Abstract
Study design:
Cross-sectional, non-experimental design.
Objectives:
(1) Determine the sensitivity and specificity of the general population body mass index (BMI) cutoff for obesity (30 kg m−2) in a representative sample of persons with spinal cord injury (SCI); (2) develop a more sensitive BMI cutoff for obesity based on percentage of fat mass (%FM) and C-reactive protein (CRP).
Setting:
Ontario, Canada.
Methods:
A total of 77 community-dwelling adults with chronic SCI underwent anthropometric measures (%FM by bioelectrical impedance analysis, length, weight, BMI (kg m−2)) and provided blood samples to determine CRP. Sensitivity and specificity analyses, piecewise regression, non-linear regression, and receiver–operator characteristic curves were used to determine new BMI cutoffs.
Results:
A BMI cutoff of 30 kg m−2 failed to identify 73.9% of obese participants vs 26.1% at a lowered cutoff of 25 kg m−2. BMI cutoffs based on risk levels of the %FM and CRP considered together ranged from 22.1 kg m−2–26.5 kg m−2.
Conclusions:
People with chronic SCI and BMI values >22 kg m−2 should be considered as being at high risk for obesity and obesity-related chronic diseases.
Sponsorship:
Canadian Institutes of Health Research.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) results from incidents causing acute SCI, most commonly motor vehicle mishaps, and affects 20 000 North Americans each year.1, 2 On account of advances in acute medical care, the primary causes of mortality after an SCI have shifted from urogenital diseases2 to respiratory and cardiovascular diseases (CVDs). Both of these diseases are commonly associated with obesity, and their prevalence in the SCI population surpasses the prevalence rates in the able-bodied population.3
On account of its ease of use and low cost, body mass index (BMI; weight (kg)/height (m2)) is the most common screening tool in able-bodied populations to identify those who are obese and at risk for obesity-related chronic disease.4 The World Health Organization has identified a BMI of 30 kg m−2 as the cutoff above which able-bodied people are considered obese and at risk for chronic diseases such as CVD. Despite being developed in the able-bodied population, BMI is often applied to those with SCI, both clinically and in research studies. Mean BMI in studies of people with SCI ranges from 23.1 to 25.7 kg m−2,5, 6, 7, 8 whereas the percentage of fat mass (%FM) in these same samples ranges from 27.5 to 36.3%, consistent with obesity fat mass (FM) values.9 This suggests that BMI underestimates obesity, leading to a failure in the identification of persons with SCI who are truly obese by the %FM.
Low-grade inflammation, characterized by elevated C-reactive protein (CRP), is indicative of the inflammation associated with CVD,10 and has been included in other algorithms to estimate risk.11 The development of new BMI cutoffs to identify obese persons with SCI, and which are based on the measured %FM and biological variables, such as CRP, would allow clinicians to intervene earlier in the hopes of reducing obesity-related morbidity and mortality in this population. With these issues in mind, our objectives were to (1) determine sensitivity of the current BMI obesity cutoff of 30 kg m−2 in a representative sample of persons with chronic SCI; (2) develop a more sensitive obesity BMI classification system based on measured percent body fat and the novel biological marker, CRP.
Materials and methods
Participants
The Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI) is an observational cohort study of physical activity and health of community-dwelling adults with chronic, traumatic, SCI in Ontario, Canada. Methods for SHAPE SCI have been published.12 Data for the current study were drawn from the SHAPE SCI substudy, the purpose of which was to examine risk factors for, and the presence of, chronic disease. Participants were men and women ⩾18 years, ⩾1-year post-traumatic SCI, and who lived within 200 km of McMaster University.
The Research Ethics Boards of Hamilton Health Sciences and University of Guelph approved the protocol. Written, informed consent was obtained from each participant before participation. Substudy participants were given a nominal honorarium.
