Abstract
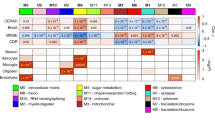
Development of disease-modifying therapies against Alzheimer’s disease (AD) requires biomarkers reflecting the diverse pathological pathways specific for AD. We measured 665 proteins in 797 cerebrospinal fluid (CSF) samples from patients with mild cognitive impairment with abnormal amyloid (MCI(Aβ+): n = 50), AD-dementia (n = 230), non-AD dementias (n = 322) and cognitively unimpaired controls (n = 195) using proximity ligation-based immunoassays. Here we identified >100 CSF proteins dysregulated in MCI(Aβ+) or AD compared to controls or non-AD dementias. Proteins dysregulated in MCI(Aβ+) were primarily related to protein catabolism, energy metabolism and oxidative stress, whereas those specifically dysregulated in AD dementia were related to cell remodeling, vascular function and immune system. Classification modeling unveiled biomarker panels discriminating clinical groups with high accuracies (area under the curve (AUC): 0.85–0.99), which were translated into custom multiplex assays and validated in external and independent cohorts (AUC: 0.8–0.99). Overall, this study provides novel pathophysiological leads delineating the multifactorial nature of AD and potential biomarker tools for diagnostic settings or clinical trials.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available at https://www.synapse.org/PRIDE_AD. MS CSF results from previous studies have been provided by co-authors (J.J.L., N.T.S., E.B.D. and A.I.L.)13,25, and all data are available at https://www.synapse.org/consensus and https://www.synapse.org/#!Synapse:syn20821165/wiki/596086.
Code availability
The code that supports the findings of this study is available from the authors on reasonable request. All models were built using publicly available packages and functions in R.
References
Jellinger, K. A. Neuropathology of dementia disorders.J. Alzheimers Dis. Parkinsonism 4, 135 (2014).
Beach, T. G., Monsell, S. E., Phillips, L. E. & Kukull, W. Accuracy of the clinical diagnosis of Alzheimer disease at National Institute on Aging Alzheimer Disease Centers, 2005–2010. J. Neuropathol. Exp. Neurol. 71, 266–273 (2012).
Gauthier, S. et al. Why has therapy development for dementia failed in the last two decades? Alzheimers Dement. 12, 60–64 (2016).
Jansen, I. E. et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat. Genet. 12, 43 (2019).
van der Kant, R., Goldstein, L. S. B. & Ossenkoppele, R. Amyloid-β-independent regulators of tau pathology in Alzheimer disease. Nat. Rev. Neurosci. 21, 21–35 (2020).
Park, S. A., Han, S. M. & Kim, C. E. New fluid biomarkers tracking non-amyloid-β and non-tau pathology in Alzheimer’s disease. Exp. Mol. Med. 52, 556–568 (2020).
Schoonenboom, N. S. M. et al. Cerebrospinal fluid markers for differential dementia diagnosis in a large memory clinic cohort. Neurology 78, 47–54 (2012).
Jack, C. R. et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14, 535–562 (2018).
Robinson, J. L. et al. Neurodegenerative disease concomitant proteinopathies are prevalent, age-related and APOE4-associated. Brain 141, 2181–2193 (2018).
Ewers, M. et al. CSF biomarkers for the differential diagnosis of Alzheimer’s disease: A large-scale international multicenter study. Alzheimers Dement. 11, 1306–1315 (2015).
van Bokhoven, P. et al. The Alzheimer’s disease drug development landscape. Alzheimers Res. Ther. 13, 186 (2021).
Bader, J. M. et al. Proteome profiling in cerebrospinal fluid reveals novel biomarkers of Alzheimer’s disease. Mol. Syst. Biol. 16, e9356 (2020).
Higginbotham, L. et al. Integrated proteomics reveals brain-based cerebrospinal fluid biomarkers in asymptomatic and symptomatic Alzheimer’s disease. Sci. Adv. 6, eeaz9360 (2020).
Assarsson, E. et al. Homogenous 96-Plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE 9, e95192 (2014).
