Abstract
Evidence indicates that glucose variation (GV) plays an important role in mortality of critically ill patients. We aimed to investigate the relationship between the coefficient of variation of 24-h venous blood glucose (24-hVBGCV) and mortality among patients with acute respiratory failure. The records of 1625 patients in the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) database were extracted. The 24-hVBGCV was calculated as the ratio of the standard deviation (SD) to the mean venous blood glucose level, expressed as a percentage. The outcomes included ICU mortality and in-hospital mortality. Participants were divided into three subgroups based on tertiles of 24-hVBGCV. Multivariable logistic regression models were used to evaluate the relationship between 24-hVBGCV and mortality. Sensitivity analyses were also performed in groups of patients with and without diabetes mellitus. Taking the lowest tertile as a reference, after adjustment for all the covariates, the highest tertile was significantly associated with ICU mortality [odds ratio (OR), 1.353; 95% confidence interval (CI), 1.018–1.797] and in-hospital mortality (OR, 1.319; 95% CI, 1.003–1.735), especially in the population without diabetes. The 24-hVBGCV may be associated with ICU and in-hospital mortality in patients with acute respiratory failure in the ICU, especially in those without diabetes.
Similar content being viewed by others
Introduction
Glucose variation (GV) has been identified as a risk factor for adverse outcomes in various patients1. A previous study indicated that increased standard deviation (SD) and coefficient of variation (CV), are independently associated with longer hospital stay and higher mortality in non-critically ill patients2. Besides, in critically ill patients, the higher mean absolute glucose (MAG) change over a given period or SD also conferred a strong independent risk of mortality3,4,5,6. However, the relationship between coefficient of variation of 24-h venous blood glucose (24-hVBGCV), calculated as the ratio of the SD to the mean of venous blood glucose readings available during first 24-h in ICU, and mortality among patients with acute respiratory failure in intensive care unit (ICU) remains unclear. Therefore, the present study was conducted to explore this relationship using the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC-II) database.
Results
Analysis of baseline characteristics
The baseline characteristics of the study participants are shown in Table 1. According to the tertiles of 24-hVBGCV, patients were divided into three groups. Statistically significant differences were found among the groups regarding the distribution of age (P = 0.005), SOFA score (P < 0.001), diabetes (P < 0.001), renal failure (P < 0.001), and use of insulin (P < 0.001). There was no statistical significance regarding sex, ethnicity, obesity, chronic pancreatitis, heart failure, or infection (P > 0.05). In the three groups (lowest to highest tertiles), both ICU mortality and in-hospital mortality were significantly different (ICU mortality, 25.3% vs. 32.1% vs. 37.1%, P < 0.001; in-hospital mortality, 30.7% vs. 38.0% vs. 42.1%, P < 0.001).
Relationship between 24-hVBGCV and mortality
In univariate analysis, taking the lowest tertile as a reference, the highest tertile was associated with ICU mortality (OR, 1.738; 95% CI, 1.339–2.256) and in-hospital mortality (OR, 1.640; 95% CI, 1.278–2.106). After adjustment for a series of covariates, the highest tertile was also related to higher ICU mortality (OR, 1.353; 95% CI, 1.018–1.797) and in-hospital mortality (OR, 1.319; 95% CI, 1.003–1.735), compared with the lowest tertile of 24-hVBGCV (Table 2).
Interaction and subgroup analysis
The interaction analyses were conducted between 24-hVBGCV and diabetes. However, there was no significant relationship (Pinteraction = 0.135; hospital, Pinteraction = 0.160), which indicates that whether or not patients have diabetes has no effect on the relationship between 24-hVBGCV and mortality. Considering the clinical practice, the population was also divided into two subgroups: diabetes or non-diabetes patients. Surprisingly, compared with the lowest 24-hVBGCV tertile, the highest tertile was associated with ICU mortality (OR, 1.453; 95% CI, 1.050–2.010) and in-hospital mortality (OR, 1.382; 95% CI, 1.012–1.888) in non-diabetes patients after adjusting for all the covariates (Table 3).
