Abstract
This study aimed to investigate changes in Schlemm’s canal, intraocular pressure and ocular blood circulation following the activation of the sympathetic nervous system. Twenty healthy volunteers were enrolled in this study. The cold pressor test (CPT) was adopted. Cross-sectional area of Schlemm’s canal (SCAR), superficial and deep retinal vessel densities (s-RVD;d-RVD), pupil diameter (PD), intraocular pressure (IOP), mean ocular perfusion pressure (MOPP) and heart rate variability (HRV) were measured at three time-points: baseline (T0) and 5 min (T1) and 10 min (T2) after the CPT. After cold stimulation, LF/HF index (the ratio of low frenquency and high frenquency) increased significantly. IOP decreased from 16.9 ± 1.9 mmHg at baseline to 16.4 ± 2.7 mmHg at T1 and to 15.2 ± 2.7 mmHg at T2. The nasal cross-sectional area of SCAR (SCAR-n) increased from 6283.9 ± 2696.2 µm2 at baseline to 8392.9 ± 3258.7 µm2 at T1 and to 10422.0 ± 3643.8 µm2 at T2. The temporal cross-sectional area of SCAR (SCAR-t) increased from 6414.5 ± 2218.7 µm2 at baseline to 8610.8 ± 2317.1 µm2 at T1 and to 11544.0 ± 4129.2 µm2 at T2. The expansion of Schlemm’s canal was observed after the CPT might be caused by sympathetic nerve stimulation, subsequently leading to decreased IOP.
Similar content being viewed by others
Introduction
The sympathetic nervous system (SNS) is a component of the peripheral nervous system that regulates many human physiological variables including heart rate, blood pressure, respiration, digestion, and sexual arousal1. In the eye, the intraocular pressure and ocular blood circulation were also mainly controlled by the sympathetic nervous system2,3. The influence of circadian rhythm in the SNS upon intraocular pressure has been a subject of interest. It was found that excision of the superior cervical sympathetic ganglion lowered, and electrical stimulation of the sympathetic nerve trunk elevated IOP4. In 1898, cervical sympathectomy became a popular operation, with most glaucoma surgeons fascinated about its results5. However, the effect on IOP was transient after interfering with the autonomic nervous system (ANS) and the mechanism by which the SNS influences IOP remains controversial.
In general, the branches of the central retinal artery are not innervated by adrenergic fibres and the systemic control of the autonomic nervous system has a minor influence, however, there are some conflicting opinions regarding the absence of the influence of sympathetic innervation on the retina6. Lanigan et al. reported a significant association between retinal vessel calibre and sympathetic nervous stimulation2. After sympathetic blockage (stellate ganglion blockage, SGB), the blood flow of the optic nerve head (ONH) and the ipsilateral retina significantly increased7; In addition, there was a report that SGB increased the retinal circulation in patients with Bell’s palsy8. However, no study evaluating the effects of SNS on the ONH and the retinal vessel density has been conducted.
The increased intraocular pressure is the major risk factor of glaucoma, which is a leading cause of irreversible blindness in the world9,10. The insufficient retinal blood supply was also found that has a role in the development of glaucoma in recent years11. So, it is necessary to evaluate the effect of the autonomic nervous system upon the IOP and ocular blood supply.
Several autonomic nervous function tests are available to aid clinicians, including the hand-grip exercise, head tilt test, the cold pressor test (CPT) and the water drinking test12,13. The CPT remains the most well-known test for the determination of ANS integrity14. Numerous studies have found that the CPT induces reproducible, sympathetic nervous system (SNS) activation in normal subjects15,16,17. This study aimed to examine the variations in retinal and ONH vessel density and possible mechanisms underlying IOP changes following the activation of the SNS after the CPT.
Results
Twenty-four participants (24 eyes) were enrolled in this study. Four participants were excluded due to unsatisfactory image quality. Finally, 20 participants (20 eyes; 11 males; 9 females) were included. Participants’ mean age was 26.75 ± 3.3 years (range 22–36, years), mean best corrected visual acuity (BCVA) was 0.98 ± 0.06 (range 0.8–1.0) and mean RE was −2.14 ± 2.01 diopter (range −5.50–0.80, diopter).
