Abstract
Study design:
Retrospective study.
Objectives:
The purpose of this investigation was to review the outcomes and safety of retrograde ureteroscopic laser lithotripsy (URS) for the treatment of urolithiasis in the spinal cord injury (SCI) population.
Setting:
Virginia, USA.
Methods:
All patients with SCI who underwent URS with holmium:YAG laser lithotripsy for urolithiasis over a 15-year period were identified. Stone size, location and number at presentation were recorded. Information regarding patient characteristics, intra-operative complications, surgical efficacy, stone clearance, peri-operative complications, and follow-up stone events was collected and analyzed.
Results:
A total of 67 URS procedures were performed on 29 SCI patients during the study period with an average follow-up of 3.4 years. Patients had an average of 2.3 ipsilateral ureteroscopies. The majority (85.1%) used indwelling catheters for long-term bladder management, and complete stone clearance after the first procedure was 34.3%. Of the 44 cases with residual stones >4 mm, 20 (45.5%) were secondary to technical or procedural limitations. The intra-operative complication rate was comparable to non-SCI studies at 1.5%, but peri-operative complications were significantly higher at 29.9% with the majority due to urosepsis. Factors associated with peri-operative complications include chronic obstructive pulmonary disease, motor incomplete injuries and lack of a pre-operative ureteral stent.
Conclusion:
URS in the SCI population is an effective treatment for ureteral or renal stones but may be associated with greater risks and reduced efficacy.
Sponsorship:
None.
Similar content being viewed by others
Introduction
Urolithiasis is a frequent complication of individuals with spinal cord injury (SCI), which occurs with an incidence of 4–7%. Indwelling catheters, bladder dyssynergia, recurrent urinary tract infections (UTIs), hypercalcuria and vesicoureteral reflux place this population at a higher risk.1 Current treatment options for urolithiasis include shockwave lithotripsy (SWL), percutaneous nephrolithotripsy, retrograde ureteroscopic lithotripsy (URS), laparoscopic lithotomy or open lithotomy.
With advances in endourology, ureteroscopic surgery has become a popular choice for the minimally invasive treatment of urolithiasis. In the general population, studies reveal stone-free rates between 77 and 93% after one procedure. Success varies depending on size, number and location of stones.2, 3, 4, 5 Intra-operative complications range between 0 and 6%, and major peri-operative complications between 1 and 3%.2, 4, 6 Unfortunately, it is not known whether these studies are directly applicable to patients with SCI. SCI results in neurogenic bladder, which significantly alters bladder function including ability to empty, bladder pressure, continence and bladder compliance.7 Detrusor-sphincter-dyssynergia, a common problem in SCI patients with neurogenic bladder dysfunction, can cause elevated detrusor pressures. Over time, fibrosis and contracture of the bladder wall lead to reduced compliance, vesicoureteral reflux, and may impact stone formation and clearance rates.8
To our knowledge, no published data are available regarding surgical outcomes or complication rates of URS with laser lithotripsy in the SCI population. Therefore, the purpose of our investigation was to review the outcomes and safety of URS with laser lithotripsy to allow physicians to more accurately counsel SCI patients regarding the risks and benefits of URS.
Methods
This study was approved by the Institutional Review Board at the McGuire Veterans Affairs Hospital where the overwhelming majority (97.5%) of SCI patients are males. Electronic medical records of all SCI patients who underwent URS for urolithiasis between 1995 and 2010 were retrospectively reviewed. Patients were identified by cross-referencing URS current procedural terminology codes with an active registry of SCI patients. Patients were excluded if they required URS for reasons other than urolithiasis, were over the age of 89 (to reduce risk of identification), or did not have neurogenic bladder, defined as partial or complete bladder dysfunction due to a known neurologic injury.
Pre-operative preparation
All patients had pre-operative urine cultures and were given culture-specific or broad-spectrum (in cases where contaminated specimens or multiple species were identified) antibiotics pre-operatively that continued for at least 48 h post-operatively. Stents were placed pre-operatively, before the day of surgery, in all patients who originally presented with urosepsis, obstruction or renal insufficiency. The method of anesthesia was determined by the attending anesthesiologist as a function of patient safety and personal preference.
