Abstract
In-vivo corneal confocal microscopy is a powerful imaging technique which provides clinicians and researcher with the capabilities to observe microstructures at the ocular surfaces in significant detail. In this Mini Review, the optics and image analysis methods with the use of corneal confocal microscopy are discussed. While novel insights of neuroanatomy and biology of the eyes, particularly the ocular surface, have been provided by corneal confocal microscopy, some debatable elements observed using this technique remain and these are explored in this Mini Review. Potential improvements in imaging methodology and instrumentation are also suggested.
Similar content being viewed by others
Introduction
The ocular surface is richly innervated with sensory nerves, particularly at the cornea which is a clear dome-like tissue forming the frontmost part of the eye. In-vivo corneal confocal microscopy is a technique which is capable of imaging corneal microstructures at different depths of the tissue. Together with immunohistochemical techniques, it has provided insight into biological functions of different neuronal and immunological constituents of the cornea. The sub-basal nerve plexus has garnered substantial interest as it is the densest and most homogenous of the several nerve plexi in the cornea, situated between the basal epithelial layer and Bowman’s layer1. Corneal confocal microscopy has provided an opportunity to image corneal microstructures non-invasively and monitor how these change overtime with exposure to various stimuli. This Mini Review summarises current iterations of corneal confocal microscopy instrumentation with particular focus on laser scanning confocal microscopy which is the most widely used form. In addition to the optics of confocal microscopy and image analysis, this Mini Review also explores the anatomical, neurobiological and immunological insights afforded by corneal confocal microscopy as well as the pervasive gaps in our knowledge. Limitations and future directions in the advancement of the corneal confocal microscopy technique will also be explored (Box 1).
Emergence and optics of confocal microscopy
Ocular imaging techniques have advanced and improved over the past few decades, with in-vivo confocal microscopy emerging as a potential diagnostic technique for ocular surface diseases due to its ability to observe ocular surface microstructures in a non-invasive and rapid manner. This imaging technique is based on the principle of confocal microscopy first described in 19552. Compared to conventional light microscopy, confocal microscopy produces images with higher resolution and better out-of-focus information rejection. It is also able to capture images of cellular layers from various depths within a thick tissue specimen using its optical sectioning capability and hence, is well suited for the investigation of intact tissue in living organisms.
The optical sectioning property of the confocal microscope makes it possible to store a three-dimensional data set of intensity values of thick objects by using a point source and a point detector in the illumination and detection paths, respectively3. The sample is illuminated using a diffraction-limited focused laser spot and the reflected or transmitted light is detected by a point-like detector (Fig. 1). When light comes from the focal region of a specimen, it is focussed onto a point detector (Fig. 1a) and hence produces a strong signal. However, light which comes from a region away from the focal plane (say z1) is defocused at the pinhole (Fig. 1b) and therefore produces a much weaker signal. In terms of the resolution of the image, a narrower axial response width implies a higher axial resolution. In other words, the narrower the peak in the V(z) profile, the better the system is at distinguishing between objects located at different axial positions (Fig. 1c). This unique system contributes to the powerful imaging capabilities of the in-vivo corneal confocal microscope in producing images of high resolution and magnification.
Schematic diagram of a confocal microscope illustrates the optical section property (a) when the sample is placed at the correct image distance (z), the reflected light is focussed on to the point detector, and (b) when the sample lies at some other image distance (z1), the reflected light focuses above or below the plane of the point of detection. c The V(z) profile represents the axial resolution of a confocal system. A narrower axial response width indicates a higher axial resolution.
Confocal imaging of the ocular surface
There are three types of commercially available in-vivo confocal microscopy developed for assessing the ocular surface: the Tandem Scanning Confocal Microscope (Tandem Scanning Corp, Virginia, USA), the Confoscan 4 (Nidek Technologies Srl, Padova, Italy), and the Heidelberg Retinal Tomograph with Rostock Corneal Module (HRT-RCM, Heidelberg Engineering, GmBH, Dossenheim, Germany). These microscopes differ from one another in terms of the intensity of the light source, magnification, image contrast, and image resolution. However, the HRT-RCM which uses a laser scanning confocal microscope provides higher resolution and magnification compared to earlier corneal confocal microscopy models4, and is currently more widely used by clinicians and researchers worldwide.
While confocal microscopy is capable of imaging various regions of the ocular surface, it has been more widely used to characterise features of the cornea. Corneal epithelial cells, stromal keratocytes and endothelial cells can be imaged at high resolution which enable assessment of their integrity and shape. Cell densities, including resident immune cells, can also be monitored using corneal confocal microscopy5,6.