Discussion
Many studies have shown that increased MAG change per hour or SD was independently associated with length of ICU stay and mortality in critically ill patients3,5. In the present study, we used CV of 24-h venous blood glucose to evaluate the blood GV. Our findings suggest that higher 24-hVBGCV was associated with ICU and in-hospital mortality in patients with acute respiratory failure after adjusting for a series of variables, especially in non-diabetes patients.
Previous studies have focused on the relationship between GV and mortality2,3,7,8,9. By measuring MAG change per hour from 5728 ICU patients in a retrospective cohort3, Hermanides J et al. concluded that high MAG variation was strongly associated with increased ICU and in-hospital death; conversely, low GV seemed to have a protective effect, even when mean glucose levels remained elevated. Collecting all glucose values for every patient during the stay in hospital to calculate the mean glucose, Krinsley et al.5 found that high GV, calculated by the SD of each patient’s mean absolute glucose level, has an effect on mortality in critically ill adult patients. High SD of glucose may serve as an independent risk factor of ICU mortality10. Recently, a prospective observational study11, in which GV was calculated as the CV of blood glucose (derived as a percentage of SD to mean blood glucose during the entire ICU stay), also confirmed that patients with lower GV had lower ICU/in-hospital mortality than those with higher GV. However, the population was limited to patients with hyperglycemia and lower SOFA scores; importantly, all blood glucose values from admission to discharge were collected and utilized, which might compromise the feasibility of possible risk stratification in the future.
In the present study, 24-hVBGCV was calculated during the first 24 h after ICU admission, it may provide an earlier prediction of mortality. In the regression model, we adjusted for a series of covariates that may influence mortality; in addition, use of insulin was adjusted into the regression model to eliminate the influence of glucose level. Furthermore, considering the relationship between hyperglycemia and mortality12, we conducted a sensitivity analysis to explore whether such a relationship exists in patients with or without diabetes. Surprisingly, compared with the lowest 24-hVBGCV tertile, the highest tertile was associated with ICU mortality and in-hospital mortality in non-diabetic patients after adjustment for all the covariates. Our results are consistent with previously published findings using mean absolute glucose change per hour or SD in critically ill patients13,14. Therefore, our findings showed that 24-hVBGCV might serve as an independent risk factor of mortality in patients with acute respiratory failure.
Previous studies have demonstrated that high GV leads to greater oxidative stress and endothelial dysfunction than dose sustained hyperglycemia15,16,17. In vitro, Quagliaro et al.15found that exposure of endothelial cells to intermittent high glucose stimulated reactive oxygen species overproduction, leading to accelerated cellular apoptosis. Studies in both patients with diabetes and healthy subjects observed that oscillating glucose produced further significant increases in endothelial dysfunction and oxidative stress compared with sustained high glucose16,17. For non-diabetic patients, acute stress response and inflammatory response were the main causes of increased glucose14. In addition, El-Osta et al.18found that even short-term hyperglycemic spikes could have long-lasting effects on vascular cells. A meta-analysis including at least 12 independent cohorts was shown the relation of glucose variability to ICU mortality in non-diabetic patients with stress hyperglycemia19. Diabetic patients may develop a relative tolerance to the cardiovascular effects associated with moderate degrees of hyperglycemia14. Moreover, hyperglycemia itself is an independent risk factor for death; thus, death caused by diabetes and its complications might conceal the effect of blood glucose fluctuation on mortality12. Therefore, it was reasonable that we found a significant association between GV and mortality in the non-diabetic group rather than in the diabetic group.
This study has the following strengths. First, a large cohort of patients were enrolled from various units (medical and coronary care ICUs), reflecting a real-world situation. Second, this was a homogeneous group of critically ill patients with acute respiratory failure, excluding patients with the extra fluctuations in blood glucose caused by surgical procedures. In addition, the 24-hVBGCV was adopted to avoid the calculation error caused by the difference in blood glucose monitoring frequencies in the treatment process of patients due to diabetes. However, our study also has some limitations. Because of the retrospective design of the study, potential bias (i.e., Berkson’s bias) may exist. Moreover, our study investigated the association between 24-hVBGCV and mortality in patients with acute respiratory failure, rather than causality. Therefore, well-designed prospective studies are needed for future investigation.
