Abstract
Although most patients recover from COVID-19, it has been linked to cardiac, pulmonary, and neurologic complications. Despite not having formal criteria for its diagnosis, COVID-19 associated cardiomyopathy has been observed in several studies through biomarkers and imaging. This study aims to estimate the proportion of COVID-19 patients with cardiac abnormalities and to determine the association between the cardiac abnormalities in COVID-19 patients and disease severity and mortality. Observational studies published from December 1, 2019 to September 30, 2020 were obtained from electronic databases (PubMed, Embase, Cochrane Library, CNKI) and preprint servers (medRxiv, bioRxiv, ChinaXiv). Studies that have data on prevalence were included in the calculation of the pooled prevalence, while studies with comparison group were included in the calculation of the odds ratio. If multiple tests were done in the same study yielding different prevalence values, the largest one was used as the measure of prevalence of that particular study. Metafor using R software package version 4.0.2 was used for the meta-analysis. A total of 400 records were retrieved from database search, with 24 articles included in the final analysis. Pooled prevalence of cardiac abnormalities in 20 studies was calculated to be 0.31 [95% Confidence Intervals (CI) of (0.23; 0.41)], with statistically significant heterogeneity (percentage of variation or I-squared statistic I2 = 97%, p < 0.01). Pooled analysis of 19 studies showed an overall odds ratio (OR) of 6.87 [95%-CI (3.92; 12.05)] for cardiac abnormalities associated with disease severity and mortality, with statistically significant heterogeneity (I2 = 85%, between-study variance or tau-squared statistic τ2 = 1.1485, p < 0.01). Due to the high uncertainty in the pooled prevalence of cardiac abnormalities and the unquantifiable magnitude of risk (although an increased risk is certain) for severity or mortality among COVID-19 patients, much more long-term prognostic studies are needed to check for the long-term complications of COVID-19 and formalize definitive criteria of “COVID-19 associated cardiomyopathy”.
Similar content being viewed by others
Introduction
Coronavirus Disease 2019 (COVID-19), caused by the novel virus Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has evidently spread throughout the world, claiming at least 1.1 million lives as of this writing1. While much of information regarding this pathogen, such as its transmission dynamics, spectrum of clinical manifestations, complications, diagnostics, and treatment have been determined.
Meanwhile, short-term and long-term effects of COVID-19 are still being elucidated. Although majority of the COVID-19 cases are mild and asymptomatic, and most patients recover from the disease, COVID-19 has been linked to cardiac, pulmonary and neurologic complications. As of this writing, there are reports of cardiac abnormalities and dysfunction, detected through biomarkers and imaging, among mild, moderate, severe, critical, and even recovered cases.
Cardiac pathology caused by SARS-CoV-2 has been documented in vitro2, and it was observed to be associated with worse outcomes. However, due to the variability in the overabundance of various prognostic studies, the definite proportion or frequency of this occurring among patients, and the definite magnitude of risk for severity and mortality have yet to be fully elucidated. There is also no definite criteria or formal definition of COVID-19 associated cardiomyopathy.
This study aims to estimate the proportion of COVID-19 patients with cardiac abnormalities and to determine the association between the cardiac abnormalities in COVID-19 patients and disease severity and mortality.
Methodology
Research question formulation, inclusion and exclusion criteria
The population of interest includes patients with laboratory-confirmed COVID-19 patients. The identified exposure is any form of cardiac abnormality found in diagnostic tests such as echocardiography, cardiac magnetic resonance imaging, electrocardiogram, and serum biomarkers such as troponin. These were compared to confirmed COVID-19 patients who have no abnormalities in aforementioned cardiac tests. The main outcomes of interest were severity, in-hospital mortality, or both. Both prospective and retrospective observational studies (cohort studies, case–control studies, case series) and randomized controlled studies were included, while all other study designs, such as case reports, commentaries, editorials, guidelines, reviews, and studies published only as abstracts were excluded.