Nerve fibres innervating the cornea form several plexi within anterior layers of the cornea, from the stroma to the epithelium. As the sub-basal nerve plexus is the densest and most homogenous of these nerve plexi, it has been widely studied particularly in ocular surface diseases. Currently, quantifying parameters such as corneal nerve fibre length or density are normally conducted using software which could include manual tracing or methods such as CCMetrics7, and semi-automated tracing such as NeuronJ, a plugin in ImageJ (National Institutes of Health, Maryland, USA). Automated procedures have also been proposed to substantially reduce the time needed to analyse corneal nerve parameters, although studies have shown that conventional automated procedures may underestimate these parameters compared to manual or semi-automated procedures8,9. The following section outlines further advancements in the analysis of corneal nerve parameters particularly with artificial intelligence (AI).
Image analysis
Advances in AI have encouraged clinical neuroscience towards more objective systems for quantifying corneal nerve morphology from corneal confocal microscopy images10,11,12. Automation provides clinicians with diagnostic leverage for inferring disease from measurable image structure using computational models developed in software. Two of the most popular geometric attributes that have been modelled using AI previously include nerve density or length and tortuosity of the sub-basal nerve plexus.
Nerve density is commonly defined as the standardised distribution of nerve fibres over a finite area of image space in mm/mm2 or the ‘sum of the nerve branches observed within a frame’13. Models that automatically estimate nerve density require images of corneal nerve fibres to be fully segmented. Any model fragmentation generated by false negatives would lead to underestimates of nerve density.
Scarpa et al.12 used simple convolutional Gabor kernel filters in conjunction with image equalisation to enhance the nerve contours in corneal confocal microscopy images to improve nerve segmentation. They found the estimates of segmented nerve length from their model were correlated with the lengths of subjectively identified nerve contours, accounting for around 74% to 88% of subjective judgments of nerve length. Another recent approach used a multiscale dual-model approach that applied even-symmetric Gabor filters to the image in one step to then enhance contours and a background noise reduction operation in an alternate step14. Even symmetric Gabor filters model the behaviour of simple cells found in the primary visual cortex and thus model subjective gradings of corneal nerves. The success of this approach has been improved with the support of artificial neural networks15 and has been leveraged upon by end-user software packages like ACCMetrics16.
Kim and Markoulli17 devised a ‘structure enhancement’ model based on multiscale spatial Gabor filters and operations to eliminate vignetting of corneal confocal microscopy images. Although this approach is simple and principled in modelling human visual detection of image contours, it does not outperform ACCMetrics17. However, another recent proposal used U-Net convolutional neural networks to perform corneal nerve segmentation from corneal confocal microscopy images18. The sensitivity of their model performed at the level expected of human subjective graders, which has proved useful for segmenting corneal nerve contours in corneal confocal microscopy images to estimate nerve density. While deep learning algorithms continue to evolve and be developed to enhance nerve segmentation and evaluation, most are limited to research settings and require further validation before implementation in clinical practice19,20. A software using a customised deep learning-based approach known as deepNerve has recently been developed and used for animal and clinical human studies21,22, demonstrating the promising potential of artificial intelligence in this area.
In comparison to nerve density, nerve tortuosity is not as well defined. Oliveira‐Soto and Efron13 proposed a grading system whereby a score of zero indicates nerve contours appear straight and a score of four indicates nerve contours frequently and largely change orientation across their length. A potential limitation of this definition is there is no clear guide on what an extreme example of tortuosity should look like and how intermediate levels perceptually scale. However, the advent of machine learning provides the ability to ‘inversely’ determine the image-based parameters that predict human observer gradings.
Using a generative model design, ref. 10 proposed a reliable automated model of tortuosity that was motivated by the need to account for the overall magnitude of changes in nerve orientation across the image and number of local ‘twists’—denoted by the number of inflection points along a segmented nerve fibre’s length. An alternative approach used Multinomial logistic ordinal regression to show that mean curvature at two different spatial scales was diagnostic of human subjective tortuosity gradings23. However, a more recent study by ref. 24 proposed that nerve tortuosity was best quantified directly using U-Net segmentation to assess adjacent angular detection of nerve contour orientations (USAAD). This model first obtains a local-scale index of tortuosity by determining the straight-line contours that connect every adjacent pair of nerve pixels segmented using the earlier-described U-Net segmentation algorithm. Reducing the number of key points allows the model to assess tortuosity over longer spatial ranges. This model was found to generate outstanding performance in accounting for subjective ratings. Evidence also suggested that subjective ratings of tortuosity is computed across multiple scales spanning the full range of nerve lengths available. Could this mean that tortuosity estimates are weighted towards longer nerves when they are visible? Consistent with this view, a simple model that weighted tortuosity estimates based on nerve fibre length was found to exhibit sound correspondence with human judgements of tortuosity and provided diagnostic leverage in the prediction of diabetes11.
