Abstract
Stroke survivors frequently report increased perceived challenge of walking (PCW) in complex environments, restricting their daily ambulation. PCW is conventionally measured through subjective questionnaires or, more recently, through objective quantification of sympathetic nervous system activity during walking tasks. However, how these measurements of PCW reflect daily walking activity post-stroke is unknown. We aimed to compare the subjective and objective assessments of PCW in predicting home and community ambulation. In 29 participants post-stroke, we measured PCW subjectively with the Activities-specific Balance Confidence (ABC) Scale and objectively through electrodermal activity, quantified by change in skin conductance levels (SCL) and skin conductance responses (SCR) between outdoor-complex and indoor-steady-state walking. High-PCW participants were categorized into high-change SCL (ΔSCL ≥ 1.7 μs), high-change SCR (ΔSCR ≥ 0.2 μs) and low ABC (ABC < 72%) groups, while low-PCW participants were categorized into low-change SCL (ΔSCL < 1.7 μs), low-change SCR (ΔSCR < 0.2 μs) and high-ABC (ABC ≥ 72%) groups. Number and location of daily steps were quantified with accelerometry and Global Positioning System devices. Compared to low-change SCL group, the high-change SCL group took fewer steps in home and community (p = 0.04). Neither ABC nor SCR groups differed in home or community steps/day. Objective measurement of PCW via electrodermal sensing more accurately represents home and community ambulation compared to the subjective questionnaire.
Similar content being viewed by others
Introduction
Stroke is a major leading cause of disability world-wide, afflicting more than 795,000 people in the United States of America every year1. The southeastern region of USA, including north Florida2, is often referred to as ‘the stroke belt’ due its 20–32% higher prevalence of stroke than the national average3. Most individuals regain the ability to walk in safe and predictable environments, such as their home, within 6 months post-stroke4, however, as many as 74% report dissatisfaction with their level of community ambulation outside of their home environment5. Stroke survivors frequently perceive community ambulation as challenging6,7,8 and report reduced balance confidence in accomplishing common, yet complex tasks such as negotiating uneven terrains and walking in unpredictable, crowded environments5,8. Perceived challenge of walking is a broad term that encompasses fear of falling, balance confidence, and anxiety specifically pertaining to walking-related activities6,9. The prevalence of increased perceived challenge of walking varies between 32 and 83% between the first six months to over four years post-stroke10,11. In fact, increased perceived challenge of walking triggers a fear-avoidance cycle12,13, leading to diminished self-reported community ambulation14, total daily walking activity8,15,16,17 and community participation13,18,19, limitations beyond those simply secondary to post-stroke physical impairments20. Thus, addressing perceived challenge of walking is vital for improving community ambulation, an essential yet unmet goal for more than 90% stroke survivors21,22.
Conventionally, the construct of perceived challenge of walking has been measured through self-report questionnaires that assess one’s confidence to perform daily activities without falling. For example, the modified Falls-Efficacy questionnaire23 and the Activities-Specific Balance Confidence (ABC) Scale24 evaluate balance confidence during standing- and walking-related activities in and around one’s home/yard and community environment. While these standardized questionnaires are validated, easy to administer, inexpensive and time efficient, subjective measurement of perceived challenge comes with biases such as over-reporting positive traits, under-reporting negative traits or choosing extreme scores25,26. Moreover, since self-reported balance confidence is solely based on one’s own interpretation of their abilities to perform complex tasks, it does not always align with the physiological stresses of walking in challenging situations6. Since perceived challenge has a strong impact on community ambulation5,13,16, its assessment needs to be coupled with objective measures based on physiologic responses that may or may not be consciously perceived by an individual, such as quantification of sympathetic nervous system (SNS) activity9,27,28,29.
SNS is activated during physically or cognitively challenging and stressful situations, eliciting a ‘fight or flight’ response, causing an increase in eccrine sweat gland activity, elevated cardiopulmonary responses as well as a drop in skin temperature27,30,31,32. These increased physiological stress responses may be objectively quantified through continuous monitoring of pulse wave, skin temperature and skin conductance31,32. Arterial pulse wave monitoring quantifies an individual’s heart rate variability (HRV), which is known to decrease under stressful situations such as when walking in complex urban streets versus calming forest trails31,32,33,34. Skin temperature is also known to drop when viewing fearful graphics in young healthy adults35. However, both HRV measurement and skin temperature analysis have not yet been validated to measure autonomic stress responses during walking in individuals with stroke. Moreover, HRV and skin temperature are influenced by both sympathetic and parasympathetic nervous system whereas eccrine sweat gland activity in the palms and soles is primarily controlled by the SNS through sudomotor nerves and is less impacted by thermoregulatory changes9,36. In stressful situations, increased eccrine sweat gland activity leads to reduced resistance and increased electrical conductance of the skin, which can be easily measured with a small, imperceptible direct current via skin conductance27,30. Additionally, through a series of investigations Clark et al., and Chatterjee et al., have demonstrated the feasibility, utility, and validity of skin conductance measurement in quantifying SNS activity during challenging walking tasks in varied indoor and outdoor environments for both older adults9,28 and people post-stroke6,37.
Compared to indoor walking, stroke survivors demonstrated increased SNS responses during challenging outdoor tasks like walking up and down a ramp, negotiating a curb, and walking on grassy terrain6,9,37. Higher SNS activity during complex walking tasks is also associated with worse task performance, as quantified by slower walking speeds6. Thus, SNS activity reflects both the ‘conscious’ and ‘unconscious’ aspects of perceived challenge, fear of falling, as well as anticipation of possible negative consequences (e.g., falls), present when performing challenging tasks9,28,29. Moreover, SNS activity depends on several factors such as the demands of and an individual’s physical skill for completing the task, their past experience with and their perceived confidence in accomplishing the task successfully as well as the environment in which the task is performed6. These factors form important components of successful community ambulation, and may influence one’s decision to engage in community ambulation, outside the familiarity of their home38. Thus, unlike self-reported balance confidence27, assessing SNS responses via skin conductance allows for valid, objective, non-invasive, nonverbal, and involuntary assessment of physiological stress responses during community ambulation27. Yet, it is unknown if community ambulation can be more accurately predicted with objective, sensor-based measure of perceived challenge or through subjective balance confidence questionnaires. To successfully enhance community ambulation, it is essential to accurately identify individuals who perceive a high challenge of walking and assess how their perceived challenge may impact their daily walking activity in home and community environments.