Literature search strategy
Comprehensive searches of electronic databases (PubMed, Embase, Cochrane Library, CNKI) and preprint servers (medRxiv, bioRxiv, ChinaXiv) were conducted, including studies published from December 1, 2019 to September 30, 2020 in both English and non-English languages. In the case of PubMed, search words include ("2019 nCoV" OR "2019nCoV" OR "2019-nCoV" OR "COVID 19" OR "COVID19" OR "COVID-19" OR "new coronavirus" OR "novel coronavirus" OR (Wuhan AND coronavirus) OR (Wuhan AND pneumonia) OR "SARS-CoV" OR "SARS-CoV-2" OR "SARS CoV-2"), ("troponin" OR "cardiac" OR "myocardial" OR "TnI" OR "TnT" OR "cardiovascular" OR "heart" OR "CMR" OR "cardiac MRI" OR "cardiac magnetic resonance imaging" OR "echocardiography" OR "BNP" OR "brain natiuretic peptide" OR "NT-proBNP"). In the Cochrane Library, search words include ("COVID-19" OR "coronavirus" OR "2019-nCoV") AND ("cardiac" OR "cardiovascular" OR "myocardial" OR "troponin" OR "echocardiography" OR "BNP" OR "NT-proBNP" OR "cardiac MRI" OR "CMR"). In Chinese electronic databases, keywords include 新型冠状病毒, 心机损伤. Free text search in Google Scholar used the queries "COVID-19 cardiac echocardiography", "COVID-19 cardiac troponin", "COVID-19 cardiac MRI". If one search strategy, such as in the case of ChinaXiv, yielded no results, another approach was done to ensure no articles are missed out. Detailed step-by-step search strategy is elucidated in Supplementary Material 1.
Study selection
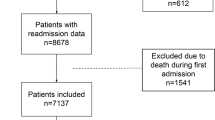
One assessor reviewed all relevant titles and abstracts independently and selected articles for full-text review if inclusion criteria are met. Full-text review and appraisal was done by two assessors. Disagreements were resolved by discussion between the two reviewers; a third person was involved when consensus cannot be reached (Fig. 1).
Data extraction
The following data from each study were extracted: first author’s name, study design, population type (whether only severe and critical cases are included, or even mild and moderate cases are included), diagnostic methods for cardiac abnormalities, frequency of cardiac abnormalities, and frequencies of severity and mortality among patients with and without the aforementioned cardiac abnormalities. Studies that have data on prevalence were included in the calculation of the pooled prevalence, while studies with comparison group were included in the calculation of the odds ratio. If multiple tests were done in the same study yielding different prevalence values, the largest one was used as the measure of prevalence of that particular study.
Risk of bias (quality) assessment for prognosis studies
Two reviewers independently assessed the quality of the included studies using the framework by Dans et al.3 that uses the following signaling questions answerable by a “Yes” or “No”:
-
Were all important prognostic factors considered?
-
Were unbiased criteria used to detect the outcome in all patients?
-
Was follow-up rate adequate?
-
If clinical prediction rules are being tested, was a separate validation study done?
Results from these ratings and especially non-agreement were then the basis for discussion until final consensus is made.
Strategy for data synthesis
Meta-analysis software, Metafor (R package) by Viechtbauer4 using R software package version 4.0.2, was used in this study. Heterogeneity among the studies was assessed using the Cochran's Q and I2 statistics. Cochran’s Q is the result of the Chi-squared test of several studies5. At 0.10 significance level, p-values < 0.10 indicate rejection of the hypothesis that the measures of association are similar5. The I2 statistic represents the percentage of variability in effect estimates due to real dispersion among the studies5. I2 of at least 50% is considered substantial heterogeneity; it means that at least half of the total variability among effect sizes is due to true heterogeneity between studies5. The tau-squared statistic is a function of I2.
Random effects models6 were used to account for the heterogeneity of included studies. In studies with zero count for events in either the exposure or comparator group, 0.5 was automatically added in all counts6. Pooled prevalence of cardiac abnormalities was estimated at 95% confidence level using the Logit Transformation Method and Clopper–Pearson Intervals respectively. The Logit Transformation Method was used to estimate the pooled prevalence by log-transforming the prevalences of the individual studies7. The Clopper–Pearson Intervals, or more commonly known as the exact binomial test, calculates the confidence intervals based on the binomial distribution and therefore produces more conservative estimates and wide confidence intervals8, 9.
Pooled odds ratios and 95%-CI were calculated using the DerSimonian–Laird Method. The DerSimonian–Laird Method adjusts the standard errors of the individual odds ratios to incorporate variations across different studies10, producing wider confidence intervals.