Enroth, S. et al. High throughput proteomics identifies a high-accuracy 11 plasma protein biomarker signature for ovarian cancer. Commun. Biol. 2, 221 (2019).
Fang, M. et al. The ER UDPase ENTPD5 promotes protein N-glycosylation, the Warburg effect, and proliferation in the PTEN pathway. Cell 143, 711–724 (2010).
Clements, C. M., Mcnally, R. S., Conti, B. J., Mak, T. W. & Ting, J. P. protein, stabilizes the antioxidant transcriptional master regulator Nrf2. Proc. Natl Acad. Sci. USA 103, 15091–15096 (2006).
Maes, M. B. et al. Kinetic investigation of human dipeptidyl peptidase II (DPPII)-mediated hydrolysis of dipeptide derivatives and its identification as quiescent cell proline dipeptidase (QPP)/dipeptidyl peptidase 7 (DPP7). Biochem. J 386, 315–324 (2005).
Soisson, S. M. et al. Structural definition and substrate specificity of the S28 protease family: The crystal structure of human prolylcarboxypeptidase. BMC Struct. Biol. 10, 1–8 (2010).
Patiño-Lopez, G. et al. Human class-I restricted T cell associated molecule is highly expressed in the cerebellum and is a marker for activated NKT and CD8+ T lymphocytes. J. Neuroimmunol. 171, 145–155 (2006).
Derkinderen, P. et al. Tyrosine 394 is phosphorylated in Alzheimer’s paired helical filament tau and in fetal tau with c-Abl as the candidate tyrosine kinase. J. Neurosci. 25, 6584–6593 (2005).
Beroun, A. et al. MMPs in learning and memory and neuropsychiatric disorders. Cell. Mol. Life Sci. 76, 3207–3228 (2019).
Erickson-Viitanen, S., Ruggieri, S., Natalini, P. & Horecker, B. L. Thymosin beta 10, a new analog of thymosin beta 4 in mammalian tissues. Arch. Biochem. Biophys. 225, 407–413 (1983).
Baietti, M. F. et al. Syndecan-syntenin-ALIX regulates the biogenesis of exosomes. Nat. Cell Biol. 14, 677–685 (2012).
Johnson, E. C. B. et al. Large-scale proteomic analysis of Alzheimer’s disease brain and cerebrospinal fluid reveals early changes in energy metabolism associated with microglia and astrocyte activation. Nat. Med. 26, 769–780 (2020).
Isgrò, M. A., Bottoni, P. & Scatena, R. Neuron-Specific enolase as a biomarker: Biochemical and clinical aspects. Adv. Exp. Med. Biol. 867, 125–143 (2015).
Pollio, G. et al. Increased expression of the oligopeptidase THOP1 is a neuroprotective response to Aβ toxicity. Neurobiol. Dis. https://doi.org/10.1016/j.nbd.2008.04.004 (2008).
Dayoub, H. et al. Dimethylarginine dimethylaminohydrolase regulates nitric oxide synthesis: genetic and physiological evidence. Circulation 108, 3042–3047 (2003).
Kannan, L. et al. R-spondin3 prevents mesenteric ischemia/reperfusion-induced tissue damage by tightening endothelium and preventing vascular leakage. Proc. Natl Acad. Sci. USA 110, 14348–14353 (2013).
Wesenhagen, K. E. J., Teunissen, C. E., Visser, P. J. & Tijms, B. M. Cerebrospinal fluid proteomics and biological heterogeneity in Alzheimer’s disease: A literature review. Crit. Rev. Clin. Lab. Sci. 57, 86–98 (2019).
Boström, G. et al. Different inflammatory signatures in Alzheimer’s disease and frontotemporal dementia cerebrospinal fluid. J. Alzheimers Dis. 81, 629–640 (2021).
Konijnenberg, E. et al. APOE ϵ4 genotype-dependent cerebrospinal fluid proteomic signatures in Alzheimer’s disease. Alzheimers Res. Ther. 12, 65 (2020).