URS technique
URS was performed with a holmium:YAG laser (American Medical Systems, Inc., Minnetonka, MN, USA) employing 200–365 μM laser fibers. In general, distal ureteral stones were accessed with rigid scopes and proximal stones with flexible scopes. Procedures were performed with the intention to ablate all ipsilateral calculi to fragments of <1 mm in greatest diameter. A ureteral stent was placed at the conclusion of all procedures in which ureteral access was successfully achieved. Routine use of antegrade guide wires to help with identification of ureteric orafices was not performed. However, all possible maneuvers were performed to achieve successful ureteral access intra-operatively including leg extension, use of multiple guide wires, use of external abdominal pressure and the use of ureteral balloon dilation.
Post-operative management
Follow-up imaging was performed 1–14 days post-operatively to evaluate for residual stone burden. This imaging included a kidneys, ureter, and bladder xray, renal ultrasound or CT scan depending on body habitus, stone type and surgeon preference. Residual stone size was recorded based on the radiology report. If no size was specified, then images were directly reviewed by one of the authors (TW) and measured using iSite Enterprise (Philips Electronics, Inc., Andover, MA, USA) imaging software. Decision for stent removal was made based on stone size (⩽4 mm), lack of symptoms (i.e. recurrent UTI or pain), or resolution of obstruction. If residual stone burden was significant, then the patient was scheduled for a repeat intervention.
The time period used to define peri-operative complications was <30 days. Co-morbidities of chronic obstructive pulmonary disease, coronary artery disease, diabetes mellitus and hypertension were specifically selected in this study as each may impact surgical risks. The primary method of bladder management was recorded to determine possible associations with surgical outcomes.
Statistics
Univariate comparisons of patient variables were performed against outcomes of intra-operative complications, peri-operative results and follow-up events to identify factors associated with improved or reduced outcomes. Statistical analyses were performed using Wilcoxon Rank Sums (for continuous variables) and Fisher’s Exact tests (for categorical variables) where appropriate. All analyses were performed by a dedicated statistician blinded to the study data using SPSS 11.0 software (IBM Corporation, Armonk, NY, USA). Data are reported as mean values±s.e.m., and P-values of <0.05 were considered significant.
Results
A total of 67 URS with laser lithotripsy were performed on 29 SCI patients during the study. Patient demographics, neurologic history and medical co-morbidities are listed in Table 1. The average patient had 2.3 ipsilateral URS performed. For patients who required multiple interventions, each procedure was counted as a unique case. One patient underwent bilateral ureteroscopic procedures on the same day, which was counted as two separate procedures. All patients in this study were male. Average age at time of URS was 52.7±1.38 years old (31–86), and average length of time to URS from date of initial injury was 18.2±1.3 years (1–40). Average follow-up after each procedure was 3.4±0.4 years (0–12 years). The majority of stones were located within the kidney (64.2%) with a range of sizes and numbers as shown in Table 2. A majority of cases (74.6%) had more than one stone upon presentation, and 25.4% required at least one contralateral stone treatment at a later date.
In terms of urologic history, the majority of patients used indwelling catheters as the primary means of bladder management (85.1%). Patients had prior urologic procedures for reasons other than urolithiasis in 34.3%, and 47.8% had prior treatments for ipsilateral stones. The most common indication for URS was recurrent UTI. In addition, 62.7% of cases had concurrent contralateral stones (Table 3).
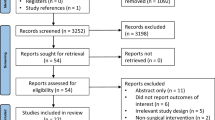
A summary of all outcomes including rates of residual stones, intra-operative complications, peri-operative complications and follow-up ipsilateral stone events is shown in Figure 1.
Intra-operative results
Intra-operative complications occurred in one patient (1.5%) due to ureteral perforation. There were no cases of intra-operative autonomic dysreflexia (AD) despite 58% of patients with past medical history of this condition. The majority of cases (63%) were performed with regional anesthesia with 20.9% receiving conscious sedation, and 16.4% receiving general anesthesia. A pre-operative (before the day of surgery) stent was placed in 58.2% of cases.