In summary, there appears to be great benefit achieved thus far through image analysis techniques developed in previous literature. One potential limitation of these approaches is that ground truth is consistently referenced to subjective gradings made by human observers. However, this may not be a limitation as the end goal of AI is to optimally assist clinicians with their diagnostic and monitoring responsibilities, but not replace them.
Neurobiological and immunological insights
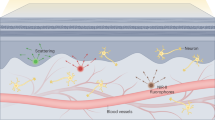
Neural and immunological features are the two main components investigated using corneal confocal microscopy. As mentioned, the sub-basal nerve plexus is the one of the most studied part of the cornea given its uniform and dense nerve fibre distribution1. Both corneal confocal microscopy and immunohistochemical techniques have demonstrated distinct morphological patterns in this plexus, with some of the earlier montaged corneal confocal microscopy images showing nerve fibres converging towards a clockwise or anti-clockwise spiral25. This region has been termed the inferior whorl which is situated about 1–2 mm inferonasal from the anatomical centre of the cornea. While various theories have been suggested for the spiral pattern of the sub-basal nerve plexus, recent studies have shown that interactions with corneal epithelial cells also migrating from limbal regions have substantial impact on dictating the course of nerve fibre migration26,27. Specifically, axon guidance ligands have been found on corneal epithelial cells including Semaphorins, Ephrins and Netrins28. Various studies have also indicated the potential for the inferior whorl to act as a landmark for monitoring neuronal changes particularly in peripheral neuropathic conditions29,30. However, there has been evidence of deviations from this spiral pattern associated with advancing age31 or neuronal damage32 which may confound identification of the inferior whorl region. While laser scanning confocal microscopy can provide substantial detail of corneal microstructures in high resolution and magnification, one of its limitations is the small field of view associated with each image frame which constitutes an area of 0.16 mm2. In relation to quantitative sub-basal nerve plexus outcomes including corneal nerve parameters and dendritic cell density, various studies have shown that random sampling of a selected number of images (usually 8 or more) from a total pool collected from areas of interest of the cornea may be sufficient in optimising reproducibility and accuracy of measures32,33,34. Widefield imaging capabilities could further facilitate analysis of nerve migration35,36 and monitor neuronal morphological changes in the sub-basal nerve plexus.
Certain resident immune cells can also be imaged within the cornea through corneal confocal microscopy. This has been supported by earlier findings which identified the presence of bone marrow-derived CD11c+ dendritic cells which are potent antigen presenting cells located mainly within the epithelial and anterior stromal layer of the cornea, as well as macrophages in the stroma37. Plasmacytoid dendritic cells, a subpopulation of bone marrow-derived dendritic cells, have also been shown to be present particularly in the peripheral regions with pivotal roles in inducing immune tolerance38 or wound healing39. While corneal confocal microscopy lacks the capability of providing functional characterisation of immune cells, researchers have used its high resolution and magnification to analyse morphological properties particularly with dendritic cells. Generally, dendritic cells with larger size and/or more dendrites are characterised as activated or mature40,41, indicating a more inflamed state in the cornea.
The biological interconnectedness between both eyes can also be demonstrated through the cornea. Recent studies using corneal confocal microscopy to investigate corneal infections including herpetic keratitis or cataract surgery in one eye have shown bilateral reduction in corneal nerves in both eyes42,43,44. Experimentally-induced corneal nerve cut or injury to one eye in animal studies have also affected corneal nerve function45 and increased CD11c+ or CD11b+ dendritic cells expressing co-stimulatory molecules in the unaffected eye46. Such interdependence between the two ocular surfaces may partly be due to a neurogenic inflammatory reflex mediated by activation of the transient receptor potential vanilloid 1 channel involved in nociceptive signalling and subsequent substance P release47. A corneal-trigeminal axis involving upregulation proinflammatory cytokines, substance P and infiltration of immune cells may also contribute to the propagation of inflammation from the affected corneal surface to bilateral trigeminal ganglia48.
Prevailing uncertainties in the identification of corneal microstructures
While corneal confocal microscopy has provided substantial information of anatomical structures and biological function in the cornea, certain gaps in knowledge remains pervasive. corneal confocal microscopy has been used to monitor corneal nerve recovery following therapeutic or surgical interventions in various ocular surface diseases49,50, but it is also thought to be able to detect signs of aberrant regeneration. Microneuromas are another neuronal feature that has been identified with corneal confocal microscopy and commonly described as terminal enlargements of a corneal nerve51,52. It is thought that these enlargements are associated with aberrant nerve regeneration and neuropathic pain following injury to the corneal nerve53. While severed nerves have historically demonstrated these abnormal neuronal growths54, recent studies have shown that some features previously identified as microneuromas with corneal confocal microscopy could potentially be corneal nerve stromal-epithelial nerve penetration sites55. The latter could be characterised as being diffuse hyperreflective sites as supported by immunohistochemical findings showing continuation between the sub-basal corneal nerve and underlying originating stromal nerve55. Emerging evidence from murine models demonstrated that the presence of these penetration sites may be elevated with metabolic stress or dysfunction56. However, standardisation in the identification of these neuronal features is still required.