Moreover, over the past two decades, the measurement of community ambulation has advanced from self-reported questionnaires to utilizing wearable sensors to measure daily steps21,39,40. However, as community ambulation is most widely defined as “independent mobility outside the home, which includes the ability to confidently negotiate uneven terrain, private venues, shopping centers and other public spaces”21, simply quantifying total daily steps does not accurately reflect this definition. To fully understand and correctly report post-stroke walking ability, it is vital to specifically quantify true community ambulation as only that which occurs outside the home. With improvement in Global Positioning System (GPS) technology, daily stepping activity can now be accurately parsed into home and community steps post-stroke41,42,43. Yet, it is unknown if perceived challenge of walking impacts community ambulation that specifically occurs outside-of-home. Analyzing the utility of wearable technology like accelerometers, GPS devices and skin conductance sensors may encourage the clinical use of consumer-friendly technological resources to quantify both perceived challenge of walking as well as home and community ambulation post-stroke.
Thus, the primary purpose of this study was to test differences in home and community ambulation between stroke survivors with lower and higher perceived challenge of walking. We hypothesized that compared to individuals with low perceived challenge of walking, those with high perceived challenge of walking would take fewer home and community steps, when perceived challenge of walking was measured objectively with SNS activation, but not when measured subjectively with the ABC scale.
Methods
This cross-sectional study was conducted at the Malcolm Randall VA Medical Center, Gainesville, and Brooks Rehabilitation Clinical Research Center, Jacksonville, Florida between October 2019 and May 2021. Participants were: (1) at least six months post-stroke, (2) > 18 years of age, (3) community-dwelling, (4) able to follow 3-step command, (5) able to ambulate independently without physical assistance from another person, with or without an assistive or orthotic device, and (6) community ambulators. Participants were excluded for (1) a neurological diagnosis other than stroke, (2) history of intermittent claudication, (3) angina at rest or with minimal exertion, (4) history of COPD, (5) orthopedic conditions that limit mobility, and (6) ongoing physical rehabilitation services. Eligible participants signed a written informed consent form approved by the University of Florida Institutional Review Board. The procedures used in this study were approved by the University of Florida’s Institutional Review Board (IRB#201901748 and IRB#201900944) and adhere to the tenets of the Declaration of Helsinki. This study’s protocol is based on our previously published work6,9,28,37.
To characterize our participants clinical walking capacity, we assessed their gait speed and gait-related endurance. To obtain gait speed, participants walked on a GAITRite mat, an instrumented, computerized 4.98-m walkway, and completed two trials at their self-selected speed. Gait speed was calculated as the average of the two trials. The GAITRite has shown high concurrent validity in measuring hemiparetic gait speed when compared with 3-Dimentional motion capture system44. The Six-Minute Walk Test (6MWT) assessed participants’ gait endurance45,46,47, as they walked for six minutes around a 16-m walkway. The 6MWT has demonstrated excellent test–retest reliability (ICC: 0.95)48. Customary assistive and orthotic devices were permitted for assessments.
Perceived challenge of walking during daily home and community ambulation was assessed subjectively with the ABC Scale24. This 16-item self-report questionnaire assesses the stem question “How confident are you that you will not lose your balance or become unsteady when you…” on a scale of 0% (not confident at all) to 100% (completely confident). The ABC scale has high internal consistency (Cronbach’s α = 0.94), excellent test–retest reliability (ICC = 0.85) and has a moderately positive association with functional balance ability measured by the Berg Balance Scale (ρ = 0.36) as well as gait speed (ρ = 0.48) in individuals post-stroke24. The final score was calculated as a 16-item average, in which higher percentage values depicted higher balance confidence (lower perceived challenge).
SNS activity was measured from palmar sweat responses as participants walked a prescribed, laboratory-based indoor (lower challenge) and outdoor (higher challenge) course. All participants completed one trial of each task in the order outlined in Table 1. We chose not to randomize the order of the tasks as SNS responses may increase rapidly when performing a higher challenge task but may display a slower recovery to baseline if participants performed the higher challenge task first followed by the lower challenge task49. A waist belt-worn data acquisition unit (Flexcomp Infiniti, Thought Technology, Montreal, QC, Canada) recorded participants’ palmar sweat responses. Adhesive and disposable electrodes, with a conductive paste (0.5% saline in a neutral base) applied to the 10 mm Ag/AgCl recording surface, were securely placed on the proximal phalanges of both hands’ index and ring fingers50. An event-marking device connected to the data acquisition unit was manually activated by study personnel to insert markings in the data pertaining to key events of baseline resting, indoor, and outdoor walking tasks. Verbalization was limited to the provision of directions of the prescribed path, to reduce extraneous influence on SNS responses.
To accurately quantify true community ambulation as only that which occurs outside the home, participants wore an accelerometer (StepWatch Activity Monitor-4 (SAM)) along with a GPS device (GlobalSat DG-500) for seven days. The SAM demonstrates high test–retest reliability (ICC > 0.96)51 and high criterion validity (Pearson’s r = 0.96) for post-stroke step counts in both indoor and outdoor environments52. The GlobalSat, a pager-sized GPS device53,54,55, recorded participants’ location at 5-s intervals on a micro SD card, viewed post-data collection with device-specific software54. GlobalSat GPS devices have been validated to study outdoor walking53 and have been previously used to quantify outdoor ambulation in people with stroke41. Participants wore the GPS device on a waist belt and the SAM on their non-paretic ankle during all waking hours except while bathing. Participants charged the GPS device nightly. To complement the GPS data during data cleaning, and analysis, participants completed a Trip Activity Log (TAL) (Supplemental Material#1, Fig. S1.1). One complete trip was operationally defined as leaving one’s home/yard space to go out in the community and returning home5. A trip may include visiting multiple types of locations such as going to a coffee shop, followed by grocery store and then a medical appointment before returning home. Participants were instructed to fill out the time they departed from home and arrived back home for each trip per day.