SCAR-n, SCAR-t increased after cold stimulation (Fig. 1). SCAR-n increased from 6283.9 ± 2696.2 µm2 at T0 to 8392.9 ± 3258.7 µm2 post-CPT at T1 and increased to 10422.0 ± 3643.8 µm2 at 10 min post-CPT. SCAR-t increased from 6414.5 ± 2218.7 µm2 at T0 to 8610.8 ± 2317.1 µm2 post-CPT at T1 and increased to 11544.0 ± 4129.2 µm2 at T2. IOP changed from 16.9 ± 1.9 mmHg at T0 to 16.4 ± 2.7 mmHg at T1 and then further decreased to 15.2 ± 2.7 mmHg at T2, post-CPT. Pupil diameter increased from 5.22 ± 0.9 mm at T0 to 5.50 ± 0.9 mm at T1 and returned to 5.11 ± 0.8 mm at T2 (Fig. 2). MAP (Mean arterial pressure) increased from 91.4 ± 2.1 mmHg (T0) to 100.9 ± 2.8 mmHg (T1) and returned to 88.9 ± 2.3 mmHg (T2). MOPP (Mean ocular perfusion pressure) increased from 74.0 ± 8.4 mmHg at T0 to 84.6 ± 11.8 mmHg at T1 and then decreased to 73.3 ± 9.7 mmHg at T2, post-WDT. (Table 1). In the control group, no significant change in these parameters were found (Table 2).
Morphology of Schlemm’s canal (yellow arrow). Before (left, T0) and after (right, T2) the cold pressor test. The SCAR increased after the CPT. SC: Schlemm’s canal; AC: anterior chamber. SCAR: Cross-sectional area of Schlemm’s canal; CPT: Cold pressor test. T0: recordings at baseline after 5 min rest; T2: recordings (6–10 min) after 1 min cold stimulation.
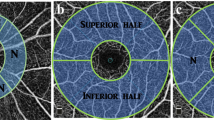
After cold stimulation, LF/HF increased from 0.53 ± 0.24 at T0 to 0.82 ± 0.25 and decreased to 0.59 ± 0.24 (Fig. 3). Superficial retinal and deep vessel densities across four quadrants (inferior, superior, nasal, and temporal) decreased at T1 after CPT and then returned to baseline at T2 (Fig. 4A,B).
The HRV results obtained from a 3-leads ECG recording. The frequency domains are generated using Fourier transform from the recorded R–R intervals. Upper: The R–R interval curve from the 1-minute recording. Below: The frequency domain result during the CPT (T0 and T1). VLF: 0–0.04 Hz, LF: 0.04–0.15 Hz, HF:0.15–0.4 Hz. HRV: Heart rate variability; ECG: Electrocardiograph.
(A,B) The retinal vessel density decreased significantly at T1 after cold stimulation. A1: the diagram of OCTA in superficial retinal layer; A2: the diagram of superficial retinal vessel density at T0; A3: the diagram of superficial retinal vessel density at T1 after CPT; B1: the diagram of OCTA in deep retinal layer; B2: the diagram of deep retinal vessel density at T0; B3: the diagram of deep retinal vessel density at T1. CPT: Cold pressor test. OCTA: Optic Coherence Tomography Angiography.
The significant differences were revealed by the one-way repeated measures ANOVA test. The SCAR (nasal and temporal) significantly increased from T0 to T2; MAP and MOPP significantly increased from T0 to T1 and returned to baseline at T2. The IOP significantly decreased from T0 to T2; the LF/HF significantly increased from T0 to T1 and returned to baseline at T2. The pupil diameter significantly increased in T1 and returned to baseline in T2. Both of s-RVD and d-RVD significantly decreased at T1 and returned to baseline in T2. (Fig. 5A–D). There were no significant differences in TM-thickness and ODVD (optic disc vessel density) at any timepoints.