Methods
Demographic information including age, sex, ethnicity, location and level of lesion, and family and personal medical histories, was collected from each participant by trained interviewers using a structured questionnaire during a home visit. Weight was taken with participants wearing light clothing, to the nearest 0.1 kg using a portable, digital wheelchair scale (Health O Meter 2450KL, Brooklyn, NY, USA). The weight of the wheelchair was subtracted from the weight of the participant sitting on the wheelchair. Participants then transferred to a length board (National Lifesaving Society item EQ-10, Edmonton, AB, Canada) positioned on a bed. Participants' legs were straightened, heads positioned in the Frankfurt plane, and feet placed in dorsal flexion. Length was determined using an elastic tape measure, measuring segmentally from heel to knee, knee to hip and hip to head. Body composition was measured using whole-body bioelectrical impedance analysis (RJL Systems Bioelectrical Body Composition Analyzer Quantum II, Clinton Twp., MI, USA) and the electrode placement of Lukaski et al.13 Participants were asked to fast for 12 h, avoid alcohol and exercise for 24 h before testing and void bladders and catheters 30 min before testing. Total body water (TBW) was determined as follows:14


where weight is in kg, stature is in cm and resistance is in ohms. TBW was divided by 0.732, the lean tissue hydration constant15 to determine fat-free mass. FM was calculated as body weight (kg)–fat-free mass (kg). The coefficient of variation of duplicate resistance values, performed on five participants, was 0.22%.
Blood was taken after a 12-h overnight fast, stored on ice in a lightfast container, centrifuged and analyzed at McMaster University Medical Center on the same day as collection. High sensitivity CRP was determined using particle enhanced immunonephelometry (CardioPhaseTM hsCRP, Dade Behring; Mississauga, ON, Canada). A CRP of ⩾3 mg l−1 was used as the cutoff point to identify persons at high risk of CVD.10
Data analysis
Analysis of the sensitivity and specificity of BMI cutoffs of 30 kg m−2 and 25 kg m−2, relative to the %FM cutoffs for obesity,9 was performed using SPSS (Statistical Package for the Social Sciences, v. 15.0, Chicago, IL, USA). Six participants were excluded from the sensitivity and specificity analysis due to missing length (n=2), weight (n=1) or bioelectrical impedance analysis measurement (n=3). BMI cutoffs were determined from the %FM using non-linear regression. On account of the small number of female participants (n=14), only males were used for the non-linear regression analysis (n=60). Sample size for non-linear regression was calculated using a effect size of 0.15, an α level of 0.05, and a desired power of 0.80 to determine a minimum required sample of 54 participants.16, 17 Piecewise linear regression was used to determine BMI cutoffs from CRP. Male and female participants with CRP values ⩾10 mg l−1 were excluded from this analysis, resulting in a sample of 57. Determination of BMI cutoffs to identify men with both high CRP (3–10 mg l−1) and high %FM (⩾22%, indicative of obesity) was completed using a receiver–operator characteristic curve. Fourteen participants were included in this analysis.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Demographic and injury characteristics are presented in Table 1. Values for BMI and %FM, which were used for all analyses, are presented in Table 2. Mean CRP for the sample was 3.3±2.8 mg l−1. The BMI cutoff of 30 kg m−2 had a sensitivity of 20.5% and a positive predictive value of 100%, both of which changed to 73.9 and 89.5%, respectively, with a BMI cutoff of 25 kg m−2 (Table 3). That is, 73.9% of people with obese %FM levels were identified by a BMI of 25 kg m−2, and of the 38 participants identified as obese using a BMI cutoff of 25 kg m−2, 89.5% were also identified as obese by the %FM.