Hyperreflective round cells have also been identified amongst the sub-basal nerve plexus particularly at the inferior whorl region. As their size and hyperreflectivity seem to reflect those of dendritic cells, they are considered to be a subtype of immune cells which lack dendrites. These cells have been given different labels including globular cells57, dot-like features31 or round-shaped immune cells58. The evidence for the true nature and biological significance of these cells remain limited with little knowledge of immunohistochemical correlates. However, CD86+ round-shaped dendritic cells closely associated with sub-basal nerve fibre branching points have been observed by ref. 59. These cells penetrate the basement membrane into the stroma and may play a role in guiding nerve movement or trajectory59. Whether these cells represent those observed in corneal confocal microscopy remain unknown.
Cells with dendritiform morphology are often labelled as dendritic cells in studies using corneal confocal microscopy. A recent study identified the presence of resident CD8+ memory T-cells in constant motility following a resolution of local infection which also demonstrated dendritic morphology using immunostaining techniques60. Highly motile dendritiform cells were also observed with corneal confocal microscopy in humans by constructing single images of the same area imaged by corneal confocal microscopy in a time series60. These are reminiscent of ‘immature’ dendritic cells labelled in previous studies61,62, however whether corneal confocal microscopy can distinguish these immune cell types based on morphology alone requires further investigation. It is evident that more widefield in-vivo corneal imaging techniques which can also localise corneal nerve regions to be imaged could facilitate more thorough comparisons and precise monitoring of these corneal microfeatures.
Current clinical and research applications
In specialty clinics for corneal disease, corneal confocal microscopy has demonstrated high discriminative ability in distinguishing infectious keratitis of various aetiologies. It is particularly useful in cases with atypical clinical presentations where differentiation is more difficult such as the visualisation of fungal filaments and acanthamoeba trophozoites or cysts to confirm an uncertain diagnosis63,64,65,66. Recent findings in corneal confocal microscopy have also been associated with systemic biological health such as higher corneal nerve parameters with higher serum levels of omega-3 polyunsaturated fatty acids particularly docosahexanoic acid67 and associations between reduced corneal nerve parameters in Alzheimer’s disease or transgenic mice overexpressing human non-mutated tau68. Corneal confocal microscopy has mostly been studied in the context of diabetes, which is one of the most common causes of peripheral nerve injury in the distal extremities particularly the feet69. Its utility in diagnosing and predicting the development of diabetic peripheral neuropathy has been demonstrated in previous studies70,71,72 (Fig. 2). Loss of corneal nerves and increase in corneal dendritic cells were found to be more prominent in affected patients73,74. Similar changes have been observed in ocular surface conditions particularly in dry eye disease75 which is known to have elements of neurological and inflammatory dysfunction76.
Note that the nerve density is the least in the T1DPN+ images, followed by the T1DPN– and then healthy controls. The figure was reprinted from Tummanapalli et al. with permission from Elsevier72.
Future outlook
Several improvements could be made to enhance imaging capabilities of the corneal confocal microscopy, a few of which have been discussed in previous sections of this Mini Review. The most commonly used methodology in clinical research settings involves random selection of a set number of images with sufficient quality from a pool of images obtained from a participant’s eye prior to analysis33,34. Sampling strategy of adequate images has been shown to produce sufficient accuracy, however for longitudinal or clinical monitoring purposes, real-time widefield imaging capabilities may provide more insight into regional changes in the cornea over time or following exposure to various stimuli77,78. In fact, a minimum repeatable area of 1.5 mm2 is shown to have reliable morphological characterisation of the sub-basal nerve plexus79,80.
Precise and repeatable localisation technology built into corneal confocal microscopy instrumentation, akin to those available in optical coherence tomography (OCT) to facilitate follow-up assessments of the posterior pole, is yet to be devised for routine clinical use. More recently, OCT technology with real-time eye tracking has been adapted to provide non-contact visualisation of corneal nerves81, as well as other ocular surface structures in a larger field of view including tear film patterns, limbal crypts and conjunctival vasculature82,83. However, these techniques are yet to be adopted for widespread use and the inherent curvature and clarity of the cornea continue to present a challenge in widefield imaging. Volumetric scans may also shed more light on 3-dimensional structures particularly in terms of the physical interactions between neuronal, epithelial and immune elements. This may further inform the concept of peripheral epineuroimmune interactome which characterises the biological interdependence of these microstructures essential for the maintenance of health84. In order to enhance patient- and clinician-friendliness, non-contact procedures would also be desirable to prevent deterrence of patients who may be more sensitive to mechanical sensations85. AI is also increasingly utilised to further improve the sophistication of corneal nerve20,86,87,88 or immune cell segmentation and detection20,89. These advancements may improve the applicability of corneal confocal microscopy and also improve efficiency in observing corneal microstructures to achieve the aim of understanding their biological significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
References
Marfurt, C. F., Cox, J., Deek, S. & Dvorscak, L. Anatomy of the human corneal innervation. Exp. Eye Res. 90, 478–492 (2010).
