need for restoration, root canal treatment or extraction of the second molar if clinical monitoring or patient compliance are sub-optimal?
The aim of this study was to identify the prevalence of caries in wisdom teeth and corresponding second molars in patients referred to our oral and maxillofacial departments. We also attempted to identify if caries was more likely for a particular range of angulation of the mesioangular third molar.
Methods
A pilot study was conducted over a two month period in 2007 in the oral and maxillofacial unit at a district general hospital in Surrey (hospital A). The results of this were presented at the local regional audit and other centres were invited to join a more expansive study. Two further oral and maxillofacial units from district general hospitals in the Surrey area where recruited (hospitals B and C).
A clinician from each of the participating units was allocated as the chief data collector for that unit. Data collection commenced on 1 February 2008 and ended on 30 June 2008. Data were collected on each new patient clinic for patients referred to the department for assessment of one or both lower third molars. Eruption status was recorded at the time of consultation. All other data was collected after analysis of the patient's OPG X-ray. If a lower third molar was lone standing (ie no corresponding second molar present), it was excluded from the study. Hospitals A and C used the digital 'PACS' X-ray system while hospital B used the traditional 'hard copy' type.
For each patient the following data were recorded:
-
Hospital number
-
Patient age on date of consultation
-
DMFT (decayed, missing, filled teeth) score was recorded by analysing all teeth except wisdom teeth. Teeth which were decayed, missing for non-orthodontic reasons or filled were allocated a score of 1. The DMFT score was used as a basic means of analysing overall dental health in the subjects. If distal caries was the only lesion present on a lower second molar, this tooth was given a score of zero. As we were looking specifically at this lesion, this allowed us to compare the dental health of those patients with and without distal caries on the second molar
-
Eruption status of each lower wisdom tooth present, ie fully erupted, partially erupted or unerupted
-
Angulation of the lower wisdom tooth as per Winter's classification13
-
Radiographic evidence of caries or restoration in the lower third molar
-
Radiographic evidence of caries or restoration in the distal surface of the lower second molar
-
For all lower third molars classed as mesioangular, the angulation of the lower third molar was recorded. This was defined as the angle created by the intersection of a line through the occlusal plane of the third molar and the mandibular occlusal plane as shown in Figure 2.1 As lack of sharpness of the OPG X-ray was occasionally encountered, the angle was recorded to the nearest five degrees.
After X-ray analysis, the data collected by each centre were reviewed by one of the other clinicians in the study. All X-rays for third molars recorded as mesioangular were re-analysed by the second clinician with specific focus on the presence of caries and the angulation of the third molar. If there was a disagreement as to the presence of caries, the X-ray was re-analysed by both clinicians. If an agreement could not be reached on the presence or absence of caries, the patient was excluded from the study. The final value for the angulation of the third molar was taken as the mean of the values recorded by each of the two assessors.
All analysis was undertaken by clinicians working either full- or part-time in oral and maxillofacial units. Analysis at hospital A was undertaken by two staff grades. Analysis at hospital B was undertaken by an associate specialist and a staff grade. Analysis at hospital C was undertaken by a senior house officer and a staff grade.
All results were recorded in a database and data was imported into SPSS version 12.0.01 (SPSS Inc.) for analysis. Inter-observer variability was calculated using Cohen's kappa statistic. Associations between variables were investigated using the chi-square test and odds ratios were calculated.
Results
Data were recorded for 439 consecutive patients over the five month data collection period. Nineteen patients were excluded as the X-ray was unavailable, resulting in the analysis of 420 patients: 213 from hospital A, 118 from hospital B and 89 from hospital C.
After analysis by two clinicians, there was a difference in opinion regarding the presence of caries in 34 cases. However, there was a good level of agreement between observers. For caries in the third molar the level of agreement was K = 0.85 (95% CI 0.78-0.92) and for distal second molar caries it was K = 0.86 (95% CI 0.80-0.92). When those X-rays causing a difference of opinion were analysed by both clinicians together, a consensus of opinion was reached in all of the cases.
The median age of patients was 28 years (range 14-88, SD = 11.0) and the median DMFT score was 5 (range 0-27, SD = 4.9). As the majority of patients had two lower wisdom teeth present, 776 lower wisdom teeth were analysed in total. Of these, 136 teeth were classified as unerupted, 493 as partially erupted and 147 as fully erupted.
The frequency of the various Winter's angulations are shown in Table 1. There was no difference between the ages of the patients in the four groups.
In total 183 of the 776 lower third molars (23.6%) were carious. Distal caries was identified in the second molar in 150/776 (19.3%). Figure 3 shows the prevalence of caries in the lower third molar relative to Winter's angulation and Figure 4 shows the prevalence of caries in the distal aspect of the lower second molar relative to Winter's angulation.
Third molar caries was significantly associated with mesioangular third molars (χ2 (1) = 7.2, p <0.007). This reflects the fact that 29% of the mesioangular group had caries in the lower wisdom tooth compared to 21% for the other groups combined. Furthermore, the odds ratio revealed that mesioangular third molars were 1.6 times more likely to be carious than other groups combined.