Data analysis
Skin conductance signals were sampled at 32 Hz, and downloaded through Biograph Infiniti software (Thought Technology, Montreal, QC, Canada). Skin conductance was analyzed using MATLAB (v. R2019a; The Mathworks, Natick MA) with Ledalab v3.4.9. Raw data were down-sampled to 8 Hz followed by visual inspection for major signal artifacts that may be attributable to abrupt finger movements (e.g., forming a fist), tugging of wires or other unknown sources. Such major artifacts were indicated by rapid, high frequency fluctuations in their signal amplitude, inconsistent with the rate of amplitude change typically observed in electrodermal responses6,9,28,37. Relatively few outlying artifacts were identified and these were removed and replaced with linear interpolation (see example raw data plot in Supplementary Material#2, Fig. S2). Analyzed skin conductance signals were separated into skin conductance level (SCL) and skin conductance response (SCR) components using continuous decomposition analysis28,50. SCL indicates overall, slow-tonic responses to the challenges of walking whereas moments of acute unsteadiness and fear during walking are represented through the fast-phasic and high frequency changes in SCR6,27. An amplitude criterion of 0.05 microsiemens (μS) defined SCRs and minimized any movement artifacts6.
We determined change in SCL from simple indoor tasks to complex outdoor walking tasks as:
Similarly, change in the rate of SCR from indoor to outdoor walking tasks was calculated as:
The rate of SCRs was defined as the number of SCRs detected during a recording period, divided by the duration of the recording period6. We used the mean of each of the three perceived challenge of walking variables (∆SCL, ∆SCR and ABC) to categorize participants into higher and lower perceived challenge groups as accurate cut-offs for these variables have not been established in the literature. By evaluating the accuracy of each of the three variables, the results of this categorization would help clinicians and rehabilitation scientists choose the most accurate variable when predicting community ambulation post-stroke.
For quantification of community ambulation, the SAM provided total strides/day over 10-s intervals in a Microsoft Excel format56. To obtain total steps/day, the number of strides were doubled, and then summed. To ensure compliance, step data was plotted and visually inspected for at least 8 h of wear time per day (see example plots in Supplemental Material#1, Fig. S1.2)57. Any day that did not meet this criterion was excluded from the analysis. Location data (latitude, longitude, timestamp) from the GPS device was downloaded via GlobalSat software in a Microsoft Excel format. Using time stamp synchronization in MATLAB through a custom code, we mapped the SAM-derived stepping activity onto the location data from the GPS device. The latitude and longitude for the patient’s residential address was derived from Google Maps. Home was operationally defined as an individual’s geographical residential address with an 85-m surrounding perimeter. The 85-m radius accounted for average yard space58 and any erroneous spikes (i.e., noise) in the GPS signals when indoors. Each participant’s walking location was categorized as home or community (location away from home). The GPS file was visually inspected for any missing data that exceeded 30 min. Any missing GPS data was compared with the participant’s TAL and characterized as ‘missing at home’, ‘missing in community’, or ‘missing while in transition between home and community’. For missing GPS data while the participant was at home, MATLAB automatically characterized steps during this period as ‘home steps’. If the missing GPS data coincided completely with the participant’s time outside of home, MATLAB interpolated the data between the previous and next locations in the community, classifying all steps taken during this missing period as ‘community steps’. If GPS data was missing while the participant was in transition between home and community, and if steps taken during this period were less than 10% of total steps for the day, MATLAB interpolated the step data between the previous and next GPS location. However, if steps taken during the ‘missing while in transition’ period exceeded 10% of the total steps for that day, the entire day was excluded from the analysis to ensure more than 90% accuracy in classifying steps as home and community (see SAM-GPS data analysis algorithm in Supplemental Material#1, Fig. S1.3). Data included in the analysis were obtained from devices worn for at least four days and eight hours per day. Home and community steps/day were extracted and averaged for the recording period. All authors have full access to study data and take responsibility for its integrity.
Statistical analysis
We used the Kolmogorov–Smirnov and Shapiro–Wilk tests59 to determine the normality of all variables. To examine any differences in clinical or demographic characteristics with the ΔSCL, ΔSCR and ABC groups, we conducted independent t-tests. To assess the relationship between ΔSCL, ΔSCR, ambient temperature and relevant demographic characteristics, we conducted Pearson product-moment correlation and Spearman’s Rho correlation tests for the continuous and categorical variables, respectively. To examine differences between indoor and outdoor walking in SCR and SCL within each participant, we conducted repeated measures ANOVA tests with ambient temperature as a covariate. To assess for differences in home and community ambulation between the groups of higher and lower perceived challenge, we conducted three separate MANOVA models (one model for each classification variable: ∆SCL, ∆SCR and ABC). Any significant main effects were interpreted with follow-up univariate analyses with Bonferroni corrections. We used the Box’s M test (Box’s Test for Equivalence of Covariance Matrices) to test if the covariation between dependent variables was equal across groups. After confirming multivariate normality assumptions (a non-significant Box’s M) and non-redundancy of independent variables, we proceeded with statistical analysis, using the Statistical Package for the Social Sciences (SPSS, Version 24) with the significance level set at alpha equal to 0.05. Power analysis suggested a total of 29 subjects to achieve 80% power (Details in Supplementary Material#3). To account for non-compliance and technical issues, we enrolled a total of 40 individuals in this study. Any differences in demographic and clinical characteristics between the included and excluded participants were tested through independent t-tests (continous variables) and Chi-square tests (categorical variables).