A two-slope piecewise regression model was then used to estimate the BMI at which the %FM started to increase to levels of concern (that is, obesity). Convergence of the model required seven iterative steps, with the last iteration having a sum of squares of 1396.3, and a slope of 0.01 below the cutoff of 22.1 kg m−2 and a slope of 0.53 above the BMI cutoff at an FM of 22.4% (Figure 1, Table 4). A BMI range of 26.5 to 29.8 kg m−2 was associated with a CRP value of 2.6 mg l−1 (Figure 2, Table 4), the value associated with moderate CVD risk in the able-bodied population.18 This range was determined from the r2-value of the model above and below the CRP cutoff of 2.6 (<0.01, 0.05), Thus, participants with BMI of 26.5–29.8 kg m−2 tended to have a CRP at 2.6 mg l−1, associated with moderate CVD risk.
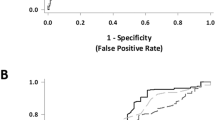
The creation of a risk variable based on elevated CRP and elevated %FM identified 14 male participants with both a CRP ⩾3.0 mg l−1, the high-risk cutoff for CVD,10 and a %FM of ⩾22, indicative of obesity in men.9 When this variable was plotted against BMI using receiver–operator characteristic curves, the BMI value of 25 kg m−2 was identified as having the best combination of sensitivity (0.90) and specificity (0.52; Table 4). The area under the curve was 0.77, relatively close to the ideal area under the curve of 1.0 (Figure 3).
Discussion
This study contributes to a growing body of literature examining the use of BMI in the SCI population to identify obesity, and is the first to suggest lower BMI cutoffs based on both %FM and CRP as biomarkers. The major findings were the following: (1) The current BMI cutoff of 30 kg m−2 fails to identify 73.9% of persons with SCI who are truly obese; (2) persons with a SCI and a BMI ⩾22.1 kg m−2 may be candidates for lifestyle and/or medical interventions to reduce risk of obesity-related chronic diseases, or at the very least, are candidates for further screening.
Persons with SCI commonly have up to 15% more body fat than BMI-matched able-bodied controls.19 This discrepancy is due to the lack of neuronal stimulation below the site of injury as well as a drastic decrease in physical activity, causing a loss of lean muscle and bone and an accretion of adipose tissue after SCI.6 These changes lead to an increase in obesity based on the %FM that has the potential of not being captured by BMI because both weight and BMI tend to remain unchanged in the SCI population. Not surprisingly, we found that the BMI cutoff of 30 kg m−2 failed to identify 73.9% of those who were obese. This shortcoming is not trivial as the identification of people who are obese is crucial to identify those at risk for obesity-related chronic diseases such as CVD. When a BMI of 25 kg m−2 was used instead, 53.4% more participants were appropriately categorized as obese. Remarkably consistent with our findings, a small study5 of men with paraplegia reported that the obesity cutoff of 30 kg m−2 failed to identify 80% who are truly obese, with a decrease in misidentification of 40% when the BMI cutoff was lowered to 25 kg m−2.
Using %FM, we noted that a BMI of 22.1 kg m−2 is associated with an %FM 22.4% in men. This FM percentage is indicative of obesity in men aged 18–40 years and approximates the obesity cutoff for men aged 41–60 years (>25%), and aged 61+years (>23%).9 This indicates that decreased BMI cutoffs more accurately capture obesity when defined on the basis of %FM in specialized populations such as those with SCI.
We found that a BMI range of 26.5–29.8 kg m−2 was associated with cardiovascular risk based on the American Heart Association definitions for CRP. The lower end of the BMI range approached the lowered BMI cutoff of 25 kg m−2, which showed improved sensitivity and predictive value in our sample. Ideally, one BMI point would have corresponded with a CRP of 2.6 mg l−1 as opposed to the 3.4 kg m−2 range as indicated in Figure 2. The range likely would have been smaller if the sample had been larger to reduce the variation.