Distal second molar caries was also significantly associated with mesioangular third molars (χ2 (1) = 138.0, p <0.0001). For the mesioangular group 42% had distal second molar caries compared to 7% for other groups combined. The odds ratio indicated that mesioangular third molars were 9.4 times more likely to have distal caries in the associated second molar than the other groups combined.
Looking specifically at mesioangular teeth, 267 teeth were analysed, of which 74 (28%) were classified as unerupted, 176 (66%) as partially erupted and 17 (6%) as fully erupted. Of the 78 cases with caries in the third molar, the median age was 28 years (range 18-57, SD = 7.5) and the median DMFT was 5 (range 0-16, SD = 3.4). Of the 113 cases of caries in the distal aspect of the corresponding second molar, the median age was 28 years (range 16-64, SD = 8.9) and the median DMFT was 5 (range 0-16, SD = 3.8). This shows that there was no difference in either the age of presentation or DMFT of patients with caries in the distal aspect of the lower second molar or third molar compared to wisdom tooth referrals as a whole.
When the angulations of the third molars were considered and divided into groups with intervals of 15 degrees, we found there was no difference between these groups with respect to caries in the third molar or the distal aspect of the second molar (refer to Figs 5 and 6).
The eruption status of the third molar was considered in relation to the prevalence of caries in the third molar and distal aspect of the second molar respectively. One percent of unerupted, 38% of partially erupted and 59% of fully erupted mesioangular third molars were carious. There was distal second molar caries in 11% of unerupted, 55% of partially erupted and 53% of fully erupted mesioangular third molars. Given that the prevalence of caries in the unerupted groups is low, if we exclude unerupted teeth the prevalence of caries in the third molar is 77 out of 193 (40%) and the prevalence of caries in the distal aspect of the second molar is 105 out of 193 (54%).
Discussion
It has been reported that the selection of a population sample for analysis of third molars would be difficult as a random sample of the general population would be required and the taking of radiographs from such persons is ethically questionable.2 We accept that this sample has some bias in that most patients have been referred by their general dental practitioner, making the presence of pathology more likely.
The age of the study population was similar to other studies.3,14 The breakdown of angulations was similar to other studies apart from the horizontal group, which was slightly smaller in our study.2,3 Taking all radiographs together, the prevalence of distal second molar caries was 19.3%, which is more than in Turkish (12.6%),15 Swedish (13%) and Thai (13%) studies but less than American (26%) and Jordanian (21.5%) samples.16,17,18,19
From our results it is clear that distal caries in a second molar related to a mesioangular third molar is a problem in Surrey. Taking the three participating units as a whole, 113 of the 267 mesioangular teeth had caries in the distal aspect of the corresponding second molar, which equates to approximately five teeth per week of the study. We suggest that extrapolating this nationwide would show a large number of lower second molars requiring restoration, root canal treatment or extraction due to the presence of a mesioangular third molar. This is to the detriment of the patient's overall dental health and potentially to the finances of the patient and health service.
Other studies suggest that distal caries in the second molar is a disease of older patients.1,20,21,22 McArdle and Renton found the median age of patents with distal cervical caries in the second molar to be 30 and for their DMFT score to be approximately half the mean score for the general population for various age groups.23 They also found that 82% of mesioangular third molars causing distal cervical caries were of an angulation between 40 and 80 degrees.1 We did not find a difference in the age of patients with a mesioangular third molar and distal caries in the second molar when compared to the group as a whole (median age of both groups was 28). Neither did we find a difference in the DMFT score of the two groups (median score for both groups was 5). Our larger sample size and the fact that our population was Surrey patients may account for this difference. Also, we analysed all carious lesions whereas McArdle and Renton studied only those patients whose second molars had been extracted due to distal caries. We found 73% of cases of second molar distal caries to be associated with a mesioangular third molar with an angulation of 30-75 degrees, but caries also occurred at high levels in other groups. It was not possible to identify a range of angulation for which caries was more likely.
Conclusion
The authors are in agreement with the NICE guidelines,12 in that all unerupted third molars as well as partially or fully erupted third molars classed as vertical, horizontal or distoangular should be left in situ, providing they are pathology and symptom free. However, we feel that the mesioangular third molar which is partially or fully erupted and is related to a lower second molar requires special consideration. Our study shows a high prevalence of patients being referred with distal caries in lower second molars where a partially or fully erupted mesioangular third molar is present. We accept that with careful monitoring, these lesions may be picked up early, which allows the mesioangular third molar to be removed and subsequent restoration of the second molar. However in our experience these patients tend to present with an advanced carious lesion which in turn is difficult to restore. General dental practitioners seem reluctant to attempt restoration of these teeth until the offending third molar is removed, which will allow the lesion to progress further while the patient awaits surgery. Removal of a third molar is not without risks, which can be significant.12,21 However, we feel that when a partially or fully erupted mesioangular third molar is present the possibility of caries in the lower second molar should be discussed as part of the consent process. If the tooth is left in situ, the importance of careful monitoring, regular bitewing radiographs, oral hygiene instruction and preventative advice should be stressed to both general dental practitioner and patient. If the joint decision between clinician and patient is for extraction of the third molar, the current NICE guidance does not encourage this. We feel that our study casts some doubt on this view and a further larger, possibly nationwide study would be useful. In addition, further research into the fate of second molars with distal caries related to mesioangular third molars would be beneficial, as would research into the attitudes of general dental practitioners to restoring these teeth.