(A–D) One-way repeated measures ANOVA of SCAR-n, SCAR-t, IOP, MOPP, PD, s-RVD and d-RVD at three time-points (T0, T1, T2) during cold stimulation. The asterisk indicates statistically significant differences (P < 0.05). ANOVA: Analysis of Variance; SCAR-n: the nasal cross-sectional area of Schlemm’s canal; SCAR-t the temporal cross-sectional area of Schlemm’s canal; IOP: intraocular pressure; MOPP: mean ocular perfusion pressure; PD: pupil diameter; s-RVD: the superficial retinal network; d-RVD: the retinal deep capillary network.
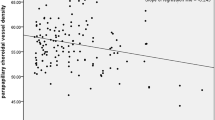
A significant correlation was found between ΔSCAR-m (The variation of mean value of SCAR in nasal and temporal from T0 to T2) and ΔIOP (The variation of IOP from T0 to T2; R2 = 0.3106, P = 0.011), and also found between ΔSCAR-m and ΔLF/HF (The variation of LF/HF from T0 to T2; R2 = 0.202, P = 0.04), but not in ΔSCAR-m and ΔPupil diameter (The variation of LF/HF from T0 to T2; R2 = 0.013, P = 0.63, Fig. 6A–C).
(A–C) The linear regression analyses of ΔSCAR-m, ΔIOP, ΔPD and ΔLF/HF. There is significant correlation of ΔSCAR-m and ΔIOP, ΔSCAR and ΔLF/HF, but not in ΔSCAR and ΔPD. ΔSCAR-m: The variation of mean value of SCAR in nasal and temporal from T0 to T2; ΔIOP: the variation of IOP from T0 to T2. ΔPD: the variation of pupil diameter from T0 to T2; ΔLF/HF: the variation of LF/HF from T0 to T2.
Discussion
The cold pressor test was first described by Hines and Brown in 1932, which was designed to measure the reaction of the blood vessels to a standard stimulus18. Increased BP reaction to CPT has been associated with a higher risk of hypertension19. Fremann et al. found that the response will promote an increase of 15–20 mmHg and 10–15 mmHg in systolic and diastolic blood pressure, respectively15. In our study, MAP and MOPP were also found to increase obviously during the CPT. The release of norepinephrine and epinephrine, the activation of β-adrenergic receptors and α2-adrenergic activity were validated after the cold stimulation. The activation of the peripheral sympathetic nervous system during the CPT is considered as the major mechanisms mediating the vasoconstrictive response20,21.
Heart rate variability (HRV) is the physiological variation between the R-R beat, which could provide real-time information of the peripheral autonomic nervous system non-invasively. HRV was used in our study to evaluate the SNS activity during the CPT. The frequency domains of HRV were acquired by the Fourier transform and divided into three parts: very-low-frequency (VLF, 0–0.04 Hz), low-frequency (LF, 0.04–0.15 Hz), and High Frequency (HF, 0.15–0.4 Hz). The LF/HF was thought to represent the balance of activity of the sympathetic and parasympathetic nervous system, especially the activity of SNS22. In our study, after the CPT, the significantly increased LF/HF was found, which indicated that the sympathetic nervous system was activated during the CPT.
The autonomic nervous system maintains the physiological functions of numerous body organs, such as the heart, lungs and gastrointestinal tract23. The ocular response for the ANS mainly included the variation of pupil size, intraocular pressure and ocular blood flow. Pupillary size might be influenced by many factors, such as illumination intensity, wakefulness, emotional state etc., but mainly reflected the balance between the tonus of sympathetic (pupil dilatation) and parasympathetic (pupil constriction) nervous system. In our study, pupil diameter was found significantly dilated after cold stimulation, which means that the balance disorders of peripheral ANS occurred. IOP was found to obviously decreased during the cold pressor. The balance of aqueous humor production and outflow determines IOP. Previous studies discussed that parasympathetic and sympathetic innervation involved influenced both aqueous humor production and outflow. But the precise underlying mechanism of any observed changes in IOP is still unclear24.