Surgical efficacy and stone clearance
Complete stone clearance, as defined as removal of any stone larger than 4 mm, was obtained in only 34.3% of cases. There were 44 cases (65.7%) with residual stones >4 mm based on the initial post-operative imaging. Twenty (45.5%) of these cases were secondary to technical or procedural reasons including inability to identify or pass the scope through the ureteral orifice in 9 of 20 (45%) cases and inability to successfully access all of the stones in 8 of 20 (40%) cases. Patient age at the time of the procedure was associated with incomplete clearance. The mean age of patients with successful clearance was 50.9±1.6 years as compared with 57.0±2.5 years for patients with incomplete clearance (P=0.02). Also, those patients who had undergone urodynamic evaluations at any time before the surgery (n=50, 74.6%) had a significantly greater chance of failure (39/50, 78%) compared with those who did not (8/17, 47.1%), (P=0.03).
Peri-operative results
The peri-operative (within 30 days) complication rate was 29.9%. Specific complications are shown in Figure 2. Urosepsis was the most common complication identified in 12 of the 67 cases (17.9%) with respiratory failure and acute outlet obstruction each occurring in 3 (4.5%) cases. One case resulted in death from urosepsis and respiratory failure. Of note, some of the patients developed more than one complication. Patients who had pre-operative (before the date of procedure) ureteral stent placement had lower peri-operative complication rates (P=0.02). Chronic obstructive pulmonary disease was associated with higher rates of peri-operative complications (P=0.02), but other medical co-morbidities including hypertension, diabetes and history of AD were not significant. Mean operative time was 87±5.0 min and did not differ in patients who experienced peri-operative complications. Surprisingly, motor incomplete SCI was associated with higher peri-operative complications than motor complete SCI (P=0.02), Figure 3.
Univariate comparisons identified pre-operative stent placement (Stents), chronic obstructive pulmonary disease (COPD), and incomplete SCI as factors that were associated with higher peri-operative complication rates. (+) positive for the factor (gray bars) and (−) negative for the factor (black bars). *P<0.05.
Follow-up interventions
The majority of cases (71.6%) required at least one follow-up intervention ipsilaterally. The decision to perform another urological intervention was based on residual stone size, symptoms (recurrent UTI, pain and so on) and/or persistent obstruction. The procedures used in follow-up were repeat ureteroscopy (31%), SWL (16%) and percutaneous nephrolithotripsy (15%). Patients required no follow-up intervention in 29% of cases and 9% had other types of interventions. No factors other than increased age (P=0.01) were associated with the occurrence of follow-up stone events. Patients did not receive prophylactic medical therapy to prevent recurrent stones.
Discussion
In this study of URS in the SCI population, complete stone clearance, defined as removal of any stone larger than 4 mm, was obtained in only 34.3% of cases. This is significantly lower than reported clearance rates of 77–93% for URS in the non-SCI population.2, 4, 5 In the SCI population, average clearance rates using SWL are 44–55%,9, 10, 11 and percutaneous nephrolithotripsy clearance rates are 54–87%.12, 13
One possible explanation for the high failure rate of URS in the SCI population may be that chronic neurogenic bladder dysfunction can cause fibrosis and bladder wall contractures which alter the ureteral orifice and urethral anatomy.14 In addition, patients with SCI often suffer from lower extremity contractures making positioning in the lithotomy position difficult or impossible.15 In our current series, nearly half (45.5%) of failures were due to technical limitations (inability to access the ureteral orifice or inability to access stones), making this an important factor for patient counseling. Interestingly, pre-procedure placement of a ureteral stent did not prevent technical failures. As reported in other investigations,16 increased age was associated with higher rates of peri-operative complications. To our knowledge, the use of antegrade guide wires to identify the difficult ureteral orifice has not been studied and the technique should be considered in future investigations.