References
McArdle L, Renton T . Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of the third molar? Br J Oral Maxillofac Surg 2005; 44: 42–45.
van der Linden W, Cleaton-Jones P, Lownie M . Diseases and lesions associated with third molars. Review of 1001 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79: 142–145.
Knutsson K, Brehmer B, Lysell L, Rohlin M . Pathoses associated with mandibular third molars subjected to removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82: 10–17.
Faculty of Dental Surgery of the Royal College of Surgeons of England. Current clinical practice and parameters of care. The management of patients with third molar teeth. London: Faculty of Dental Surgery of the Royal College of Surgeons of England, 1997.
Weisenfield M D L, Kondis S L . Prophylactic removal of impacted third molars, revisited. Gen Dent 1991; 39: 344–345.
Mercier P, Precious D . Risks and benefits of removal of impacted third molars. J Oral Maxillofac Surg 1992; 21: 17–27.
Toth B . The appropriateness of prophylactic extraction of impacted third molars. A review of the literature. Bristol: Health Care Evaluation Unit, University of Bristol, 1993.
Sands T, Pynn B R, Nenniger S . Third molar surgery: current concepts and controversies. Part 1. Oral Health 1993; 83(5): 11–17.
Sands T, Pynn B R, Nenniger S . Third molar surgery: current concepts and controversies. Part 2. Oral Health 1993; 83(5): 19–30.
Stephens R G, Kogon S L, Reid J A . The unerupted or impacted third molar – a critical appraisal of its pathologic potential. J Can Dent Assoc 1989; 55: 201–207.
Robinson P D . The impacted lower wisdom tooth: to remove or to leave alone? Dent Update 1994; 21: 245–248.
National Institute for Clinical Excellence. Guidance on the extraction of wisdom teeth. London: NICE, 2000.
Winter G B . Principles of exodontia as applied to the impacted third molar. St Louis: American Medical Books, 1926.
Lyssell L, Rohlin M . A study of indications used for removal of the mandibular third molar. Swed Dent J 1987; 11: 23–29.
Polat H B, Özan F, Kara I, Ozdemir H, Ay S . Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: e41–e47.
Lysell L, Brehmer B, Knutsson K, Rohlin M . Judgment on removal of asymptomatic mandibular third molar: influence of the perceived likelihood of pathology. Dentomaxillofac Radiol 1993; 22: 173–177.
Punwutikorn J, Waikakul A, Ochareon P . Symptoms of unerupted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87: 385–390.
Knutsson K, Brehmer B, Lysell L, Rohlin M . Asymptomatic mandibular third molars: oral surgeons' judgment of the need for extraction. J Oral Maxillofac Surg 1992; 50: 329–333.
Al-Khateeb T H, Bataineh A B . Pathology associated with impacted mandibular third molars in a group of Jordanians. J Oral Maxillofac Surg 2006; 64: 1598–1602.
Brickley M R, Shepherd J P . An investigation of the rationality of lower third molar removal, based on USA National Institutes of Health criteria. Br Dent J 1996; 180: 249–254.
de Boer P J, Raghoebar M, Stegenga B, Scheon PJ, Boering G . Complications after third molar extraction. Quintessence Int 1995; 26: 779–784.
Nordenram A, Hutlin M, Kjellman O, Ramstrom G . Indications for removal of the mandibular third molar. Swed Dent J 1987; 11: 23–29.
Office for National Statistics. Adult dental health survey. Oral health in the United Kingdom, 1998. London: HMSO, 1998.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Allen, R., Witherow, H., Collyer, J. et al. The mesioangular third molar – to extract or not to extract? Analysis of 776 consecutive third molars. Br Dent J 206, E23 (2009). https://doi.org/10.1038/sj.bdj.2009.517
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.517
This article is cited by
-
3rd molar surgery and consent
BDJ Student (2020)
-
Bucco alveolar bone thickness of mandibular impacted third molars with different inclinations: a CBCT study
Surgical and Radiologic Anatomy (2020)
-
Third Molar and Their Relationship with Caries on the Distal Surface of Second Molar: A Meta-analysis
Journal of Maxillofacial and Oral Surgery (2018)
-
NICE or not so NICE?
British Dental Journal (2013)
-
Summary of: The effects of NICE guidelines on the management of third molar teeth
British Dental Journal (2012)