Schlemm’s canal is a vessel that collects aqueous humor and passes it into the bloodstream, thus serving a critical role in the maintenance of stable intraocular pressure (IOP), which is essential for maintaining the eye’s physiological functions25. By using a morphometric analysis system, Allingham RR et al. found that reduction in SC dimensions in POAG eyes may account for approximately half of the decrease in outflow facility26. The SC has attracted considerable interest in recent years27. In this study, SCAR was found expanded and was correlated with the activation of SNS (LF/HF index). In our previous work, SNS was stimulated by the aerobic exercise, consequently causing the expansion of the SC lumen and IOP reductions28. Histological studies have been revealed that β2-adrenergic receptors expressed in the SC. Specifically, Zhou et al. also found that endothelial SC cells softened to isoproterenol via its action on β2 adrenergic receptors29,30. Collectively, these findings indicated that the SNS is involved in SC regulation. Significant increases in SCAR following cold stimulation in the present study could be explained by the activation of the SNS.
Mathematical modeling revealed that the dilation of the SC increases its outflow facility and leads to subsequent IOP reductions31. An in vitro study found that increased IOP was often accompanied by occlusions to the SC lumen32. Increasing the length of the SC also improves its outflow, as observed after treatment with SC scaffolds32,33. By means of SC-relevant anti-glaucoma surgery, such as canaloplasty, viscocanalostomy, and SC scaffolding, significant decreases in IOP can be achieved34. Above all, there’s the close relationship of Schlemm’s canal with the maintenance of stable IOP. In the present study, IOP was found to significantly decrease. And the variation of SCAR and IOP correlated significantly in the post-CPT period. Thus, the IOP trough following CPT might arise from the expansion of SC lumen.
There is a significantly decreased vessel density of retinal tissue after cold stimulation. In 1973, the efficient auto regulation of retinal blood flow was first proposed by Alm and Bill. Any elevation in retinal perfusion pressure is compensated by vasoconstriction in the retinal vasculature to maintain the stability of the retinal blood flow and vice versa35. Nagaoka T also found that the constriction of the retinal arterioles plays an important role in the maintenance of retinal blood flow in response to an acute increase in systemic BP using a laser Doppler velocimetry system36. The acute increase in MOPP may explain the decreased superficial and deep retinal vessel density in our study.
However, in our observation, there is no significant change in vessel density of optic disc after the activation of SNS. According to Takayama J, the velocity of ONH does not differ significantly between eyes with and without sympathetic nerve amputation; suggesting that the sympathetic system has no effect on ONH circulation37. The result is the same as what we found. Many studies have found that the trabecular sheets mechanically distend into the SC when an IOP of 30–50 mmHg is achieved, reducing the SC lumen38. However, in this study, we found no significant change in TMTH (trabecular meshwork thickness) following cold stimulation. Thus, the IOP decrease in this study is likely not due to variations of the TM.
While it offers some interesting insights into ocular physiology, the present study also has some limitations that warrant discussion. First, the results might be compared to those in abnormal, aged glaucoma populations or developmental glaucoma populations in future studies. Second, animal models might allow for more precise testing of mechanism and third, using the CPT with different models of ocular degeneration might allow further elucidation of ocular physiology.
Patients and Methods
Participants
A total of 24 healthy volunteers from Tongji Hospital in Wuhan (Hubei province, China) were recruited between May 2018 and August 2018. All participants underwent an ophthalmic examination. The eye ipsilateral to the dominant hand was used for all studies.
Inclusion criteria were as follows: 1) IOP < 21 mmHg and normal ophthalmoscopic appearance of the optic nerve (cup-to-disc ratio < 0.5 in both eyes, cup-to-disc ratio asymmetry <0.2, absence of hemorrhage, and localized or diffuse rim thinning); 2) greater than 18 years of age; 3) no history of use of medications that affect the circulatory system within the month prior to their enrolment; 4) no caffeine consumption for at least 24 hr prior to their participation.