A funnel plot, together with Egger’s Test, was used to determine potential publication bias. The results—the intercept, its confidence intervals—represent the degree of asymmetry of the funnel plot11. The farther it is from zero, the more asymmetric is the funnel, indicating publication bias11.
Post-hoc sensitivity analyses—leave-one-out analysis and Baujat diagnostics—were also done.
Analysis of subgroups or subsets
Subgroup analyses were done according to the following.
-
(1)
Study design: case–control, cross-sectional, and cohort studies;
-
(2)
Study population: studies that included only severe and critical patients, and studies that included mild, moderate, severe, and critical patients as defined by the World Health Organization Interim Guidelines for the Clinical Management of COVID-19, or Novel Coronavirus Infectious Pneumonia Management Guidelines by the People’s Republic of China Central Health Committee; and
-
(3)
Type of cardiac test done.
Results
Study selection
From the database search, 294 articles were retrieved and additional 120 studies were identified through Google Scholar, giving a total of 400 studies after 14 duplicates were removed. After screening articles by title, 306 articles were excluded because 281 articles are not relevant or did not satisfy the inclusion criteria, and 25 articles were letters, editorials, protocol summaries, or reviews, leaving only 94 articles. After screening articles by abstract, 25 articles were excluded because 19 articles were not relevant, and 6 articles were letters, editorials, protocol summaries, or reviews. 69 articles then underwent full-text screening, thus excluding 45 articles, all of which do not have the relevant population, exposure, or outcome parameters. This leaves 24 articles to be included in the final analysis. 20 articles are included in estimation of the pooled prevalence, and 19 articles are included in the meta-analysis of odds ratios.
Summary of characteristics of included studies
Among 24 papers included in the final analysis, there are four case–control studies, two cross-sectional studies, and 18 cohort studies. All studies were done in a hospitalized setting. Deng et al. had analysis on both severity and mortality. Most of these studies involved multiple cardiac biomarkers. More details of the included studies are found in Table 1.
Summary of appraisal of included papers
Two (2) studies—Knight et al. and Li et al.—have unclear risk of bias because it is unclear whether they have considered all important prognostic factors (D1). The rest have low risk of bias overall. The risk of bias assessment traffic light plot can be seen in Supplementary Material 2.
The major weaknesses of these studies lie in their retrospective design, questionable temporality (as some are cross-sectional and case–control), different and sometimes unclear thresholds to define an “abnormal cardiac test”.
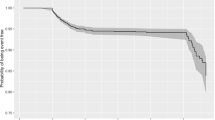
Pooled prevalence calculation
A total of 20 studies (two cross-sectional studies and 18 cohort studies) were included in the calculation of pooled prevalence, yielding a total of 4393 patients, 1040 of whom had at least one abnormal result in a cardiac test. Pooled prevalence is at 0.31 [95%-CI (0.23; 0.41)] (Fig. 2). Heterogeneity was statistically significant with I2 = 97%, τ2 = 0.9373, p < 0.01.
Subgroup analysis according to study design
Breaking this down further according to study design, cohort studies report a pooled prevalence of 0.33 [95%-CI (0.23; 0.44)], and cross-sectional studies report a pooled prevalence of 0.22 [95%-CI (0.12, 0.36)]. Likewise, heterogeneity is significant for both subgroups, with I2 = 97%, τ2 = 0.9919, p < 0.01 in cohort studies and I2 = 86%, τ2 = 0.2124, p < 0.01 (Fig. 2).
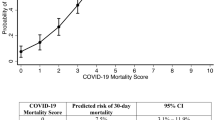
Association of cardiac abnormalities with disease severity and mortality
A total of 19 studies (two cross-sectional, three case–control, and 14 cohort studies) were included in the calculation of odds ratios. Pooled analysis of 19 studies showed an overall odds ratio (OR) of 6.87 [95%-CI (3.92; 12.05)] (Fig. 3) with significant heterogeneity (I2 = 85%, τ2 = 1.1485, p < 0.01).
Subgroup analysis according to study design
Further subgroup analysis according to study design showed: (1) for cohort studies, an OR of 5.68 [95%-CI (3.21; 10.06)] with significant heterogeneity (I2 = 78, τ2 = 0.8013, p < 0.01); (2) for cross-sectional studies, an OR of 4.78 [95%-CI (0.62; 36.75)] with significant heterogeneity (I2 = 85, τ2 = 1.8368, p < 0.01); and (3) for case control studies, an OR of 18.58 [95%-CI (2.88; 120.00)] with significant heterogeneity (I2 = 92%, τ2 = 2.1723, p < 0.01).