Whelan, C. D. et al. Multiplex proteomics identifies novel CSF and plasma biomarkers of early Alzheimer’s disease. Acta Neuropathol. Commun. 7, 169 (2019).
Duits, F. H. et al. Matrix metalloproteinases in Alzheimer’s disease and concurrent cerebral microbleeds. J. Alzheimers Dis. 48, 711–720 (2015).
Dayon, L. et al. Alzheimer disease pathology and the cerebrospinal fluid proteome. Alzheimers Res. Ther. 10, 66 (2018).
Suhre, K., McCarthy, M. I. & Schwenk, J. M. Genetics meets proteomics: perspectives for large population-based studies. Nat. Rev. Genet. 22, 19–37 (2021).
Dammer, E. B. et al. Multi-platform proteomic analysis of Alzheimer’s disease cerebrospinal fluid and plasma reveals network biomarkers associated with proteostasis and the matrisome. Preprint at bioRxiv https://doi.org/10.1101/2022.06.20.494087 (2022).
Wildsmith, K. R. et al. Identification of longitudinally dynamic biomarkers in Alzheimer’s disease cerebrospinal fluid by targeted proteomics. Mol. Neurodegener. 9, 22 (2014).
Begcevic, I. et al. Brain-related proteins as potential CSF biomarkers of Alzheimer’s disease: A targeted mass spectrometry approach. J. Proteomics 182, 12–20 (2018).
Bai, B. et al. Deep multilayer brain proteomics identifies molecular networks in alzheimer’s disease progression. Neuron 105, 975–991 (2020).
Seyfried, N. T. et al. A multi-network approach identifies protein-specific co-expression in asymptomatic and symptomatic Alzheimer’s disease. Cell Syst. 4, 60–72 (2017).
Gao, S., Casey, A. E., Sargeant, T. J. & Mäkinen, V.-P. Genetic variation within endolysosomal system is associated with late-onset Alzheimer’s disease. Brain 141, 2711–2720 (2018).
Butterfield, D. A. & Halliwell, B. Oxidative stress, dysfunctional glucose metabolism and Alzheimer disease. Nat. Rev. Neurosci. 20, 148–160 (2019).
Butkiewicz, M. et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 414–430 (2019).
Lepelletier, F. X., Mann, D. M. A., Robinson, A. C., Pinteaux, E. & Boutin, H. Early changes in extracellular matrix in Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 43, 167–182 (2017).
Wang, H. et al. Regulation of beta-amyloid production in neurons by astrocyte-derived cholesterol. Proc. Natl Acad. Sci. USA 118, e2102191118 (2021).
Philibert, K. D., Marr, R. A., Norstrom, E. M. & Glucksman, M. J. Identification and characterization of Aβ peptide interactors in Alzheimer’s disease by structural approaches. Front. Aging Neurosci. 6, 1–9 (2014).
Lonskaya, I., Hebron, M. L., Desforges, N. M., Franjie, A. & Moussa, C. E.-H. Tyrosine kinase inhibition increases functional parkin‐Beclin‐1 interaction and enhances amyloid clearance and cognitive performance. EMBO Mol. Med. 5, 1247–1262 (2013).
Siddiqui, T. J. et al. An LRRTM4-HSPG complex mediates excitatory synapse development on dentate gyrus granule cells. Neuron 79, 680–695 (2013).
Gong, C.-X., Liu, F. & Iqbal, K. Perspective multifactorial hypothesis and multi-targets for Alzheimer’s disease. J. Alzheimers Dis. 64, 107–117 (2018).
Johnstone, D., Milward, E. A., Berretta, R. & Moscato, P. Multivariate protein signatures of pre-clinical Alzheimer’s disease in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Plasma Proteome Dataset. PLoS ONE 7, e34341 (2012).
Kim, Y. et al. Targeted proteomics identifies liquid-biopsy signatures for extracapsular prostate cancer. Nat. Commun. 7, 11906 (2016).