Preliminary evidence suggests that CRP is a major risk factor for the high prevalence of CVD in the SCI population. Indeed, one study showed that men with SCI who were free of infection were 2.29 times more likely to have CRP >3 mg l−1 than able-bodied matched controls.20 CRP, together with low high-density lipoprotein cholesterol levels, may be a major CVD risk factor for those with SCI.20 This is critical as the metabolic profile of those with SCI often appears normal for traditional biomarkers associated with CVD risk,21 even though they have a higher rate of CVD mortality than able-bodied population. It thus makes sense to include a biological marker, such as CRP, as a factor on which to base new BMI cutoffs. In support of this, in an able-bodied population, CRP has been shown to improve the predicative ability of the Framingham risk score.11
In a subset of the participants who were part of this study (n=65), it was earlier reported that only 2.4–18.4% people had metabolic syndrome (as identified by traditional definitions), compared with 19.4–39.0% in the able-bodied population.21 Given the low prevalence of metabolic syndrome in the SHAPE SCI substudy sample, the average FM of 29.4%, found in this study (indicating obesity and high risk), was unexpected. When looking beyond the traditional biomarkers for CVD risk, CRP was the only biomarker indicative of high risk (3.1 mg l−1).21 Our determination of a BMI cutoff based on CRP, one of the most probable indicators of CVD risk in the SCI population, is a notable contribution to the literature.
A BMI cutoff above which participants had both a %FM, indicative of obesity (⩾22.1%), and a CRP, associated with high risk for CVD (⩾3.0 mg l−1), would be the most relevant in identifying those most in need of intervention. On the basis of this combined risk factor variable, a BMI of 25 kg m−2 was determined by the receiver–operator characteristic curve as the most appropriate cutoff because of its high sensitivity (0.90), although still maintaining a reasonable specificity (0.52). The sacrifice in specificity is appropriate for a screening tool as its intention is to be a first cut, warranting further tests to identify the specific level of risk for those individuals identified as potentially at risk for obesity-related chronic disease by BMI.
Strengths and limitations
To our knowledge, this study of the utility of BMI included the largest and most representative sample to date of people with SCI (n=77). This study involved men and women with both complete and incomplete paraplegia and tetraplegia, more representative of the SCI population than many other studies published in the current literature. Because of the home-based nature of this study, health and mobility did not prevent participation, and we were able to recruit a larger, more generalizable sample than that typically reported in SCI studies or that is available for hospital or university-based testing.
Our use of a novel biomarker (CRP) to identify BMI cutoffs is an important strength of the study, because it has been shown that the traditional CVD risk factor profile is not present in the SCI population,21 despite an increased rate of CVD compared with the able-bodied population. However, we recognize the controversy of measuring CRP in this population due to the possible presence of urinary tract infections and pressure sores. To address this, we excluded participants with CRP ⩾10 mg l−1 (n=15), a level commonly associated with infection.
Although we do acknowledge that bioelectrical impedance analysis is subject to violation of the assumptions of hydrostatic weighing, the portable options for body composition assessment were limited due to the home-based visits. Ideally, the use of a measure that has been validated against the four-compartment modeling would have been advantageous; however was not a possibility because of the nature of the home visits and the financial cost of these techniques.22 The cutoffs of the %FM that we used were developed in an able-bodied population.9 We acknowledge that these cutoffs may not be ideal for a disabled population; however, we also point out that they are used as a reference in SCI populations.5
When performing the sensitivity analysis, participants were analyzed in subgroups according to both age and gender. On account of the wide age range of the small sample of women, this analysis may not represent the ability for a BMI of 25 kg m−2 to more accurately capture obese women with SCI. Women (n=14) were included in the analysis because of the lack of studies on women in the SCI literature. The non-linear modeling used to predict BMI based on the %FM and the nature of cutoffs for %FM9 in a small number of women precluded their inclusion in this analysis. The small number of men per age group resulted in the use of one group regardless of age to estimate BMI by %FM.
This study shows that the current BMI cutoff fails to identify most obese individuals in the SCI population, as defined by the %FM and risk of obesity-related chronic disease based on CRP. We provide evidence to the clinical and scientific communities supporting the use of lower BMI cutoffs (that is, above 22 kg m−2) to better identify persons with chronic SCI who are obese, and importantly, who are at risk for CVD.