Subgroup analysis according to the type of test
Further subgroup analysis according to the type of test showed: for Troponin I (TnI), an OR of 12.43 [95%-CI (2.44; 19.77)] with significant heterogeneity (I2 = 94%, τ2 = 3.0468, p < 0.01); for NT-proBNP, an OR of 12.43 [95%-CI (5.69; 27.15)] with minimal heterogeneity (I2 = 1%, τ2 = 0.0035, p = 0.37); for 2D Echocardiography, an OR of 2.79 [95%-CI (1.12; 6.94)] with significant heterogeneity (I2 = 58%, τ2 = 0.4984, p = 0.07); for Troponin T (TnT), an OR of 8.06 [95%-CI (5.06; 12.83)] with minimal heterogeneity (I2 = 0%, τ2 = 0, p = 0.70); and for Creatinine Kinase (CK), an OR of 3.64 [95%-CI (2.04; 6.50)] with minimal heterogeneity (I2 = 0%, τ2 = 0, p = 0.33) (Fig. 4). Only one study was noted for BNP, ECG, and myoglobin; hence, the pooled OR and the heterogeneity could not be obtained.
Publication bias of included studies
A funnel plot of the studies showed little to no publication bias (Fig. 5A). Egger’s Test likewise showed no significant publication bias nor funnel asymmetry, with Intercept = 1.347 [95%-CI (− 1.18; 3.87)], t = 1.045, p = 0.31.
(A) Funnel plot of all included studies show a relative paucity of studies with smaller sample sizes and lesser odds ratios (lower-left region). (B) Baujat plot of all studies included in the estimation of the pooled odds ratio. (C) Baujat plot of all cohort studies included in the estimation of the pooled odds ratio.
Heterogeneity and sensitivity analysis
Post-hoc sensitivity analysis was done using methods available in dmetar12 and metafor R packages4. Among all studies included in the estimation of the pooled odds ratio (OR), McCullough et al. and Nie et al. were identified to be outliers (Supplementary Material 3). Leave-one-out analysis also show that these two studies contribute a significant fraction of the heterogeneity. Excluding Nie et al. would lead to OR of 5.700 [95%-CI (3.535; 9.191)], with I2 = 76.6%. Excluding McCullough et al. would lead to OR of 7.545 [95%-CI (4.319; 13.180)], with I2 = 81.3%. Baujat diagnostics (Fig. 5B) show that Nie et al. and McCullough et al. contribute to 43.3% and 22.7% of the heterogeneity respectively, totaling to 66% (Supplementary Material 3). Nie et al. used a case–control study design, which has inherent sampling and selection bias. McCullough et al. on the other hand used ECG to define an abnormal cardiac finding. Among all cohort studies included in the estimation of the pooled odds ratio (OR), Shi et al. was identified to be the outlier (Supplementary Material 3). Excluding Shi et al. would lead to OR of 4.725 [95%-CI (2.850; 7.834)], with I2 = 67.9. Baujat diagnostics (Fig. 5C) show that Shi et al. and McCullough et al. contribute to 20.2% and 11.6% of the heterogeneity respectively, totaling to 31.8% (Supplementary Material 3). Shi et al. is the only study that used myoglobin as a biomarker for cardiac abnormality.
Discussion
The substantial heterogeneity among studies precludes any definitive conclusion on the magnitude of risk or odds ratio of severity or mortality associated with any abnormal cardiac finding in any given test. Nevertheless, subgroup analyses of certain cardiac biomarkers—namely, CK, Troponin T, NT-proBNP, as well as Troponin I (if the case–control study by Nie et al. is removed)—show more reliable odds ratios with their nonsignificant heterogeneity. All forest plots show a clear trend towards definite increase in mortality or severity risk among COVID-19 patients exposed to a positive finding in any cardiac abnormality test.