Minsky, M. Memoir on inventing the confocal scanning microscope. Scanning 10, 128–138 (1988).
Sheppard, C. J. R., Hamilton, D. K., Cox, I. J. & Cullen, A. L. Optical microscopy with extended depth of field. Proc. R. Soc. Lond. A 387, 171–186 (1997).
Chirapapaisan, C., Thongsuwan, S., Chirapapaisan, N., Chonpimai, P. & Veeraburinon, A. Characteristics of corneal subbasal nerves in different age groups: an in vivo confocal microscopic analysis. Clin. Ophthalmol. 15, 3563–3572 (2021).
Misra, S. L., Goh, Y. W., Patel, D. V., Riley, A. F. & McGhee, C. N. J. Corneal microstructural changes in nerve fiber, endothelial and epithelial density after cataract surgery in patients with diabetes mellitus. Cornea 34, 177–181 (2015).
Alotaibi, S., Ozkan, J., Papas, E. & Markoulli, M. Diurnal variation of corneal dendritic cell density. Curr. Eye Res. 47, 1239–1245 (2022).
Petropoulos, I. N. et al. Repeatability of in vivo corneal confocal microscopy to quantify corneal nerve morphology. Cornea 32, e83–e89 (2013).
Zhang, Y., Wu, Y., Li, W. & Huang, X. Semiautomated and automated quantitative analysis of corneal sub-basal nerves in patients with DED with ocular pain using IVCM. Front. Med. 9, 831307 (2022).
Dehghani, C. et al. Fully automated, semiautomated, and manual morphometric analysis of corneal subbasal nerve plexus in individuals with and without diabetes. Cornea 33, 696–702 (2014).
Scarpa, F., Zheng, X., Ohashi, Y. & Ruggeri, A. Automatic evaluation of corneal nerve tortuosity in images from in vivo confocal microscopy. Investig. Ophthalmol. Vis. Sci. 52, 6404–6408 (2011). %J Investigative Ophthalmology & Visual Science.
Klisser, J. et al. Automated analysis of corneal nerve tortuosity in diabetes: Implications for neuropathy detection. Clin. Exp. Optom. 105, 487–493 (2022).
Scarpa, F., Grisan, E. & Ruggeri, A. Automatic recognition of corneal nerve structures in images from confocal microscopy. Investig. Ophthalmol. Vis. Sci. 49, 4801–4807 (2008).
Oliveira-Soto, L. & Efron, N. Morphology of corneal nerves using confocal microscopy. Cornea 20, 374–384 (2001).
Dabbah, M. A., Graham, J., Petropoulos, I., Tavakoli, M. & Malik, R. A. Dual-model automatic detection of nerve-fibres in corneal confocal microscopy images. Med. Image Comput. Comput. Assist Int. 13, 300–307 (2010).
Dabbah, M. A., Graham, J., Petropoulos, I. N., Tavakoli, M. & Malik, R. A. Automatic analysis of diabetic peripheral neuropathy using multi-scale quantitative morphology of nerve fibres in corneal confocal microscopy imaging. Med. Image Anal. 15, 738–747 (2011).
Chen, X. et al. An automatic tool for quantification of nerve fibers in corneal confocal microscopy images. IEEE Trans. Biomed. Eng. 64, 786–794 (2017).
Kim, J. & Markoulli, M. Automatic analysis of corneal nerves imaged using in vivo confocal microscopy. Clin. Exp. Optom. 101, 147–161 (2018).
Colonna, A., Scarpa, F. & Ruggeri, A. in Computational Pathology and Ophthalmic Medical Image Analysis. (eds D. Stoyanov et al.) 185–192 (Springer International Publishing).
Preston, F. G. et al. Artificial intelligence utilising corneal confocal microscopy for the diagnosis of peripheral neuropathy in diabetes mellitus and prediabetes. Diabetologia 65, 457–466 (2022).
Setu, M. A. K., Schmidt, S., Musial, G., Stern, M. E. & Steven, P. Segmentation and evaluation of corneal nerves and dendritic cells from in vivo confocal microscopy images using deep learning. Transl. Vis. Sci. Technol. 11, 24 (2022).