As reported previously,16 increased age was associated with higher rates of peri-operative complications. However, the reason that patients who received urodynamics evaluations had lower stone clearance rates is unclear. One possible explanation is that patients selected for urodynamics studies may have more severe bladder dysfunction. To improve efficacy, percutaneous nephrolithotripsy could be used as an alternative to URS in patients with large or multiple renal calculi. However, this technique is also associated with potential complications and often requires dependence on an experienced interventional radiologist. Another alternative technique to prevent post-operative urosepsis is use of anti-reflux stents. However, the efficacy of these stents in the prevention of urosepsis is not widely accepted.17, 18
In our study, 29.9% of cases had peri-operative complications, which is much higher than reported rates of 1–3% in non-SCI patients.2, 4 Urosepsis, which occurred in 17.9% of the cases or 60% of those with complications, was most common. These complications occurred despite prophylactic antibiotic coverage based on urine culture sensitivities or broad-spectrum coverage. The published rate of urosepsis in the general population is 3% for those undergoing URS for ureteral stones.6 Several possibilities exist for this significantly higher rate of post-operative urosepsis. Chronic neurogenic bladder is often associated with limited bladder compliance, and pressure irrigation, commonly performed during URS, may lead to intravasation of contaminated fluid. It is also well known that SCI individuals are frequently colonized with drug-resistant bacteria, and infection stones are far more common in this population.19 Due to high rates of urosepsis in current study, the authors recommend consideration of intra-operative urine cultures from the renal pelvis to identify occult bacterial species. Preventative strategies including infection control and metabolic evaluations with medical management are clearly needed in SCI patients.
In this study, the factor most significantly associated with improved peri-operative outcomes was pre-procedure placement of a ureteral stent. Our current practice has been to place a stent only if obstructive or infectious symptoms are present and then to schedule the patient for definitive treatment at a later date. However, data from the current study suggest that pre-procedure (that is, before the day of surgery) stent placement might significantly improve outcomes. Further studies are required to investigate the benefit of pre-operative stent placement in asymptomatic individuals with SCI and renal or ureteral calculi.
In the current series, the peri-operative respiratory failure rate of 4.5% was higher than rates of <1% reported in the general population.5 However, the finding that incomplete SCI was associated with worse peri-operative outcomes is difficult to understand and might simply reflect the small numbers of cases with incomplete SCI in the study (13.4%). In addition, our peri-operative obstruction rate of 4.5% was similar to rates reported in the general population.5, 6 Surprisingly, there were only two cases of documented AD. The incidence of AD appears to be significantly higher with SWL in the SCI population, ranging between 16 and 95%. Of note, the study that reported a 95% incidence was specifically evaluating AD rate during SWL performed on SCI patients without anesthesia.9, 20 All other recorded outcomes were similar to rates reported in the general population including peri-nephric hemorrhage, post-op ileus and death.
In terms of follow-up stone events, the majority of cases required follow-up ipsilateral stone procedures. However, contralateral stone treatments were also required in 25.4%. Many of these follow-up procedures were required for new stone formation and some were required after the stone continued to enlarge or became symptomatic. In any event, this high percentage of stone growth, recurrence, or new stone formation suggests the need for vigilant follow-up with serial imaging.
Limitations of this study are the small sample size, the retrospective design, and that all subjects were male. The number of patients in current study is limited due to the defined population of SCI patients and the nature of the referral SCI center in which patients may receive care at local hospitals. In addition, the use of individual cases, rather than individual patients, could bias some results but was necessary in this limited population.
Conclusion
URS in the SCI population is an effective treatment for ureteral or renal stones but may be less efficacious with higher peri-operative complications than similar procedures performed in non-SCI patients. Generally, more than one procedure is required to effectively clear the stone burden regardless of stone location or size. The risk of post-operative urosepsis is significantly higher than the general population and warrants further investigation for preventative strategies. Pre-operative stent placement appears to have a protective effect regardless of the initial indication for surgery. Extended peri-operative medical supervision is recommended given the high complication rates in the SCI population.
References
Chen Y, DeVivo MJ, Roseman JM . Current trend and risk factors for kidney stones in persons with spinal cord injury: a longitudinal study. Spinal Cord 2000; 38: 346–353.
Fabrizio MD, Behari A, Bagley DH . Ureteroscopic management of intrarenal calculi. J Urol 1998; 159: 1139–1143.
Grasso M . Ureteropyeloscopic treatment of ureteral and intrarenal calculi. Urol Clin North Am 2000; 27: 623–631.
Jiang H, Wu Z, Ding Q, Zhang Y . Ureteroscopic treatment of ureteral calculi with holmium:YAG laser lithotripsy. J Endourol 2007; 21: 151–154.
Sofer M, Watterson JD, Wollin TA, Nott L, Razvi H, Denstedt JD . Holmium:YAG laser lithotripsy for upper urinary tract calculi in 598 patients. J Urol 2002; 167: 31–34.
Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M et al2007 Guideline for the management of ureteral calculi. J Urol 2007; 178: 2418–2434.
Klausner AP, Steers WD . The neurogenic bladder: an update with management strategies for primary care physicians. Med Clin North Am 2011; 95: 111–120.
Garcia-Nieto V, Siverio B, Monge M, Toledo C, Molini N . Urinary calcium excretion in children with vesicoureteral reflux. Nephrol Dial Transplant 2003; 18: 507–511.
Niedrach WL, Davis RS, Tonetti FW, Cockett AT . Extracorporeal shock-wave lithotripsy in patients with spinal cord dysfunction. Urology 1991; 38: 152–156.
Deliveliotis C, Picramenos D, Kostakopoulos A, Stavropoulos NI, Alexopoulou K, Karagiotis E . Extracorporeal shock wave lithotripsy in paraplegic and quadriplegic patients. Int Urol Nephrol 1994; 26: 151–154.
Lazare JN, Saltzman B, Sotolongo J . Extracorporeal shock wave lithotripsy treatment of spinal cord injury patients. J Urol 1988; 140: 266–269.
Culkin DJ, Wheeler JS, Nemchausky BA, Fruin RC, Canning JR . Percutaneous nephrolithotomy in the spinal cord injury population. J Urol 1986; 136: 1181–1183.
Lawrentschuk N, Pan D, Grills R, Rogerson J, Angus D, Webb DR et al Outcome from percutaneous nephrolithotomy in patients with spinal cord injury, using a single-stage dilator for access. BJU Int 2005; 96: 379–384.
Comperat E, Reitz A, Delcourt A, Capron F, Denys P, Chartier-Kastler E . Histologic features in the urinary bladder wall affected from neurogenic overactivity--a comparison of inflammation, oedema and fibrosis with and without injection of botulinum toxin type A. Eur Urol 2006; 50: 1058–1064.
Ramsey S, McIlhenny C . Evidence-based management of upper tract urolithiasis in the spinal cord-injured patient. Spinal Cord 2011; 49: 948–954.
Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ . Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the national surgical quality improvement program. J Bone Joint Surg Am 2011; 93: 1577–1582.
Ecke TH, Bartel P, Hallmann S, Ruttloff J . Evaluation of symptoms and patients′ comfort for JJ-ureteral stents with and without antireflux-membrane valve. Urology 2010; 75: 212–216.
Battaglia M, Ditonno P, Selvaggio O, Palazzo S, Bettocchi C, Peschechera R et al Double J stent with antireflux device in the prevention of short-term urological complications after cadaveric kidney transplantation: single-center prospective randomized study. Transplant Proc 2005; 37: 2525–2526.
Matlaga BR, Kim SC, Watkins SL, Kuo RL, Munch LC, Lingeman JE . Changing composition of renal calculi in patients with neurogenic bladder. J Urol 2006; 175: 1716–1719 discussion 1719.
Kabalin JN, Lennon S, Gill HS, Wolfe V, Perkash I . Incidence and management of autonomic dysreflexia and other intraoperative problems encountered in spinal cord injury patients undergoing extracorporeal shock wave lithotripsy without anesthesia on a second generation lithotriptor. J Urol 1993; 149: 1064–1067.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wolfe, T., Klausner, A., Goetz, L. et al. Ureteroscopy with laser lithotripsy for urolithiasis in the spinal cord injury population. Spinal Cord 51, 156–160 (2013). https://doi.org/10.1038/sc.2012.86
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.86
Keywords
This article is cited by
-
Incidence and safety outcomes associated with active stone removal procedures (ASRP): a comparison between neurological and non-neurological patients using the French National Health Data Base
World Journal of Urology (2022)
-
Surveillance and management of urologic complications after spinal cord injury
World Journal of Urology (2018)
-
Flexible ureteroscopic laser lithotripsy for upper urinary tract stone disease in patients with spinal cord injury
Urolithiasis (2015)
-
Surgical Management of Urolithiasis in Spinal Cord Injury Patients
Current Urology Reports (2014)
-
Voiding Dysfunction and Upper Tract Deterioration after Spinal Cord Injury
Current Bladder Dysfunction Reports (2013)