Implications of the study findings
In another meta-analysis of 35 studies13, the pooled frequency of acute cardiac injury among COVID-19 patients was at 25.3%, which is within the bounds of the 95% confidence interval estimated by this study, between 23 and 41%. Hypertension is the most common pre-existing comorbidity in these patients with a pooled frequency of 29.2% (95%-CI 24.7; 33.6%), followed by diabetes with a pooled frequency of 13.5% (95%-CI 11.5; 15.4%)13. Overall, fewer than one-fifth of patients had pre-existing cardiovascular diseases, at 12.6% (95%-CI 10.0; 15.2%). The risk of mortality in the presence of acute cardiac injury is increased by nearly 20 times [OR = 19.64; 95%-CI (10.28, 37.53). The heterogeneity of the studies included is also moderately to highly significant; reasons for this were not detailed in the said study. There are currently little to no studies on cardiac abnormalities on only mild and moderate COVID-19 cases as these cases are likely treated on an outpatient basis. Due to overwhelmed health systems in most countries where these studies are done, mild and moderate cases are not given enough attention nor any form of cardiac biomarker screening.
In this study, a pooled odds ratio of 6.87 [95%-CI (3.92; 12.05)] means that, the COVID-19 patients with an abnormal cardiac test are 6.87 times more likely to die or have severe disease than COVID-19 patients without an abnormal cardiac test. At a 5% level of significance, the odds of dying ranges from at least four (4) times to at most twelve (12) times. Nie et al., McCullough et al., and Shi et al. are found to be outlier studies because they used a case–control study design, an ECG finding to define a cardiac abnormality, and serum myoglobin to define a cardiac abnormality respectively. Meanwhile, the Egger’s test showing no significant publication bias means that this pooled odds ratio is sufficiently exhaustive. Newer, larger, longer-term studies are necessary to significantly alter this result.
With regards to severity, persistent symptoms have been reported even after recovery from COVID-19, and this has been linked to cardiac, pulmonary, and neurologic complications14. In a study of 143 patients who recovered from COVID-1914, 87.4% reported persistence of at least fatigue or dyspnea. In another study of 100 recovered COVID-19 patients15, high-sensitivity troponin T (hsTnt) was detectable (3 pg/mL or greater) in 71 patients (71%) and significantly elevated (13.9 pg/mL or greater) in 5 patients (5%). In the same study15, 78 patients (78%) had abnormal CMR findings, and endomyocardial biopsy in patients with severe findings revealed active lymphocytic inflammation. These may all contribute to an emerging picture of an emerging epidemic of “COVID-19 associated cardiomyopathy” which may affect survivors who had mild, moderate, severe, or critical COVID-19.
The findings in this meta-analysis may provide an explanation for anecdotal reports of outside-hospital sudden deaths and increasing rates of COVID-19 “recoveries” turning into “deaths”, and more severe disease and more deaths from other comorbid conditions among COVID-19 survivors.
The pooled odds ratio for severity or mortality is but merely a single point estimate of a very fat-tailed risk due to the significant heterogeneity of the included studies, making it necessarily insufficient to give us any definite information for screening efforts16. However, there is no doubt on the precautionary principle that should be taken into consideration in implementing policies of recovery and/or follow-up. The risk for severity or mortality across all analyses presented here are asymmetrical and right-skewed. Related distribution of fatalities of pandemic outbreaks in the past 2500 years is strongly fat-tailed17. What we are dealing here is an “infectious” form of supposedly the most common cause of death worldwide—cardiac disease that is “infectious”, so to speak.
Limitations of the study
The authors faced a major challenge in disaggregating the data of each study; hence, studies are pooled together even with different study designs. Some studies have data on prevalence but not on odds ratio. Some studies have multiple tests performed. Thus, only the maximum count of the stated outcome of the study—cardiac abnormalities found through any one of the tests—is considered in calculating the pooled prevalence and odds ratio. Consequently, subgroup analyses were performed based on the specific type of test in order to address this limitation; however, the heterogeneity did not fully disappear.
The varying tests and their varying cut-off measures for the definition of a “positive finding” in each individual study likely contributes to a significant portion in the heterogeneity even among the smaller studies. This is an understandable phenomenon given the fact that information is still evolving. Some measures may have reduced validity due to the excessive inflammation in COVID-19, which may cause spuriously high levels of serum biomarkers. Therefore, we propose more studies that will eventually formalize a unified definition or diagnostic criteria for “COVID-19 cardiomyopathy”.