Exclusion criteria were as follows: 1) Best-corrected visual acuity (BCVA) < 0.5 (to ensure that the subjects had good central fixation); 2) Refractive error (RE) ≤ −6.0 D and RE ≥ + 3.0 D; 3) serious cataracts or other ocular diseases that hamper optical coherence tomography (OCT) imaging; 4) presence of other eye diseases such as age-related macular degeneration, retinal detachment, or a history of previous eye operations; 5) history or current hypertension or diabetes, or a family history of these conditions.
The study protocols were approved by the ethics committee of Tongji Hospital. Written informed consent was obtained prior to enrollment from all the participants in accordance with the tenets set forth in the Declaration of Helsinki.
Experimental procedure
The experimental group
The experimental recordings were initiated after a 5-min rest period. A baseline recording was obtained (T0, 5 min); followed by a 1-min CPT and 10 min final recovery period (T1: 0–5 min; T2: 6–10 min). For the CPT, the dominant eye and hand were included in this study. Participants were instructed to immerse their hand into an ice water bath (0°C).
The control group
The same procedure was repeated on another day. The same subjects were instructed to place their hand into an empty container for 1 min.
Their IOP, BP, HR, PD, ECG recording, the profile images of Schlemm’s canal and trabecular meshwork, the retinal and optic disc angiography images on the same side were acquired successively at T0, T1, and T2.
Measurement of intraocular pressure (IOP), systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR)
Patients fasted for at least 4 hr, after which 3 assessments were conducted. The IOP was measured using an I-care rebound tonometer (I-Care Finland Oy, Vantaa, Finland). All IOP measurements were taken by the same experienced examiner (CW). A different observer (CZQ) read and recorded the IOP readings blinded to minimize any bias.
SBP, DBP, and HR were recorded using an automatic sphygmomanometer (OmronHEM-7201; Omron, Dalian, Liaoning, China). The mean arterial pressure (MAP) and mean ocular perfusion pressure (MOPP) were calculated using the following equation: MAP = [(2 × DBP) + SBP]/3; MMOP = 2/3 (MAP− IOP).
Measurement of ocular variables
Swept-source optic coherence tomography (ss-OCT)
Assessments described in the procedure above were obtained via swept-source optic coherence tomography (OCT) using a 1310-nm wavelength and a scan speed of 30,000 A-scans per sec and an axial resolution of less than 10 μm. 3D-angle high-definition images were obtained using volumetric scans (dimension, a raster of 64 B scans each with 512 A-scans over 8 mm). Nasal and temporal quadrant scans were performed independently, and subjects were instructed to stare at one of two peripheral fixation lights. Conjunctival vessels were used as landmarks to scan the same limbal area before and after cold pressor stimulation. Scans of each site were obtained at three time points (T0, T1, T2) and with the best quality at each position (temporal area and nasal area) was chosen. All OCT tests were performed under standardized darkroom photopic conditions (ca. 3.5 lux).
The Angio-Vue optic coherence tomography angiography (Angio-Vue OCTA)
The Angio-Vue optic coherence tomography angiography (OCTA; Optovue Inc, Fremont, CA) system uses a split-spectrum amplitude-decorrelation angiography software algorithm and acquires 70,000 A-scans per sec to create OCTA volumes consisting of 304 × 304 A-scans. A central 6 mm × 6 mm region of the macula and 4.5 × 4.5 mm region of the optic disc were captured. All OCT tests were performed under standardized darkroom photopic conditions (ca. 3.5 lux).
Schlemm’s canal cross-sectional area (SCAR) and trabecular meshwork thickness (TMTH)
Schlemm’s canal and trabecular meshwork were imaged during three time-periods (T0, T1, T2) using swept-source OCT (CASIA SS-1000, www.tomey.com) following a 5-min rest period.