Tyler, E. F. et al. Corneal nerve changes observed by in vivo confocal microscopy in patients receiving oxaliplatin for colorectal cancer: The COCO study. J. Clin. Med. 11, 4770 (2022).
Oakley, J. D. et al. Deep learning-based analysis of macaque corneal sub-basal nerve fibers in confocal microscopy images. Eye Vis. 7, 27 (2020).
Annunziata, R. et al. Two-dimensional plane for multi-scale quantification of corneal subbasal nerve tortuosity. Investig. Ophthalmol. Vis. Sci. 57, 1132–1139 (2016).
Mehrgardt, P. et al. U-Net Segmented Adjacent Angle Detection (USAAD) for automatic analysis of corneal nerve structures. Data 5, 37 (2020).
Patel, D. V. & McGhee, C. N. J. Mapping of the normal human corneal sub-basal nerve plexus by in vivo laser scanning confocal microscopy. Investig. Ophthalmol. Vis. Sci. 46, 4485–4488 (2005).
Puri, S., Sun, M., Mutoji, K. N., Gesteira, T. F. & Coulson-Thomas, V. J. Epithelial cell migration and proliferation patterns during initial wound closure in normal mice and an experimental model of limbal stem cell deficiency. Investig. Ophthalmol. Vis. Sci. 61, 27 (2020).
Tuck, H. et al. Neuronal-epithelial cell alignment: a determinant of health and disease status of the cornea. Ocul. Surf. 21, 257–270 (2021).
Guaiquil, V. H., Xiao, C., Lara, D., Dimailig, G. & Zhou, Q. Expression of axon guidance ligands and their receptors in the cornea and trigeminal ganglia and their recovery after corneal epithelium injury. Exp. Eye Res. 219, 109054 (2022).
Zhang, Y. et al. Corneal sub-basal whorl-like nerve plexus: a landmark for early and follow-up evaluation in transthyretin familial amyloid polyneuropathy. Eur. J. Neurol. 28, 630–638 (2021).
Kalteniece, A. et al. Greater corneal nerve loss at the inferior whorl is related to the presence of diabetic neuropathy and painful diabetic neuropathy. Sci. Rep. 8, 3283 (2018).
Badian, R. A., Andréasson, M., Svenningsson, P., Utheim, T. P. & Lagali, N. The pattern of the inferocentral whorl region of the corneal subbasal nerve plexus is altered with age. Ocul. Surf. 22, 204–212 (2021).
Chiang, J. C. B. et al. Reproducibility and reliability of subbasal corneal nerve parameters of the inferior whorl in the neurotoxic and healthy cornea. Cornea 41, 1487–1494 (2022).
Zhang, X. Y., Wu, M., Chinnery, H. R. & Downie, L. E. Defining an optimal sample size for corneal epithelial immune cell analysis using in vivo confocal microscopy images. Front. Med. 9, 848776 (2022).
Vagenas, D. et al. Optimal image sample size for corneal nerve morphometry. Optom. Vis. Sci. 89, 812–817 (2012).
Edwards, K. et al. Development of a novel technique to measure corneal nerve migration rate. Cornea 35, 700–705 (2016).
Al Rashah, K. et al. Corneal nerve migration rate in a healthy control population. Optom. Vis. Sci. 95, 672–677 (2018).
Hamrah, P., Huq, S. O., Liu, Y., Zhang, Q. & Dana, M. R. Corneal immunity is mediated by heterogeneous population of antigen-presenting cells. J. Leukoc. Biol. 74, 172–178 (2003).
Jamali, A. et al. Characterization of resident corneal plasmacytoid dendritic cells and their pivotal role in herpes simplex keratitis. Cell Rep. 32, 108099 (2020).
Jamali, A. et al. Topical adoptive transfer of plasmacytoid dendritic cells for corneal wound healing. Methods Mol. Biol. 2193, 159–174 (2021).
Levine, H. et al. Relationships between activated dendritic cells and dry eye symptoms and signs. Ocul. Surf. 21, 186–192 (2021).
Aggarwal, S. et al. Correlation of corneal immune cell changes with clinical severity in dry eye disease: an in vivo confocal microscopy study. Ocul. Surf. 19, 183–189 (2021).
Cavalcanti, B. M. et al. In vivo confocal microscopy detects bilateral changes of corneal immune cells and nerves in unilateral herpes zoster ophthalmicus. Ocul. Surf. 16, 101–111 (2018).
Chirapapaisan, C. et al. Effect of herpes simplex keratitis scar location on bilateral corneal nerve alterations: an in vivo confocal microscopy study. Br. J. Ophthalmol. 106, 319–325 (2022).