Conclusion
Despite significant heterogeneity in most comparisons, there is a trend towards definite increase in mortality or severity risk among COVID-19 patients with any cardiac abnormality test.
Due to the high uncertainty in the pooled prevalence and/or incidence of cardiac abnormalities and the unquantifiable magnitude of risk (although an increased risk is certain) for severity or mortality among COVID-19 patients, much more long-term prognostic studies are needed to check for the long-term complications of COVID-19 and formalize definitive criteria of “COVID-19 associated cardiomyopathy”. By defining clear criteria, or by defining a specific test for the detection of any cardiac abnormality, the magnitude of risk can be better measured. Long-term prognostic studies using a defined criteria of “COVID-19 associated cardiomyopathy” on recovered patients should be done.
References
Coronavirus Update (Live): 41,017,115 Cases and 1,128,779 Deaths from COVID-19 Virus Pandemic—Worldometer. Worldometers.info. (2020). https://www.worldometers.info/coronavirus/. (Accessed 20 October 2020).
Pérez-Bermejo, J. A. et al. SARS-CoV-2 infection of human IPSC-derived cardiac cells predicts novel cytopathic features in hearts of COVID-19 patients. Cold Spring Harbor Lab. https://doi.org/10.1101/2020.08.25.265561 (2020).
Dans, A., Dans, L. & Silvestre, M. Painless Evidence-Based Medicine 2nd edn. (Wiley, 2017).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36(3), 1–48 (2010).
Aromataris, E., Munn, Z. (eds.). JBI Manual for Evidence Synthesis. JBI, 2020. https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-01.
Deeks, J.J., Higgins, J.P.T., Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (eds.). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane http://www.training.cochrane.org/handbook (2021).
Stijnen, T., Hamza, T. H. & Ozdemir, P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat. Med. 29(29), 3046–3067. https://doi.org/10.1002/sim.4040 (2010) (PMID: 20827667).
Clopper, C. & Pearson, E. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26(4), 404–413. https://doi.org/10.1093/biomet/26.4.404 (1934).
Agresti, A. & Coull, B. Approximate is better than “exact” for interval estimation of binomial proportions. The American Statistician 52, 119. https://doi.org/10.2307/2685469 (1998).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials. 7(3), 177–188. https://doi.org/10.1016/0197-2456(86)90046-2 (1986) (PMID: 3802833).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629. https://doi.org/10.1136/bmj.315.7109.629 (1997).
Harrer, M., Cuijpers, P., Furukawa, T.A, & Ebert, D. D. Doing Meta-Analysis in R: A Hands-on Guide. Zenodo https://doi.org/10.5281/zenodo.2551803 (2019).
Momtazmanesh, S. et al. Cardiovascular disease in COVID-19: A systematic review and meta-analysis of 10,898 patients and proposal of a triage risk stratification tool. Egypt. Heart J. EHJ Off. Bull. Egypt. Soc. Cardiol. 72(1), 41. https://doi.org/10.1186/s43044-020-00075-z (2020).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA https://doi.org/10.1001/jama.2020.12603 (2020).
Puntmann, V. O. et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.3557 (2020).
Taleb, N. N., Bar-Yam, Y. & Cirillo, P. On single point forecasts for fat-tailed variables. Int. J. Forecast. https://doi.org/10.1016/j.ijforecast.2020.08.008 (2020).
Cirillo, P. & Taleb, N. N. Tail risk of contagious diseases. Nat. Phys. 16, 606–613. https://doi.org/10.1038/s41567-020-0921-x (2020).
Funding
This research was funded by the authors. No external funding agency funded this research.
Author information
Authors and Affiliations
Contributions
L.F.Dy primarily conceptualized the research, with input from R.C.V.L., I.T.G.C. and L.F.Dans. L.F.Dy and R.C.V.L. assessed the articles for risk of bias, with L.F.Dans as the third assessor in cases of lack of agreement in quality assessment. L.F.Dy performed the statistical analysis with input from L.F.Dans and C.P.C. All authors approved the final version submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dy, L.F., Lintao, R.C.V., Cordero, C.P. et al. Prevalence and prognostic associations of cardiac abnormalities among hospitalized patients with COVID-19: a systematic review and meta-analysis. Sci Rep 11, 8449 (2021). https://doi.org/10.1038/s41598-021-87961-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87961-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.