The area of the nasal SC (SCAR-n; µm2) and temporal SC (SCAR-t; µm2) viewed at one region and the trabecular meshwork thickness (TMTH) of two regions (nasal and temporal) at three different time-points were measured using Image J software (version 1.45 S, National Institutes of Health, Bethesda, MD, USA). SC was defined as being observable when a black, lucent space was found (Fig. 7). The thickness of the TM was calculated as the average of measurements acquired at the anterior endpoint and the middle portion of SC, as reported previously28.
Measurement of retinal vessel density (RVD) and the optic disc vessel density (ODVD)
The retinal and optic disc vessel density was defined as the proportion of vessel area with blood flow over the total area measured, respectively. The superficial retinal network (s-RVD) included vessels from 3 mm below the internal limiting membrane to 15 mm below the inner plexiform layer; the retinal deep capillary network (d-RVD) included vessels between 15 mm and 70 mm below the inner plexiform layer. Indicators of retinal and optic disc RVD were measured at three time-points around CPT acquisition. (Fig. 8A–C).
(A–C) The OCTA images of the macular (6 × 6 mm) and optic disc (4.5 × 4.5 mm) vascular networks. (A) The retinal superficial network labeled from 3 mm below the internal limiting membrane to 15 mm below the inner plexiform layer (from red line to green line); (B) The retinal deep capillary network marked from 15 mm to 70 mm below the inner plexiform layer. (from green line to red line); (C) The Angio disc angiography was performed to generate images (4.5 mm × 4.5 mm) with the optic disc at the center. Optic disc vessel density within the RNFL was measured from internal limiting membrane (ILM) to RNFL posterior boundary (from red line to green line). OCTA: Optic Coherence Tomography Angiography; RNFL: Retinal nerve fiber layer.
Measurement of heart rate variability (HRV)
After a 5-min resting period, subjects received the 3-leads ECG recording in the sitting position for 1 min. After the 1 min cold stimulation, the same ECG process was repeated. The R-R peak was extracted and analyzed by the Kubios HRV Premium software (version 2.2; University of Eastern Finland). The index of Low frequency divides high frequency (LF/HF index) was calculated.
All measurements were taken by two observers blinded. Cases of a discrepancy of >15% were resolved by consulting the senior-most author. All data were recorded and stored for later statistical analyses.
Statistical analyses
All statistical analyses were performed using SPSS software (Version 16.0, SPSS Inc., Chicago, IL, USA). The data are presented as mean values (Means ± SDs). One-way repeated-measures ANOVA was used to compare differences in nasal and temporal SCAR (SCAR-n; SCAR-t), as well as IOP, TMTH, LF/HF, pupil diameter (PD), MOPP, HR, RVD and ODVD at three different time-periods. The paired-sample T test was used to compare the parameters at two different time points in the control group. The linear regression analyses were adopted to examine the relationship between the variations of SCAR-m (the mean value of SCAR-n and SCAR-t) and the change of IOP, the change of PD and the change of LF/HF from T0 to T2 (ΔSCAR-m, ΔIOP, ΔPD and ΔLF/HF). All tests were two-tailed. Statistical significance was defined as a P-value < 0.05.
References
Park, H. L., Jung, S. H., Park, S. H. & Park, C. K. Detecting autonomic dysfunction in patients with glaucoma using dynamic pupillometry. Medicine. 98, 11 (e14658) (2019).
Lanigan, L. P., Clark, C. & Hill, D. W. Retinal Circulation Responses to Systemic Autonomic Nerve Stimulation. Eye. 2, 412–417 (1988).
Acott, T. S., Kelley, M. J. & Keller, K. E. Intraocular Pressure Homeostasis: Maintaining Balance in a High-Pressure Environment. Journal of Ocular pharmacology and therapeutics. 24, 94–101 (2014).
Abadie, C. Nature et traitement du glaucome. Arch d’Ophthalmologie. 19, 94e (1899).
Feibel, R. M. Sympathectomy for glaucoma: Its rise and fall (1898–1910). Survey of ophthalmology. 60, 500–507 (2015).
Forster, B. A., Ferrari-Dileo, G. & Anderson, D. R. Adrenergic alpha 1 and alpha 2 binding sites are present in bovine retinal blood vessels. Invest Ophthalmol Vis. Sci. 28, 1741–1746 (2015).