Methods
Study design
This is a retrospective cohort study using patients’ data from the MIMIC-II database. It was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center (Boston, MA, USA) and the Massachusetts Institute of Technology (MIT; Cambridge, MA). The patients’ consent was waived because of the retrospective design of the study.
More than 30,000 patients in the MIMIC-II database were enrolled from the intensive care unit (ICU) at Beth Israel Deaconess Medical Center from 2001 to 2008. The database included demographic characteristics, physiological data, treatments, laboratory and radiological data, medical history, and survival outcomes20. All data used for this study were de-identified and available upon request. All authors had completed the Collaborative Institutional Training Initiative course at the University of Miami and received permission to access the MIMIC database.
The following measures were extracted for each patient: age at admission, sex, ethnicity, the first 24-h Sequential Organ Failure Assessment (SOFA) score after admission to the ICU, use of insulin, clinical status (obesity, diabetes, chronic pancreatitis, heart failure, renal failure, and infection), survival outcome, and records of IV glucose monitoring during the first 24 h of ICU stay. The extraction of data was performed by SAS version 9.4 (SAS Institute, Cary, NC, USA).
Participants
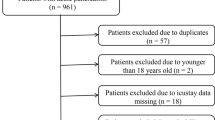
All patients (≥ 15 years old) in the database diagnosed with acute respiratory failure coded with International Classification of Diseases, Ninth Revision (ICD-9) were selected for the analysis. Individuals were excluded if (1) their number of 24-h blood glucose measurements was < 2, (2) they had multiple admissions to the hospital or ICU, (3) they stayed in the ICU for less than 24 h, or (4) they had missing covariates.
The data of 3512 patients with acute respiratory failure were extracted from the MIMIC-II database. The data of 547 (number of 24-h blood glucose measurements < 2), 1,308 (multiple hospital or ICU admissions and/or length of ICU stay < 24 h), and 32 (missing covariates) patients were excluded. Finally, 1625 patients were included in this study (Fig. 1).
Evaluation of glycemic variability
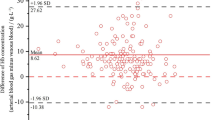
We extracted the glucose levels in venous blood samples during the first 24 h of ICU stay. We assessed variation in venous blood glucose using the CV, calculated as the ratio of the SD to the mean venous blood glucose levels, and expressed as a percentage (CV = SD/mean venous blood glucose level × 100%). Patients were divided into three groups according to the tertiles of 24-hVBGCV.
Outcomes
The outcomes were ICU mortality and in-hospital mortality.
Statistical analysis
Continuous variables are presented as mean ± SD and compared using analysis of variance (ANOVA). Categorical variables are presented as percentages and compared using a chi-squared test. Logistic regression models were used to assess the impact of 24-hVBGCV on ICU and hospital mortality. In multivariate regression analyses, the adjusted covariates included age, sex, ethnicity, SOFA score, obesity, use of insulin, and related comorbidities that could influence mortality or glucose (heart failure, diabetes mellitus, renal failure, chronic pancreatitis, and infection). Interaction analyses were performed between 24-hVBGCV and diabetes. Subgroup analyses were performed between subjects with and without diabetes. The odds ratios (OR) and their 95% confidence intervals (CI) were generated for logistic regression. All data were analyzed using SPSS version 18.0 (SPSS, Chicago, IL). P values less than 0.05 indicated statistical significance.
References
Siegelaar, S. E., Holleman, F., Hoekstra, J. B. & DeVries, J. H. Glucose variability; Does it matter?. Endocr. Rev. 31(2), 171–182 (2010).
Mendez, C. E. et al. Increased glycemic variability is independently associated with length of stay and mortality in noncritically ill hospitalized patients. Diabetes Care 36(12), 4091–4097 (2013).