References
Canadian Paraplegic Association 2007 Available at: http://www.canparaplegic.org/en/. Accessed on 17 May 2007.
National Spinal Cord Injury Statistical Center. Spinal cord injury. Facts and figures at a glance. J Spinal Cord Med 2005; 28: 379–380.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: i–xii, 1–253.
Buchholz AC, McGillivray CF, Pencharz PB . The use of bioelectric impedance analysis to measure fluid compartments in subjects with chronic paraplegia. Arch Phys Med Rehabil 2003; 84: 854–861.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN, Waters RL et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol 2003; 95: 2398–2407.
Jones LM, Legge M, Goulding A . Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 1068–1071.
Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G . Body composition assessment in spinal cord injury subjects. Acta Diabetol 2003; 40(Suppl 1): S183–S186.
Lohman T, Going S . Assessment of body composition and energy balance. In: Lamb D, Murray R (eds). Perspectives in Exercise Science and Sports Medicine. Cooper Publishing Group: Caramel, 1998, pp 61–105.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499–511.
Ridker PM, Buring JE, Rifai N, Cook NR . Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA 2007; 297: 611–619.
Martin Ginis KA, Latimer AE, Buchholz AC, Bray SR, Craven BC, Hayes KC et al. Establishing evidence-based physical activity guidelines: methods for the Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI). Spinal Cord 2007; 46: 216–221.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI . Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 1985; 41: 810–817.
Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr 2003; 77: 331–340.
Pace N, Rathburn E . The body water and chemically combined nitrogen content in relation to fat content. J Biol Chem 1945; 158: 685–691.
Cohen J . Statistical Power Analysis for Behavioral Sciences. Lawrence Erlbaum: Hillsdale, NJ, 1988.
Maxwell SE . Sample size and multiple regression analysis. Psychol Methods 2000; 5: 434–458.
George CM, Wells CL, Dugan NL, Hardison R . Hydrostatic weights of patients with spinal injury. Reliability of measurements in standard sit-in and Hubbard tanks. Phys Ther 1987; 67: 921–925.
Gater DRJ . Obesity after spinal cord injury. Phys Med Rehabil Clin N Am 2007; 18: 333–351.
Liang H, Mojtahedi MC, Chen D, Braunschweig CL . Elevated C-reactive protein associated with decreased high-density lipoprotein cholesterol in men with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 36–41.
Finnie AK, Buchholz AC, Martin Ginis KA . Current coronary heart disease risk assessment tools may underestimate risk in community-dwelling persons with chronic spinal cord injury. Spinal Cord 2008; 46: 608–615.
Clasey JL, Gater Jr DR . A comparison of hydrostatic weighing air displacement plethysmography in adults with spinal cord injury. Arch Phys Med Rehabil 2005; 86: 2106–2113.
Acknowledgements
We thank SHAPE SCI participants and Rebecca Bassett and Iwona Chudzik for their help with data collection. We would also like to acknowledge the following contributors: Cathy Craven, Keith C. Hayes, Audrey L Hicks, Amy E Latimer, Mary Ann McColl, Patrick J Potter.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Laughton, G., Buchholz, A., Martin Ginis, K. et al. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord 47, 757–762 (2009). https://doi.org/10.1038/sc.2009.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.33
Keywords
This article is cited by
-
Monitoring outcome measures for cardiometabolic disease during rehabilitation and follow-up in people with spinal cord injury
Spinal Cord (2024)
-
Obesity in wheelchair users with long-standing spinal cord injury: prevalence and associations with time since injury and physical activity
Spinal Cord (2024)
-
Prevalence of an insufficient vitamin D status at the onset of a spinal cord injury – a cross-sectional study
Spinal Cord (2023)
-
An observational study on body mass index during rehabilitation and follow-up in people with spinal cord injury in Denmark
Spinal Cord (2022)
-
Evaluation of cardiovascular disease risk in individuals with chronic spinal cord injury
Spinal Cord (2021)