Yua, H. G., Chunga, H., Yoonb, T. G., Yum, K. W. & Kim, H. J. Stellate ganglion block increases blood flow into the optic nerve head and the peripapillary retina in human. Autonomic Neuroscience: Basic and Clinical. 109, 53–57 (2003).
Nagahara, M., Tamaki, Y., Araie, M. & Umeyama, T. The acute effects of stellate ganglion block on circulation in human ocular fundus. Acta. Ophthalmol Scand. 79, 45–48 (2001).
Clark, C. V. & Mapstone, R. Systemic autonomic neuropathy in open-angle glaucoma. Doc Ophthalmol 64, 179–85 (1986).
Boland, M. V. et al. Comparative Effectiveness of Treatments for Open-Angle Glaucoma: A Systematic Review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 158, 271–279 (2013).
Chan, K. K. W., Tang, F. Y., Tham, C. C. Y., Young, A. L. & Cheung, C. Y. Retinal vasculature in glaucoma: a review. BMJ Open Ophthalmol. 11, 1–14 (2017).
Fu, Q. et al. Cardiovascular and sympathetic neural responses to handgrip and cold pressor stimuli in humans before, during and after spaceflight. Journal of Physiolog. 544, 653–664 (2002).
Jordan, J. et al. The Pressor Response to Water Drinking in Humans: A Sympathetic Reflex? Circulation. 101, 504–509 (2000).
Scharf, M & Korczyn, A. D. Cold pressor test. In: Korczyn, A. D., editor. Handbook of Autonomic Nervous System Dysfunction. New York: Marcel Decker. P, 557–562 (1995).
Freeman, R. Assessment of cardiovascular autonomic function. Clin Neurophysiol. 117, 716–730 (2002).
Kashima, H., Hayashi, N. & Ikemura, T. Regional differences in facial skin blood flow responses to the cold pressor and static handgrip tests. Eur. J. Appl. Physiol. 113, 1035–1041 (2013).
Velasco, M., Gomez, J., Blanco, M. & Rodrjguez, I. The cold pressor test: Pharmacological and therapeutic aspect. American journal of therapeutics. 4, 34–38 (1994).
Wolff, H. H. The mechanism and significance of the cold pressor response. Quarterly Journal of Medicine. 79, 261–273 (1951).
Zhang, M. Z. et al. Factors Associated with Blood Pressure Response to the Cold Pressor Test: The GenSalt Study. American Journal of Hypertension. 26, 1132–1139 (2013).
Mudge, G. H., Grossman, W., Mills, R. M., Lesch, M. & Braunwald, E. Reflex increase in coronary vascular resistance in patients with ischemic heart disease. The New England journal of medicine. 295, 1333–1337 (1976).
Nabel, E. G., Ganz, P., Gordon, J. B., Alexander, R. W. & Selwyn, A. P. Dilation of normal and constriction of atherosclerotic coronary arteries caused by the cold pressor test. Circulation. 77, 43–52 (1988).
Henry, B. L., Minassian, A., Paulus, M. P., Geyer, M. A. & Perry, W. Heart rate variability in bipolar mania and schizophrenia. J. Psychiatr. Res. 44, 168–176 (2010).
Gordan, R., Gwathmey, J. K. & Xie, L. H. Autonomic and endocrine control of cardiovascular function. World J. Cardiol. 7, 204–214 (2015).
McDougal, D. H. & Gamlin, P. D. Autonomic Control of the Eye. Compr. Physiol. 5, 439–473 (2015).
Carreon, T., van der Merwe, E., Fellman, R. L., Johnstone, M. & Bhattacharya, S. K. Aqueous outflow– A continuum from trabecular meshwork to episcleral veins. Prog. Retin. Eye Res. 57, 108–133 (2017).
Allingham, R. R., de Kater, A. W. & Ethier, C. R. Schlemm’s canal and primary open angle glaucoma: correlation between Schlemm’s canal dimensions and outflow facility. Exp. Eye Res. 62, 101–109 (1996).