Results
Of the forty individuals enrolled, eleven were excluded from the final analysis due to: non-compliance with wearing the SAM/GPS devices (n = 2), insufficient GPS data (n = 2), technical difficulties with recording skin conductance (n = 2) and poor-quality of processed SNS signals with extremely low amplitude (n = 5). Thus, the final analysis included 29 participants. Demographic and clinical characteristics did not differ between the included and excluded participants (Table 2).
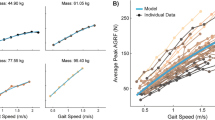
Most participants (69.4%) used an assistive device in their non-paretic hand for balance support during walking trials (Table 2). Since pressure and contact with the assistive device can significantly alter skin conductance50, we analyzed SNS signals from the paretic hand only. The ambient outdoor temperature for all participants ranged between – 2 °C to 34 °C (average 21° ± 8 °C) and had a moderately positive association with ΔSCL (r = 0.48, p = 0.008), but not with ΔSCR (see Supplemental Material#3, Table S3). The interaction between ambient outdoor temperature (covariate) and indoor and outdoor SCL values within each participant was significant (Wilks’ Λ = 0.77; F (27, 1) = 8.21; p = 0.008, Effect size ŋ2 = 0.233). Even after accounting for ambient temperature, outdoor SCL (3.47 ± 3.25 µs) was significantly higher than indoor SCL (1.75 ± 1.77 µs) (p < 0.001), suggesting a higher perceived challenge in the outdoor walking environment, as compared to indoor (Fig. 1A). In contrast, outdoor SCR (0.25 ± 0.25) did not differ from indoor SCR (0.26 ± 0.23) (p = 0.83) in our cohort (Fig. 1B).
Difference between indoor and outdoor sympathetic nervous system activity measurements using repeated measures ANOVA tests with ambient temperature as a covariate. (A) Outdoor SCL (green) is significantly higher than indoor SCL (red), after accounting for ambient temperature (**p < 0.001) [SCL(indoor or outdoor) = Walking maximum − Resting minimum]. (B) Outdoor SCR (green) is not significantly different from indoor SCR (red) [SCR(indoor or outdoor) = Rate of SCR during walking − Rate of SCR during rest].
The categorization of higher and lower perceived challenge groups based on mean ∆SCL, ∆SCR and ABC values is depicted in Table 3. Albeit non-significant, all lower perceived challenge groups (lower ΔSCL, lower ΔSCR, higher ABC) showed trends of faster gait speed and greater distance covered in the 6MWT, as compared to all higher perceived challenge groups (higher ΔSCL, higher ΔSCR, lower ABC groups) with small to medium effect sizes as depicted by Hedges’ g in Table 4.
Home and community steps/day differed significantly between the higher and lower ΔSCL groups (Main effect: Wilks’ Λ = 0.752; F(26, 2) = 4.29; p = 0.024, Effect size ŋ2 = 0.248). Follow-up univariate analysis showed that higher ΔSCL group took significantly fewer daily steps at home and in the community than the lower ΔSCL group, (Table 5, Fig. 2A). In contrast to ΔSCL groups, home and community steps/day did not differ significantly between the higher and lower ΔSCR groups (Main effect: Wilks’ Λ = 0.852; F(26, 2) = 2.25; p = 0.12, Effect size ŋ2 = 0.148). Although non-significant, as compared to lower ΔSCR group, the higher ΔSCR group showed trends towards reduced home and community steps/day with medium effect sizes (Table 5, Fig. 2B). Home and community steps/day did not differ significantly between the higher and lower ABC groups (Main effect: Wilks’ Λ = 0.99; F(26, 2) = 0.07; p = 0.93, Effect size ŋ2 = 0.005) (Table 5, Fig. 2C).
Difference in home steps and community steps/day between higher and lower perceived challenge of walking groups. (A) Higher ΔSCL group (blue) took significantly fewer home steps/day (Hedges’ g = 0.80) and community steps/day (Hedges’ g = 0.80) than the lower ΔSCL group (orange) (*p < 0.05). (B) The higher ΔSCR group (blue) showed trends towards reduced home steps/day (Hedges’ g = 0.55) and community steps/day (Hedges’ g = 0.63) than the lower ΔSCR group (orange). (C) Higher ABC group (orange) did not differ in home steps/day (Hedges’ g = 0.07) and community steps/day (Hedges’ g = 0.13) from the lower ABC group (blue). ABC-Activities-specific Balance Confidence Scale.
Discussion
This study aimed to test the hypothesis that individuals with high perceived challenge of walking would take fewer home and community steps than those with high perceived challenge of walking, when perceived challenge of walking was measured objectively with SNS activation, but not when measured subjectively with the ABC scale. Consistent with the hypothesis, individuals post-stroke who demonstrated higher perceived challenge of walking took fewer daily home and community steps than those with lower perceived challenge of walking, when perceived challenge of walking was quantified objectively, but not subjectively.
Our study provides unique evidence regarding the utility of assessing SNS responses during challenging walking tasks in differentiating between GPS-based daily home and community ambulation levels post-stroke. Measuring SNS responses to challenging walking tasks through wearable sensors provided an objective and unbiased assessment of how stroke survivors in our cohort perceived complex walking tasks as well as how this perception impacted their daily home and community steps. In the present study, individuals with above average increase in SCL between indoor and outdoor environments took significantly fewer home and community steps per day than individuals with below average increase in SCL. A similar trend of reduced home and community ambulation was also observed in the higher ΔSCR group, as compared to the lower ΔSCR group, with medium effect sizes (Table 5, Fig. 2A,B).