Hermanides, J. et al. Glucose variability is associated with intensive care unit mortality. Crit. Care Med. 38(3), 838–842 (2010).
Bagshaw, S. M. et al. The impact of early hypoglycemia and blood glucose variability on outcome in critical illness. Crit. Care. 13(3), R91 (2009).
Krinsley, J. S. Glycemic variability: A strong independent predictor of mortality in critically ill patients. Crit. Care Med. 36(11), 3008–3013 (2008).
Ali, N. A. et al. Glucose variability and mortality in patients with sepsis. Crit. Care Med. 36(8), 2316–2321 (2008).
Atamna, A. et al. High blood glucose variability is associated with bacteremia and mortality in patients hospitalized with acute infection. QJM 112(2), 101–106 (2019).
Todi, S. & Bhattacharya, M. Glycemic variability and outcome in critically ill. Indian J. Crit. Care Med. 18(5), 285–290 (2014).
Meyfroidt, G. et al. Dynamic characteristics of blood glucose time series during the course of critical illness: effects of intensive insulin therapy and relative association with mortality. Crit. Care Med. 38(4), 1021–1029 (2010).
Egi, M., Bellomo, R., Stachowski, E., French, C. J. & Hart, G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology 105(2), 244–252 (2006).
Singh, M. et al. Effect of glycemic variability on mortality in ICU settings: A prospective observational study. Indian J. Endocrinol. Metab. 22(5), 632–635 (2018).
Martin, W.G.; Galligan, J.; Simpson, S., Jr., Greenaway, T., Burgess, J. Admission blood glucose predicts mortality and length of stay in patients admitted through the emergency department. Intern. Med. J. 45 (9), 916–924 (2015).
Akirov, A., Diker-Cohen, T., Masri-Iraqi, H. & Shimon, I. High glucose variability increases mortality risk in hospitalized patients. J. Clin. Endocrinol. Metab. 102(7), 2230–2241 (2017).
Krinsley, J. S. Glycemic variability and mortality in critically ill patients: The impact of diabetes. J. Diabetes Sci. Technol. 3(6), 1292–1301 (2009).
Quagliaro, L. et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: The role of protein kinase C and NAD (P)H-oxidase activation. Diabetes 52(11), 2795–2804 (2003).
Ceriello, A. et al. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes 57(5), 1349–1354 (2008).
Monnier, L. et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295(14), 1681–1687 (2006).
El-Osta, A. et al. Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J. Exp. Med. 205(10), 2409–2417 (2008).
Eslami, S., Taherzadeh, Z., Schultz, M. J. & Abu-Hanna, A. Glucose variability measures and their effect on mortality: A systematic review. Intensive Care Med. 37(4), 583–593 (2011).
Saeed, M. et al. Multiparameter intelligent monitoring in intensive care II: A public-access intensive care unit database. Crit. Care Med. 39(5), 952–960 (2011).
Acknowledgements
The MIMIC-II database was supported by the National Institute of Biomedical Imaging and Bioengineering (NIBIB) of the National Institutes of Health (NIH) (grant number R01 EB001659).
Author information
Authors and Affiliations
Contributions
Conceptualization, X.Z., Y.H and G.W; Data curation, J.Z. and G.W; Formal analysis, X.Z., J.Z., Y.H and G.W; Funding acquisition, G.W; Investigation, G.W; Methodology, X.Z, J.Z. and J.L.; Project administration, G.W; Supervision, Y.H and G.W; Validation, X.Z, J. Z, J.L. and G.W; Writing—original draft, X.Z.; Writing—review & editing, X.Z., J.Z., X.J., R. L., Y.G., J.L., X.W, Y.H. and G. W.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Zhang, J., Li, J. et al. Relationship between 24-h venous blood glucose variation and mortality among patients with acute respiratory failure. Sci Rep 11, 7747 (2021). https://doi.org/10.1038/s41598-021-87409-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87409-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.