Genaidy, M. M., Zein, H. A. & Eid, A. M. Combined phacocanaloplasty for open-angle glaucoma and cataract: 12 months results. Clinical Ophthalmology. 11, 2169–2176 (2017).
Yan, X. Q. et al. Influence of Exercise on Intraocular Pressure, Schlemm’s Canal, and the Trabecular Meshwork. Investigative Ophthalmology & Visual Science. 57, 4733–4739 (2014).
Alvarado, J. A., Murphy, C. G., Franse-Carman, L., Chen, J. & Underwood, J. L. Effect of b-adrenergic agonists on paracellular width and fluid flow across outflow pathway cells. Invest Ophthalmol Vis. Sci. 39, 1813–1822 (1998).
Zhou, E. H. et al. Mechanical responsiveness of the endothelial cell of Schlemm’s canal: scope, variability and its potential role in controlling aqueous humor outflow. J. R. Soc. Interface. 9, 1144–1155 (2012).
Yuan, F., Schieber, A. T., Camras, L. J., Harasymowycz, P. J. & Allingham, R. R. Mathematical Modeling of Outflow Facility Increase with Trabecular Meshwork Bypass and Schlemm Canal Dilation. J. Glaucoma. 25, 355–364 (2016).
Johntone, M. A. et al. Pressure-dependent changes in structures of the aqueous outflow system of human and monkey eyes. American journal of ophthalmology. 75, 365–383 (1973).
Hann, C. R., Vercnocke, A. J., Bentley, M. D., Jorgensen, S. M. & Fautsch, M. P. Anatomic changes in Schlemm’s canal and collector channels in normal and primary open-angle glaucoma eyes using low and high perfusion pressures. Invest Ophthalmol Vis. Sci. 55, 5834–5841 (2014).
Mansouri, K. & Shaarawy, T. Update on Schlemm’s canal based procedures. Middle East Afr. J. Ophthalmol. 22, 38–44 (2015).
Alm, B. & Bill, A. The effect of stimulation of the cervical sympathetic chain on retinal oxygen tension and on uveal, retinal and cerebral blood flow in cats. Acta. Physiol. Sand. 88, 84–94 (1973).
Nagaoka, T., Mori, F. & Yoshida, A. Retinal Artery Response to Acute Systemic Blood Pressure Increase during Cold Pressor Test in Humans. Invest Ophthalmol Vis. Sci. 43, 1941–1945 (2002).
Takayama, J. et al. Topical phenylephrine decreases blood velocity in the optic nerve head and increases resistive index in the retinal arteries. Eye (Lond). 23, 827–34 (2009).
Griuerson, I. & Lee, W. R. The Fine Structure of the Trabecular Meshwork at Graded Levels of Intraocular Pressure (1) Pressure Effects Within the Near-Physiological Range (8–30 mmHg). Exp. Eye Res. 20, 505–521 (1975).
Acknowledgements
The authors would like to express special thanks to Zhitao Wang and Jian Sun for supporting in this study.
Author information
Authors and Affiliations
Contributions
J.W. carried out study design; H.Z. led field data collection and aided in experimental design; W.C. completed data collection, analyzed data and drafted the manuscript; ZC aided in field data collection and analyzed data; Y.X. and C.D. oversaw data analysis. All authors contributed to manuscript revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, W., Chen, Z., Xiang, Y. et al. Simultaneous influence of sympathetic autonomic stress on Schlemm’s canal, intraocular pressure and ocular circulation. Sci Rep 9, 20060 (2019). https://doi.org/10.1038/s41598-019-56562-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56562-0
This article is cited by
-
Abnormal Systemic and Ocular Responses to the Valsalva Manoeuvre in Primary Open-Angle Glaucoma: A Case for Autonomic Failure?
Current Medical Science (2023)
-
Influence of mental stress on intraocular pressure and visual field testing: is there a white coat syndrome in glaucoma?
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.