Previous reports have concluded that elevated autonomic stress responses are associated with decreased physical activity and increased sedentary time in healthy men and women60,61,62. This is the first study to suggest that SNS responses impact walking activity at home for individuals post-stroke. Experiencing a higher perceived challenge of walking may have negatively impacted our participants’ ability, intention and confidence to walk around at home38. On the other hand, in the presence of lower perceived challenge of walking one may be more apt to walk in the home to do daily chores, as well as complete tasks in one’s yard, such as going to the mailbox, or taking out trash, thus contributing to increased daily home steps per day63.
Similar to home ambulation, higher perceived challenge of walking, as evaluated by physiological measures, also hindered community ambulation in our participants. Previous research has reported increased SNS responses in older adults and in individuals post-stroke as they walked in complex environments6,9,37. Additionally, stroke survivors who demonstrated increased SNS responses during challenging walking tasks also exhibited cautious and slow gait patterns along with poorer task performance in previous reports6,9,37. Indeed, in our study, individuals with higher perceived challenge of walking demonstrated trends of slower gait speeds and reduced 6MWT distances as compared to those in the lower perceived challenge of walking. Since community ambulation requires one to walk for longer distances64 with confidence and adaptability to negotiate varied environments such as sidewalks with unanticipated crowds and uneven terrains like grass, and ramps5,21,65, participants within the high ΔSCL group may have found it difficult to walk in these complex scenarios, leading to disengagement or avoidance of community ambulation8. Furthermore, in a recent study, stroke survivors reported increased perceived level of walking difficulty during challenging walking tasks, similar to those conducted in the present study, like walking on grass and ramps, as compared to walking on a level surface7. Our findings support previous qualitative studies in which stroke survivors voiced their anxiety, insecurity and fear of falling as barriers to walking outdoors and gait-related participation38,66. With the advantage of wearable sensors, our results suggest that such heightened emotional and physiological stresses of challenging walking tasks may be more accurately measured through skin conductance than self-reported balance confidence and could differentiate between daily community ambulation levels in individuals with stroke.
In contrast, participants with higher and lower ABC scores (lower and higher perceived challenge of walking, respectively) did not differ in their daily home and community steps. It is plausible that our participants’ self-reported ABC scores may not have aligned with their actual confidence and ability to ambulate in their home and community environments, and may have been impacted by individual personality traits, culture, introspective abilities and literacy levels26. Individuals in the higher and lower ΔSCL and ΔSCR groups reported strikingly similar average ABC scores, despite demonstrating markedly different SNS responses while performing some of the ABC scale items such walking up and a down a ramp, uneven terrain, and outdoor sidewalks (Table 4). Like the ΔSCL and ΔSCR groups, the low ABC group demonstrated trends of slower gait speeds and reduced 6MWT distances than the high ABC group. However, unlike the SNS groups, these differences in clinical walking capacity did not translate to home and community environments for the subjective ABC groups, further highlighting the unique impact of SNS responses on community ambulation in our cohort. Moreover, only half of the items on the ABC scale are specifically related to walking outside one’s home in the community and some of these were not applicable to our cohort living in Florida, such as walking on icy sidewalks24. These characteristics of the ABC scale may have led to discrepancies between the subjective and objective measurement of perceived challenge of walking and impacted the ABC scale’s utility to distinguish between true community ambulation levels post-stroke. Similar discrepancies between self-reported ABC scores and SNS responses to challenging walking tasks have been stated previously in individuals with stroke6 and lower limb amputation67. Our findings are in conflict with previous reports that suggested a positive association between self-reported balance confidence and community ambulation14, community reintegration18,19,68 and daily walking activity post-stroke15,17,69,16. However, these previous studies examined community ambulation either only through self-report questionnaires14,18,19,68 or through total daily steps, not parsed into location of walking activity13,15,17. Like self-reported balance confidence, self-reported community ambulation may be prone to subjective biases and recall errors. Moreover, as community ambulation is defined as “independent mobility outside the home”21, simply quantifying total daily steps does not accurately reflect this definition. Thus, the inclusion of accelerometer and GPS technology strengthened the present study, compared to previous studies, to accurately examine community ambulation levels without subjective biases and uniquely parsed total daily steps specifically into home and community steps/day. Our results suggest that rehabilitation professionals should exercise caution when predicting community ambulation status merely based on self-reported balance confidence in patients post-stroke. This study provides vital insights to clinicians and rehabilitation professionals on the importance of assessing both community ambulation and perceived challenge of walking using objective, real-time measures.
Limitations
We studied participants’ SNS activation as they traversed an outdoor walking path designed to mimic a typical community environment, yet provided close supervision to assure participants’ safety. However, stress responses may differ in a true real-world, community-based environment such as a mall or park where stroke survivors may walk independently, without supervision. Due to limited sensitivity of skin conductance measurement in accurately distinguishing various walking subtasks such as walking on grass or ramp9,37, we analyzed our outdoor walking task as one entity. It is possible that some subtasks may have had a larger contribution to outdoor SCL and SCR than others. Additionally, our findings may have been influenced by factors other than complexity of walking tasks as we did not randomize our task order. However, as described before, performing lower challenge tasks before higher challenge tasks was necessary to accurately detect any increase in SNS responses49. Moreover, as true cut-offs for categorizing individuals into higher and lower perceived challenge groups have not been established in the literature, we used the mean of each of the three variables to compare subgroups. Further research is warranted to establish accurate cut-off scores to classify individuals with stroke into higher or lower perceived challenge groups. Furthermore, as this study was conducted in the subtropical climate of Florida, our results may not generalize to geographic areas with extremely cold climates. Lastly, at the time of this study, the ABC scale was the only validated questionnaire that assesses balance confidence during both home and community ambulation post-stroke. Further investigation of other validated questionnaires of perceived challenge of walking and their association with community ambulation is warranted.