Teunissen, C. E., Otto, M., Engelborghs, S., Herukka, S.-K. & Lehmann, S. White paper by the Society for CSF Analysis and Clinical Neurochemistry: Overcoming barriers in biomarker development and clinical translation. Alzheimers Res. Ther. 12, 23 (2018).
Teunissen, C. E. et al. Novel diagnostic cerebrospinal fluid protein biomarkers for pathologic subtypes of frontotemporal dementia identified by proteomics. Alzheimers Dement. 9, 86–94 (2016).
Teunissen, C. E. et al. Blood-based biomarkers for Alzheimer’s disease: Towards clinical implementation. Lancet Neurol. 21, 66–77 (2021).
van der Flier, W. M. & Scheltens, P. Amsterdam Dementia Cohort: Performing research to optimize care. J. Alzheimers Dis. 62, 1091–1111 (2018).
Lleó, A. et al. A 2-step cerebrospinal algorithm for the selection of frontotemporal lobar degeneration subtypes. JAMA Neurol. 75, 738–745 (2018).
Del Campo, M. et al. Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: An update. Biomark Med. 6, 419–430 (2012).
Albert, M. S. et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 270–279 (2011).
Dubois, B. et al. Research criteria for the diagnosis of Alzheimer’s disease: Revising the NINCDS-ADRDA criteria. Lancet Neurol. 6, 734–746 (2007).
McKeith, I. G. et al. Diagnosis and management of dementia with Lewy bodies: Third report of the DLB Consortium. Neurology 65, 1863–1872 (2005).
McKeith, I. G. et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 89, 88–100 (2017).
Rascovsky, K. et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134, 2456–2477 (2011).
Armstrong, M. J. et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 80, 496–503 (2013).
Litvan, I. et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 47, 1–9 (1996).
Shaw, L. M. et al. Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann. Neurol. 65, 403–413 (2009).
Duits, F. H. et al. The cerebrospinal fluid ‘alzheimer profile’: Easily said, but what does it mean? Alzheimers Dement. 10, 713–723 (2014).
Alcolea, D. et al. The Sant Pau Initiative on Neurodegeneration (SPIN) cohort: A data set for biomarker discovery and validation in neurodegenerative disorders. Alzheimers Dement. 5, 597–609 (2019).
Tijms, B. M. et al. Unbiased approach to counteract upward drift in cerebrospinal fluid amyloid-β 1–42 analysis results. Clin. Chem. 64, 576–585 (2018).
Jessen, F. et al. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement. 10, 844–852 (2014).
Leeuw, F. A. et al. Blood‐based metabolic signatures in Alzheimer’s disease. Alzheimers Dement. 8, 196–207 (2017).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33, 1–22 (2010).
Acknowledgements
This research is part of the neurodegeneration research program of Amsterdam Neuroscience. This study was supported by Alzheimer Nederland (WE.03-2018-05, M.d.C. and C.E.T.) and Selfridges Group Foundation (NR170065, M.d.C. and C.E.T.). M.d.C. and G.H. are supported by the attraction talent fellowship of Comunidad de Madrid (2018-T2/BMD-11885) and San Pablo CEU University. D.A. acknowledges support from Institute of Health Carlos III (PI18/00435, INT19/00016) and the Department of Health Generalitat de Catalunya PERIS program (SLT006/17/125). Collection of patients samples and data from Penn University (A.C.-P. and D.J.I.) was supported by different funding sources, including National Institute on Aging NINDS R01-NS109260-01A1, P01-AG066597, P30-AG072979 (formerly P30-AG10124) and U19-AG062418-03 (formerly NINDSP50-NS053488-09). Alzheimer Center Amsterdam is supported by Stichting Alzheimer Nederland and Stichting VUmc fonds. The chair (W.M.v.d.F.) is supported by the Pasman stichting. The clinical database structure was developed with funding from Stichting Dioraphte. Research programs of W.M.v.d.F. have been funded by ZonMW, NWO, EU-FP7, EU-JPND, Alzheimer Nederland, Hersenstichting CardioVascular Onderzoek Nederland, Health~Holland, Topsector Life Sciences & Health, stichting Dioraphte, Gieskes-Strijbisfonds, stichting