Giannaccare, G. et al. Bilateral morphometric analysis of corneal sub-basal nerve plexus in patients undergoing unilateral cataract surgery: a preliminary in vivo confocal microscopy study. Br. J. Ophthalmol. 105, 174–179 (2020).
Luna, C. et al. Unilateral corneal insult also alters sensory nerve activity in the contralateral eye. Front. Med. 8, 767967 (2021).
Lee, H. K. et al. Bilateral effect of the unilateral corneal nerve cut on both ocular surface and lacrimal gland. Investig. Ophthalmol. Vis. Sci. 60, 430–441 (2019).
Guzman, M. et al. The mucosal surfaces of both eyes are immunologically linked by a neurogenic inflammatory reflex involving TRPV1 and substance P. Mucosal Immunol. 11, 1441–1453 (2018).
Ferrari, G. et al. Ocular surface injury induces inflammation in the brain: In vivo and ex vivo evidence of a corneal-trigeminal axis. Investig. Ophthalmol. Vis. Sci. 55, 6289–6300 (2014).
Aggarwal, S. et al. Autologous serum tears for treatment of photoallodynia in patients with corneal neuropathy: efficacy and evaluation with in vivo confocal microscopy. Ocul. Surf. 13, 250–262 (2015).
Giannaccare, G. et al. In vivo and ex vivo comprehensive evaluation of corneal reinnervation in eyes neurotized with contralateral supratrochlear and supraorbital nerves. Cornea 39, 210–214 (2020).
Moein, H. R. et al. Visualization of micro-neuromas by using in vivo confocal microscopy: an objective biomarker for the diagnosis of neuropathic corneal pain? Ocul. Surf. 18, 651–656 (2020).
Ross, A. R. et al. Clinical and in vivo confocal microscopic features of neuropathic corneal pain. Br. J. Ophthalmol. 104, 768–775 (2020).
Belmonte, C., Acosta, M. C. & Gallar, J. Neural basis of sensation in intact and injured corneas. Exp. Eye Res. 78, 513–525 (2004).
Fried, K., Govrin-Lippmann, R., Rosenthal, F., Ellisman, M. H. & Devor, M. Ultrastructure of afferent axon endings in a neuroma. J. Neurocytol. 20, 682–701 (1991).
Stepp, M. A. et al. Corneal epithelial “neuromas”: a case of mistaken identity? Cornea 39, 930–934 (2020).
Machet, J. et al. Type 2 diabetes influences intraepithelial corneal nerve parameters and corneal stromal-epithelial nerve penetration sites. J. Diabetes Investig. https://doi.org/10.1111/jdi.13974 (2023).
Hao, R. et al. Analysis of globular cells in corneal nerve vortex. Front. Med. 9, 806689 (2022).
Colorado, L. H., Dando, S. J., Harkin, D. G. & Edwards, K. Label-free imaging of the kinetics of round-shaped immune cells in the human cornea using in vivo confocal microscopy. Clin. Exp. Ophthalmol. 49, 628–630 (2021).
Gao, N., Lee, P. & Yu, F. S. Intraepithelial dendritic cells and sensory nerves are structurally associated and functional interdependent in the cornea. Sci. Rep. 6, 36414 (2016).
Loi, J. K. et al. Corneal tissue-resident memory T cells form a unique immune compartment at the ocular surface. Cell Rep. 39, https://doi.org/10.1016/j.celrep.2022.110852 (2022).
Chiang, J. C. B. et al. Corneal dendritic cells and the subbasal nerve plexus following neurotoxic treatment with oxaliplatin or paclitaxel. Sci. Rep. 11, 22884 (2021).
Khan, A. et al. Corneal immune cells are increased in patients with multiple sclerosis. Transl. Vis. Sci. Technol. 10, 19 (2021).
Hoffman, J. J. et al. Diagnosis of fungal keratitis in low-income countries: evaluation of smear microscopy, culture, and In vivo confocal microscopy in Nepal. J. Fungi 8, 955 (2022).
Alantary, N., Heaselgrave, W. & Hau, S. Correlation of ex vivo and in vivo confocal microscopy imaging of Acanthamoeba. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2022-321402 (2022).
Wang, Y. E. et al. Role of in vivo confocal microscopy in the diagnosis of infectious keratitis. Int. Ophthalmol. https://doi.org/10.1007/s10792-019-01134-4 (2019).
Chidambaram, J. D. et al. Cellular morphological changes detected by laser scanning in vivo confocal microscopy associated with clinical outcome in fungal keratitis. Sci. Rep. 9, 8334 (2019).
Britten-Jones, A. C., Craig, J. P., Anderson, A. J. & Downie, L. E. Association between systemic omega-3 polyunsaturated fatty acid levels, and corneal nerve structure and function. Eye https://doi.org/10.1038/s41433-022-02259-0 (2022).