Conclusion
In the present study, stroke survivors with higher perceived challenge of walking in complex outdoor walking activities, as objectively measured by skin conductance, took fewer daily steps in both home and community, as compared to those with lower perceived challenge of walking. The impact of perceived challenge of walking on daily home and community ambulation was more accurately evaluated through SNS responses than a self-reported questionnaire in our cohort. As stroke survivors may over- or under-estimate their balance confidence in daily life, rehabilitation specialists should be aware of the potential limitations of predicting home and community ambulation levels solely based on subjective assessments. With increased advances in consumer-friendly wearable technology70,71, researchers should consider developing and validating clinically applicable, consumer-friendly, wearable devices to examine real-time SNS responses during challenging walking tasks as well as to quantify daily home and community ambulatory activity. While our previous work demonstrated reduced SNS activity following gait rehabilitation37,72, future research may investigate the impact of diminished perceived challenge of walking on daily home and community ambulation.
Data availability
The data that support the findings of this study are available on request from the corresponding author, [KB]. The data are not publicly available due to their containing information that could compromise the privacy of research participants (participant’s home addresses from GPS devices).
Abbreviations
- ABC:
-
Activities-specific balance confidence
- SNS:
-
Sympathetic nervous system
- SCL:
-
Skin conductance levels
- SCR:
-
Skin conductance responses
- 6MWT:
-
Six-minute walk test
- SAM:
-
Step activity monitor
- TAL:
-
Trip activity log
References
Virani, S. S. et al. Heart disease and stroke statistics—2021 update: A report from the American Heart Association. Circulation 135, e143 (2021).
Siegel, P. Z., Wolfe, L. E., Wilcox, D. & Deeb, L. C. North Florida is part of the stroke belt. Public Health Rep. Wash. DC 1974(107), 540–543 (1992).
Liao, Y., Greenlund, K. J., Croft, J. B., Keenan, N. L. & Giles, W. H. Factors explaining excess stroke prevalence in the US stroke belt. Stroke 40, 3336–3341 (2009).
Wade, D. T. & Hewer, R. L. Functional abilities after stroke: measurement, natural history and prognosis. J. Neurol. Neurosurg. Psychiatry 50, 177–182 (1987).
Robinson, C. A., Shumway-Cook, A., Ciol, M. A. & Kartin, D. Participation in community walking following stroke: Subjective versus objective measures and the impact of personal factors. Phys. Ther. 91, 1865–1876 (2011).
Clark, D. J. et al. Sympathetic nervous system activity measured by skin conductance quantifies the challenge of walking adaptability tasks after stroke. Gait Posture 60, 148–153 (2018).
D’souza, J., Natarajan, M. & Kumaran, D. Does the environment cause changes in hemiparetic lower limb muscle activity and gait velocity during walking in stroke survivors?. J. Stroke Cerebrovasc. Dis. 29, 105174 (2020).
Robinson, C. A., Matsuda, P. N., Ciol, M. A. & Shumway-Cook, A. Participation in community walking following stroke: The influence of self-perceived environmental barriers. Phys. Ther. 93, 620–627 (2013).
Chatterjee, S. A., Rose, D. K., Porges, E. C., Otzel, D. M. & Clark, D. J. A perspective on objective measurement of the perceived challenge of walking. Front. Hum. Neurosci. 13, 161 (2019).
Larén, A., Odqvist, A., Hansson, P.-O. & Persson, C. U. Fear of falling in acute stroke: The Fall Study of Gothenburg (FallsGOT). Top. Stroke Rehabil. 25, 256–260 (2018).
Schmid, A. A. & Rittman, M. Fear of falling: An emerging issue after stroke. Top. Stroke Rehabil. 14, 46–55 (2007).
Friedman, S. M., Munoz, B., West, S. K., Ruben, G. S. & Fried, L. P. Falls and fear of falling: Which comes first? A longitudinal secondary prevention. J. Am. Geriatr. Soc. 50, 1329–1335 (2002).
Schmid, A. A. et al. Balance and balance self-efficacy are associated with activity and participation after stroke: A cross-sectional study in people with chronic stroke. Arch. Phys. Med. Rehabil. 93, 1101–1107 (2012).
Durcan, S., Flavin, E. & Horgan, F. Factors associated with community ambulation in chronic stroke. Disabil. Rehabil. 38, 245–249 (2016).
French, M. A., Moore, M. F., Pohlig, R. & Reisman, D. Self-efficacy mediates the relationship between balance/walking performance, activity, and participation after stroke. Top. Stroke Rehabil. 23, 77–83 (2016).
Danks, K. A., Pohlig, R. T., Roos, M., Wright, T. R. & Reisman, D. S. Relationship between walking capacity, biopsychosocial factors, self-efficacy, and walking activity in persons poststroke. J. Neurol. Phys. Ther. 40, 232–238 (2016).
Miller, A., Pohlig, R. T., Wright, T., Kim, H. E. & Reisman, D. S. Beyond physical capacity: Factors associated with real-world walking activity after stroke. Arch. Phys. Med. Rehabil. https://doi.org/10.1016/j.apmr.2021.03.023 (2021).
Liu, T.-W., Ng, S. S., Kwong, P. W. & Ng, G. Y. Fear avoidance behavior, not walking endurance, predicts the community reintegration of community-dwelling stroke survivors. Arch. Phys. Med. Rehabil. 96, 1684–1690 (2015).
Pang, M. Y., Eng, J. J. & Miller, W. C. Determinants of satisfaction with community reintegration in older adults with chronic stroke: Role of balance self-efficacy. Phys. Ther. 87, 282–291 (2007).
Robinson, C. A., Shumway-Cook, A., Matsuda, P. N. & Ciol, M. A. Understanding physical factors associated with participation in community ambulation following stroke. Disabil. Rehabil. 33, 1033–1042 (2011).
Lord, S. E., McPherson, K., McNaughton, H. K., Rochester, L. & Weatherall, M. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive?. Arch. Phys. Med. Rehabil. 85, 234–239 (2004).