Equilibrio, Edwin Bouw fonds, Pasman stichting, stichting Alzheimer & Neuropsychiatrie Foundation, Philips, Biogen MA, Novartis-NL, Life-MI, AVID, Roche BV, Fujifilm and Combinostics. W.M.v.d.F. holds the Pasman chair. W.M.v.d.F. is a recipient of ABOARD, which is a public-private partnership receiving funding from ZonMW (73305095007) and Health~Holland, Topsector Life Sciences & Health (PPP-allowance; #LSHM20106). All funding is paid to her institution. Research of C.E.T. is supported by the European Commission (Marie Curie International Training Network, grant agreement No. 860197 (MIRIADE)), Innovative Medicines Initiatives 3TR (Horizon 2020, grant 831434), EPND (IMI 2 Joint Undertaking (JU) under grant agreement 101034344) and JPND (bPRIDE), National MS Society (Progressive MS alliance) and Health Holland, the Dutch Research Council (ZonMW), Alzheimer Drug Discovery Foundation, The Selfridges Group Foundation, Alzheimer Netherlands and Alzheimer Association. C.E.T. is a recipient of ABOARD, which is a public-private partnership receiving funding from ZonMW (3305095007) and Health~Holland, Topsector Life Sciences & Health (PPP allowance; LSHM20106). ABOARD also receives funding from Edwin Bouw Fonds and Gieskes-Strijbisfonds. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
M.d.C. and C.T conceived the study. M.d.C., C.F.W.P., L.V. and M.v.N. performed the statistical analysis. L.V., A.C.-P., D.J.I., W.T.H., L.H.M., J.v.S., D.A., A.L., A.W.L, Y.A.L.P., P.J.V., B.T.M. and W.M.v.d.F. recruited participants and collected clinical data and samples. M.d.C. and Y.S.H. arranged and prepared samples for proteomics analysis. J.J.L., N.T.S., E.B.D. and A.I.L. provided the proteomic data (both Olink and MS) from previous published studies13,25. M.d.C. and C.E.T. drafted the manuscript. All authors contributed to revision and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.d.C. has been an invited speaker at Eisai. L.V. received a grant for the CORAL consortium by Olink. B.M.T. and P.J.V. are inventors on a patent (WO2020197399A1; owned by Stichting VUmc). D.J.I. is a Scientific Advisory Board Member for Denali Therapeutics. D.A. participated in advisory boards from Fujirebio-Europe and Roche Diagnostics and received speaker honoraria from Fujirebio-Europe, Roche Diagnostics, Nutricia, Krka Farmacéutica S.L., Zambon S.A.U. and Esteve Pharmaceuticals S.A. D.A. declares a filed patent application (WO2019175379 A1 Markers of synaptopathy in neurodegenerative disease). W.M.v.d.F. has performed contract research for Biogen MA and Boehringer Ingelheim. W.M.v.d.F. has been an invited speaker at Boehringer Ingelheim, Biogen MA, Danone, Eisai, WebMD Neurology (Medscape) and Springer Healthcare. W.M.v.d.F. is consultant to Oxford Health Policy Forum CIC, Roche and Biogen MA. W.M.v.d.F. participated in advisory boards of Biogen MA and Roche. All funding is paid to her institution. W.M.v.d.F. is member of the steering committee of PAVE and Think Brain Health. W.M.v.d.F. was associate editor of Alzheimer’s Research & Therapy in 2020/2021. W.M.v.d.F. is associate editor at Brain. C.E.T. has a collaboration contract with ADx Neurosciences, Quanterix and Eli Lilly and performed contract research or received grants from AC-Immune, Axon Neurosciences, Bioconnect, Bioorchestra, Brainstorm Therapeutics, Celgene, EIP Pharma, Eisai, Grifols, Novo Nordisk, PeopleBio, Roche, Toyama and Vivoryon. She serves on editorial boards of Medidact Neurologie/Springer, Alzheimer’s Research & Therapy and Neurology: Neuroimmunology & Neuroinflammation and is editor of a Neuromethods book (Springer). She had speaker contracts for Roche, Grifols and Novo Nordisk. The other authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Niklas Mattsson-Carlgren and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Protein replicates measured through different PEA panels showed comparable differences.