Marquez, A. et al. Tau associated peripheral and central neurodegeneration: identification of an early imaging marker for tauopathy. Neurobiol. Dis. 151, 105273 (2021).
Feldman, E. L. et al. Diabetic neuropathy. Nat. Rev. Dis. Prim. 5, 41 (2019).
Perkins, B. A. et al. Corneal confocal microscopy predicts the development of diabetic neuropathy: a longitudinal diagnostic multinational consortium study. Diabetes Care 44, 2107–2114 (2021).
Perkins, B. A. et al. Corneal confocal microscopy for identification of diabetic sensorimotor polyneuropathy: a pooled multinational consortium study. Diabetologia 61, 1856–1861 (2018).
Tummanapalli, S. S. et al. Tear film substance P: a potential biomarker for diabetic peripheral neuropathy. Ocul. Surf. 17, 690–698 (2019).
Lagali, N. S. et al. Dendritic cell maturation in the corneal epithelium with onset of type 2 diabetes is associated with tumor necrosis factor receptor superfamily member 9. Sci. Rep. 8, 14248 (2018).
Ponirakis, G. et al. Progressive loss of corneal nerve fibers is associated with physical inactivity and glucose lowering medication associated with weight gain in type 2 diabetes. J. Diabetes Investig. 13, 1703–1710 (2022).
Xu, J. et al. In vivo confocal microscopic evaluation of corneal dendritic cell density and subbasal nerve parameters in dry eye patients: a systematic review and meta-analysis. Front. Med. 8, 578233 (2021).
Bron, A. J. et al. TFOS DEWS II pathophysiology report. Ocul. Surf. 15, 438–510 (2017).
Bohn, S. et al. In vivo monitoring of corneal dendritic cells in the subbasal nerve plexus during trastuzumab and paclitaxel breast cancer therapy—a one-year follow-up. Diagnostics 12, 1180 (2022).
Allgeier, S. et al. Real-time large-area imaging of the corneal subbasal nerve plexus. Sci. Rep. 12, 2481 (2022).
Allgeier, S. et al. A novel approach to analyze the progression of measured corneal sub-basal nerve fiber length in continuously expanding mosaic images. Curr. Eye Res. 42, 549–556 (2017).
Matuszewska-Iwanicka, A. et al. Mosaic vs. single image analysis with confocal microscopy of the corneal nerve plexus for diagnosis of early diabetic peripheral neuropathy. Ophthalmol. Ther. https://doi.org/10.1007/s40123-022-00574-z (2022).
Schenk, M. S. et al. Advances in imaging of subbasal corneal nerves with micro-optical coherence tomography. Transl. Vis. Sci. Technol. 10, 22 (2021).
Mazlin, V. et al. Real-time non-contact cellular imaging and angiography of human cornea and limbus with common-path full-field/SD OCT. Nat. Commun. 11, 1868 (2020).
Han, L. et al. Line-scanning SD-OCT for in-vivo, non-contact, volumetric, cellular resolution imaging of the human cornea and limbus. Biomed. Opt. Express 13, 4007–4020 (2022).
Jain, A., Hakim, S. & Woolf, C. J. Unraveling the plastic peripheral neuroimmune interactome. J. Immunol. 204, 257–263 (2020).
Mazlin, V. et al. Non-contact cell-detail real-time full-field OCT: capabilities and potential clinical applications of the novel anterior eye imaging tool. Investig. Ophthalmol. Vis. Sci. 60, 8 (2019).
Yang, C. et al. Multi-discriminator adversarial convolutional network for nerve fiber segmentation in confocal corneal microscopy images. IEEE J Biomed. Health Inform. https://doi.org/10.1109/jbhi.2021.3094520 (2021).
Yildiz, E. et al. Generative adversarial network based automatic segmentation of corneal subbasal nerves on in vivo confocal microscopy images. Transl. Vis. Sci. Technol. 10, 33 (2021).
Mou, L. et al. DeepGrading: deep learning grading of corneal nerve tortuosity. IEEE Trans. Med. Imaging 41, 2079–2091 (2022).
Xu, F. et al. A deep transfer learning framework for the automated assessment of corneal inflammation on in vivo confocal microscopy images. PLoS One 16, e0252653 (2021).
Lee, H. J. et al. Utility of in vivo confocal microscopy in diagnosis of acanthamoeba keratitis: a comparison of patient outcomes. Cornea 42, 135–140 (2023).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editors: Chao Zhou and Manuel Breuer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chiang, J.C.B., Roy, M., Kim, J. et al. In-vivo corneal confocal microscopy: Imaging analysis, biological insights and future directions. Commun Biol 6, 652 (2023). https://doi.org/10.1038/s42003-023-05005-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-023-05005-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.