Barclay, R. E. et al. Interventions for improving community ambulation in individuals with stroke. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD010200.pub2 (2015).
Tinetti, M. E., Richman, D. & Powell, L. Falls efficacy as a measure of fear of falling. J. Gerontol. 45, P239–P243 (1990).
Botner, E. M., Miller, W. C. & Eng, J. J. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil. Rehabil. 27, 156–163 (2005).
Donaldson, S. I. & Grant-Vallone, E. J. Understanding self-report bias in organizational behavior research. J. Bus. Psychol. 17, 245–260 (2002).
Paulhus, D. L. & Vazire, S. The self-report method. In Handbook of Research Methods in Personality Psychology 224–239 (The Guilford Press, 2007).
Dawson, M. E., Schell, A. M. & Courtney, C. G. The skin conductance response, anticipation, and decision-making. J. Neurosci. Psychol. Econ. 4, 111–116 (2011).
Clark, D. J., Rose, D. K., Ring, S. A. & Porges, E. C. Utilization of central nervous system resources for preparation and performance of complex walking tasks in older adults. Front. Aging Neurosci. 6, 1–9 (2014).
Adkin, A. L., Frank, J. S., Carpenter, M. G. & Peysar, G. W. Fear of falling modifies anticipatory postural control. Exp. Brain Res. 143, 160–170 (2002).
Critchley, H. D. Review: Electrodermal responses: What happens in the brain. The Neuroscientist 8, 132–142 (2002).
Yoon, S., Sim, J. K. & Cho, Y.-H. A flexible and wearable human stress monitoring patch. Sci. Rep. 6, 23468 (2016).
Zygmunt, A. & Stanczyk, J. Methods of evaluation of autonomic nervous system function. Arch. Med. Sci. AMS 6, 11–18 (2010).
Song, C., Ikei, H., Kagawa, T. & Miyazaki, Y. Effects of walking in a forest on young women. Int. J. Environ. Res. Public. Health 16, 229 (2019).
Song, C. et al. Physiological and psychological responses of young males during spring-time walks in urban parks. J. Physiol. Anthropol. 33, 8 (2014).
Kreibig, S. D., Wilhelm, F. H., Roth, W. T. & Gross, J. J. Cardiovascular, electrodermal, and respiratory response patterns to fear- and sadness-inducing films. Psychophysiology 44, 787–806 (2007).
Ghiasi, S., Greco, A., Barbieri, R., Scilingo, E. P. & Valenza, G. Assessing autonomic function from electrodermal activity and heart rate variability during cold-pressor test and emotional challenge. Sci. Rep. 10, 5406 (2020).
Chatterjee, S. A. et al. Mobility function and recovery after stroke: Preliminary insights from sympathetic nervous system activity. J. Neurol. Phys. Ther. JNPT 42, 224–232 (2018).
Outermans, J., Pool, J., van de Port, I., Bakers, J. & Wittink, H. What’s keeping people after stroke from walking outdoors to become physically active? A qualitative study, using an integrated biomedical and behavioral theory of functioning and disability. BMC Neurol. 16, 137–137 (2016).
Fulk, G. D. & Sazonov, E. Using sensors to measure activity in people with stroke. Top. Stroke Rehabil. 18, 746–757 (2011).
Fulk, G. D., He, Y., Boyne, P. & Dunning, K. Predicting home and community walking activity poststroke. Stroke 48, 406–411 (2017).
Hanke, T. A. et al. Measuring community mobility in survivors of stroke using global positioning system technology: A prospective observational study. J. Neurol. Phys. Ther. 43, 175–185 (2019).
McCluskey, A., Ada, L., Dean, C. M. & Vargas, J. Feasibility and validity of a wearable GPS device for measuring outings after stroke. ISRN Rehabil. 2012, 1–8 (2012).
Mahendran, N., Kuys, S. S. & Brauer, S. G. Accelerometer and global positioning system measurement of recovery of community ambulation across the first 6 months after stroke: An exploratory prospective study. Arch. Phys. Med. Rehabil. 97, 1465–1472 (2016).
Stokic, D. S., Horn, T. S., Ramshur, J. M. & Chow, J. W. Agreement between temporospatial gait parameters of an electronic walkway and a motion capture system in healthy and chronic stroke populations. Am. J. Phys. Med. Rehabil. 88, 437–444 (2009).
Statement, A. T. S. Am. J. Respir. Crit. Care Med. 166, 111–117 (2002).
Danielsson, A., Willén, C. & Sunnerhagen, K. S. Is walking endurance associated with activity and participation late after stroke??. Disabil. Rehabil. 33, 2053–2057 (2011).
Awad, L. N., Reisman, D. S., Pohlig, R. T. & Binder-Macleod, S. A. Reducing the cost of transport and increasing walking distance after stroke: A randomized controlled trial on fast locomotor training combined with functional electrical stimulation. Neurorehabil. Neural Repair 30, 661–670 (2016).
Cheng, D. K., Nelson, M., Brooks, D. & Salbach, N. M. Validation of stroke-specific protocols for the 10-meter walk test and 6-minute walk test conducted using 15-meter and 30-meter walkways. Top. Stroke Rehabil. 27, 251–261 (2020).
Illigens, B. M. W. & Gibbons, C. H. Sweat testing to evaluate autonomic function. Clin. Auton. Res. 19, 79–87 (2009).
Boucsein, W. et al. Publication recommendations for electrodermal measurements. Psychophysiology 49, 1017–1034 (2012).
Haeuber, E., Shaughnessy, M., Forrester, L. W., Coleman, K. L. & Macko, R. F. Accelerometer monitoring of home- and community-based ambulatory activity after stroke1. Arch. Phys. Med. Rehabil. 85, 1997–2001 (2004).