a, Beta coefficients (log2 fold change) of the protein replicates from the comparisons between MCI(Aβ+) or AD and controls (yellow and red respectively) and AD and non-AD dementias (blue). Stars represent the corresponding significant q-value (* q < 0.05, ** q < 0.01, ***q < 0.001) in the discrimination between groups. b, Scatter plots show the correlation of the NPX values (protein abundance) between the protein replicates that showed significant differences across the groups of interest in the complete cohort (n = 797). Regression line and 95% confident intervals are depicted. Insert indicate the spearman correlation coefficient. CON, cognitively unimpaired controls; MCI(Aβ+), mild cognitive impairment with Aβ pathological changes; AD, Alzheimer’s disease; non-AD dem: non-AD dementias.
Extended Data Fig. 2 Sensitivity analysis AD versus control.
a, Volcano plot represent the proteins differentially regulated in the validation cohort (AD = 18, CON = 44)23,24 after two-sided nested F-test analysis with no adjustments for multiple comparisons. The beta coefficients (log2 fold change) are plotted versus p values (-log10-transformed). Scatter plots show the correlation between the p-values or beta coefficients obtained in the discovery and validation cohorts. Insert indicate the spearman correlation coefficient using all proteins. Proteins showing concordance between discovery and validation (that is, consistency regarding the proteins that are dysregulated and nondysregulated or show the same direction of changes between the groups of interest in both cohorts) are colored in green and the corresponding concordance % is indicated. b, Venn diagram depicts the number and % of overlapping proteins that are significantly dysregulated (p < 0.05) between AD and controls in the discovery and validation cohorts after applying two-sided nested F-test analysis with no adjustments for multiple comparisons. The name of the overlapping proteins is specified in extended data Table 1. AD, Alzheimer’s disease; CON, cognitively unimpaired controls.
Extended Data Fig. 3 Biological processes enriched with randomly selected markers.
Bar graphs depicting the biological pathways enriched when a random selection of markers was performed. The number of proteins randomly selected is the same as those in the unique protein subsets identified along AD stages (Fig. 2b). Functional enrichment was performed using Metascape selecting GO Biological Processes as ontology source. Terms with a p-value < 0.01, a minimum count of 3, and an enrichment factor > 1.5 were collected and grouped into clusters based on their membership similarities. p-values were calculated based on the accumulative hypergeometric distribution. Kappa scores are used as the similarity metric when performing hierarchical clustering on the enriched terms, and subtrees with a similarity of > 0.3 are considered a cluster. The most statistically significant term within a cluster is chosen to represent the cluster. The corresponding GO number and biological process is defined in the right side. Stronger colors represent higher significant enrichment. Vertical line represent the significant threshold (unadjusted p < 0.01).
Extended Data Fig. 4 Mean intensity values of the protein markers included in the CSF diagnostic protein panels for early and specific diagnosis of AD.
Violins represent the abundance (log2 NPX) of the CSF proteins that combined can accurately discriminate MCI(Aβ+) (n = 50) or AD (n = 230, orange) from controls (n = 195) and AD from other types of dementias (n = 322, blue). Horizontal black and dash lines indicate median and interquartile range of the protein abundance. aITGB2 and ABL1 are also markers within the AD versus non-AD dementia panel.*q < 0.05, **q < 0.01, ***q < 0.001. n.s: non-significant. MCI(Aβ+), mild cognitive impairment with Aβ pathological changes; AD, Alzheimer’s disease; non-ADdem: non-AD dementias; CON, cognitively unimpaired controls.
Extended Data Fig. 5 Correlations between each biomarker panel composite score and AD CSF biomarkers and cognitive function.