Mudge, S., Stott, N. S. & Walt, S. E. Criterion validity of the StepWatch Activity Monitor as a measure of walking activity in patients after stroke. Arch. Phys. Med. Rehabil. 88, 1710–1715 (2007).
Noury-Desvaux, B. et al. The accuracy of a simple, low-cost GPS data logger/receiver to study outdoor human walking in view of health and clinical studies. PLoS ONE 6, e23027–e23027 (2011).
www.globalsat.com.tw. GPS Data Logger, DG-500 - GlobalSat WorldCom Corp. https://www.globalsat.com.tw/style/Frame/m5/product_detail.asp?customer_id=909&lang=2&content_set=color_2&name_id=51263&Directory_ID=30784&id=199320.
Gernigon, M., Le Faucheur, A., Noury-Desvaux, B., Mahe, G. & Abraham, P. Applicability of global positioning system for the assessment of walking ability in patients with arterial claudication. J. Vasc. Surg. 60, 973-981.e1 (2014).
Knarr, B., Roos, M. A. & Reisman, D. S. Sampling frequency impacts measurement of walking activity after stroke. J. Rehabil. Res. Dev. 50, 1107–1112 (2013).
Barak, S., Wu, S. S., Dai, Y., Duncan, P. W. & Behrman, A. L. Adherence to accelerometry measurement of community ambulation poststroke. Phys. Ther. 94, 101–110 (2014).
Stacking Up Yard Sizes by State. Realtor Magazine https://magazine.realtor/daily-news/2018/10/16/stacking-up-yard-sizes-by-state (2018).
Ghasemi, A. & Zahediasl, S. Normality tests for statistical analysis: A guide for non-statisticians. Int. J. Endocrinol. Metab. 10, 486–489 (2012).
Sebastian, D. R. et al. Associations between objectively measured physical activity, sedentary time, and cardiorespiratory fitness with inflammatory and oxidative stress markers and heart rate variability. J. Public Health Res. 11, 22799036221106580 (2022).
dos Santos, R. R. et al. Sedentary behavior: A key component in the interaction between an integrated lifestyle approach and cardiac autonomic function in active young men. Int. J. Environ. Res. Public. Health 16, 2156 (2019).
Zaffalon Júnior, J. R., Viana, A. O., de Melo, G. E. L. & De Angelis, K. The impact of sedentarism on heart rate variability (HRV) at rest and in response to mental stress in young women. Physiol. Rep. 6, e13873 (2018).
Fitzsimons, C. F. et al. Stroke survivors’ perceptions of their sedentary behaviours three months after stroke. Disabil. Rehabil. 44, 382–394 (2020).
Andrews, A. W. et al. Update on distance and velocity requirements for community ambulation. J. Geriatr. Phys. Ther. 2001(33), 128–134 (2010).
Balasubramanian, C. K., Clark, D. J. & Fox, E. J. Walking adaptability after a stroke and its assessment in clinical settings. Stroke Res. Treat. 2014, 1–21 (2014).
de Rooij, I. J. M., van de Port, I. G. L., van der Heijden, L. L. M., Meijer, J.-W.G. & Visser-Meily, J. M. A. Perceived barriers and facilitators for gait-related participation in people after stroke: From a patients’ perspective. Physiother. Theory Pract. https://doi.org/10.1080/09593985.2019.1698085 (2019).
Cho, E., Wakeling, J. M., Pousett, B. & Pollock, C. L. Mapping of electrodermal activity (EDA) during outdoor community-level mobility tasks in individuals with lower-limb amputation. J. Rehabil. Assist. Technol. Eng. 8, 1106837 (2021).
Olawale, O. A., Usman, J. S., Oke, K. I. & Osundiya, O. C. Evaluation of predictive factors influencing community reintegration in adult patients with stroke. J. Neurosci. Rural Pract. 09, 6–10 (2018).
Sánchez-Sánchez, M. L. et al. Association of barriers, fear of falling and fatigue with objectively measured physical activity and sedentary behavior in chronic stroke. J. Clin. Med. 10, 1320 (2021).
Kleckner, I. R., Feldman, M. J., Goodwin, M. S. & Quigley, K. S. Framework for selecting and benchmarking mobile devices in psychophysiological research. Behav. Res. Methods 53, 518–535 (2021).
Lang, C. E., Barth, J., Holleran, C. L., Konrad, J. D. & Bland, M. D. Implementation of wearable sensing technology for movement: Pushing forward into the routine physical rehabilitation care field. Sensors 20, E5744 (2020).
Delbaere, K. & Hadjistavropoulos, T. Commentary on: “Mobility function and recovery after stroke: Preliminary insights from sympathetic nervous system activity”. J. Neurol. Phys. Ther. 42, 233–234 (2018).
Acknowledgements
We would like to express our gratitude to Drs. Christopher Janelle and Sudeshna Chatterjee for their expert guidance in this project. We thank Kayla Borgela and De Miller Sellers for their assistance with participant recruitment and data collection as well as Michael Monaldi for developing the MATLAB code used for the SAM-GPS data analysis in this paper.
Funding
This work was supported by the Veterans Affairs Rehabilitation Research and Development grants (B3336-P and 0419BRRC-04), and Brooks-Public Health and Health Professions (PHHP) Collaboration.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualization, methodology, reviewing, and editing the manuscript. D.K.R. and K.B. conducted the investigation in this project. K.B. and D.J.C. worked on the MATLAB software code, formal analysis as well as validation of the analyzed data. K.B. wrote the original draft and prepared the figures and tables of this manuscript (using GraphPad Prism Version 9). D.K.R. and D.J.C. provided resources for the project. D.K.R. and E.J.F. provided supervision and project administration. D.K.R. lead the project through funding acquisition and data curation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bansal, K., Clark, D.J., Fox, E.J. et al. Sympathetic nervous system responses during complex walking tasks and community ambulation post-stroke. Sci Rep 13, 20068 (2023). https://doi.org/10.1038/s41598-023-47365-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47365-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.