Correlation matrix heatmaps represent the Spearman’s correlation coefficient in-between the biomarker panel composite score (PC) of each of the identified CSF panels, the classical AD CSF biomarkers (Aβ42, tTau, pTau181 and tTau/Aβ42 ratio) and MMSE score in the corresponding groups for which the specific panel was built. Positive correlations are depicted in red; negative correlations are depicted in blue. Correlation coefficients are indicated. AD, Alzheimer’s disease; non-AD dem: non-AD dementias; CON, cognitively unimpaired controls.
Extended Data Fig. 6 Additional sensitivity analysis for the CSF biomarker panels discriminating AD from controls or AD from non-AD dementias.
a, Receiver operating characteristic (ROC) curves showed that the performance of the CSF AD-diagnostic to discriminate AD from controls was similar between APOE4 + (AD = 133; CON = 44) and APOE4- (AD = 88; CON = 125) patients. b, ROC curve depicting the performance of the CSF AD-differential diagnostic discriminating AD from non-AD dementias in the subset of patients in which non-AD dementias was confirmed (AD = 230; cNon-AD dem = 101). Black line is the mean area under the curve (AUC) over all resamplings (1000 repeats of 5-fold cross-validation, gray lines). Inserts outline corresponding AUC and 95% CI. AD, Alzheimer’s disease; CON, cognitively unimpaired controls; cNon-Ad dem: confirmed non-AD dementias.
Extended Data Fig. 7 Performance of CSF biomarker panels discriminating other groups of interest.
Receiver operating characteristic (ROC) curves depicting the performance of the different panels (rows, Fig. 3, Table 2) discriminating other groups of interest (columns). Black line is the mean area under the curve (AUC) over all resamplings (1000 repeats of 5-fold cross-validation, gray lines). Inserts outline corresponding AUC and 95% CI. MCI(Aβ+), mild cognitive impairment with Aβ pathological changes; AD, Alzheimer’s disease; non-AD dem: non-AD dementias; CON, cognitively unimpaired controls.
Extended Data Fig. 8 CSF biomarker panel for MCI(Aβ+) was not fully replicated in the validation cohort using custom PEA assays.
a, Receiver operating characteristic (ROC) curve depicting the performance of CSF biomarker panel discriminating MCI(Aβ+) from controls (10 CSF proteins: ENTPD5, CRTAM, PARK7, DPP7, CLEC5A, CYR61, KYNU, PCSK9, DDAH1 and PRCP) in the discovery (a, CON = 195, MCI(Aβ+) = 50). Black line is the mean area under the curve (AUC) over all resamplings (1000 repeats of 5-fold cross-validation, gray lines). Inserts outline corresponding AUC and 95% CI. b) ROC curve depicting the performance of CSF MCI(Aβ+)-diagnostic panel in the validation cohort (CON = 110 and MCI(Aβ+) = 101) using the custom assays. CRTAM assay could not be developed due to technical difficulties and thus was not included in the analysis of the validation cohort. c) Scatter plots show the correlation between the beta-coefficients obtained in the discovery phase to those obtained with the custom assays in validation step 2. Insert indicate the spearman correlation coefficient.*ABL1 and ITGB2 are proteins that are present in both AD CSF panels. CLEC5A is present in both the AD and the MCI(Aβ+) diagnostic panel. MCI(Aβ+), mild cognitive impairment with Aβ pathological changes; AD, Alzheimer’s disease; non-AD dem: non-AD dementias; CON, cognitively unimpaired controls.
Supplementary information
Source data
Source Data Table 1
Table outlining the statistics of the CSF proteins differentially regulated across the different diagnostic groups
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
del Campo, M., Peeters, C.F.W., Johnson, E.C.B. et al. CSF proteome profiling across the Alzheimer’s disease spectrum reflects the multifactorial nature of the disease and identifies specific biomarker panels. Nat Aging 2, 1040–1053 (2022). https://doi.org/10.1038/s43587-022-00300-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-022-00300-1