Abstract
Microvesicles are small membranous particles generated during cellular activation or stress. The analysis of the content and the surface of microvesicles allow conclusions about the cells they are originating from and the underlying pathology. Therefore, CSF microvesicles have been suggested to be promising targets to monitor the (etio)pathology of neurodegenerative diseases. Microvesicles in the CSF of 15 patients with Alzheimer’s disease and 15 controls were analyzed by flow cytometry regarding the levels of CD3, CD4, CD45, CD64, BACE1, Aβ, APP and tau. The results were replicated in a second cohort comprising 14 patients with Alzheimer’s disease and 9 controls. The levels of tau and APP were reduced in microvesicles of Alzheimer’s disease patients. A significant change was neither observed in the number of microvesicles nor in the expression of the other antigens. Tau and APP in microvesicles separated patients with Alzheimer’s disease from controls with an AUC of 0.84 and 0.89 respectively. We conclude that tau and APP in CSF microvesicles are promising biomarkers which could directly provide information about the Alzheimer pathology on a cellular level.
Similar content being viewed by others
Introduction
Extracellular vesicles are a heterogeneous group of cell derived, membrane coated particles1. While a clear cut definition is hardly possible, extracellular vesicles are divided into exosomes, microvesicles and apoptotic bodies2. With a size between 30–100 nm, exosomes are the smallest particles. They are derived from the endosomal system and are released via fusion of multivesicular bodies with the cell membrane1. Apoptotic bodies form during apoptosis and are above 1000 nm in size. Microvesicles measure between 100–1000 nm and are created during cellular activation or under stress by a regulated external budding of the plasma membrane. During this process, phosphatidylserine is translocated from the inner to the outer leaflet of the lipid bilayer, where it can be detected by Annexin V (AxV). Microvesicles contain proteins and RNA of the cytoplasm and carry membrane antigens of their host cells on their surfaces3.
It was originally assumed, that the main function of microvesicles is the elimination of toxic metabolites from the cell4. Today several other physiologic functions are known, such as communication between cells, transfer of proteins, RNA, and receptors between cells, regulation of synaptic activity as well as immune modulation3,5. Also, cyto-protective properties of microvesicles have been repeatedly shown6,7.
As their generation is associated with cellular activation and stress, microvesicles are considered to be suitable biomarkers for several diseases. Carrying surface receptors and intracellular proteins of their originating cells, microvesicles can be regarded as reporters of the focus and kind of pathology8. While there are a lot of reports on changes in extracellular vesicle composition in stroke, neuroinflammation, epilepsy or brain tumors, little is known about their role in neurodegenerative diseases such as Alzheimer’s disease9,10,11,12. Unfortunately, most studies do not clearly distinguish between exosomes, microvesicles and apoptotic bodies8. In addition, almost nothing is known about extracellular vesicles derived from neurons.
Biomarkers are intended to portray aspects of the pathophysiology of diseases13. While the cause of AD is still under debate, the neuropathology is characterized by the deposition of amyloid-β (Aβ) fibrils and hyperphosphorylated tau, accompanied by neuroinflammation14. Increasing attention is being paid to the role of extracellular vesicles in this process15. It seems that oligomeric tau and Aβ can be transferred between cells via exosomes16,17. This gave rise to the hypothesis that extracellular vesicles may be the carrier of prion-like misfolded proteins spreading the disease18. Contrarily, there are also studies showing a degradation of fibrils in the presence of extracellular vesicles19,20.
Established biomarkers of AD have several shortcomings. Measurement is hard to standardize, they are expensive, require lumbar puncture or are associated with radioactivity21. The development of disease modifying therapies is especially impaired by the lack of biomarkers that indicate the activity of the disease and predict the rate of cognitive decline22. Therefore, the identification of such biomarkers is of special interest23.
This study aims to detect differences in the composition of microvesicles as well as their load with tau and Aβ peptides in the cerebrospinal fluid (CSF) of patients with AD.
Material and Methods
Patients
The study protocol was approved by the ethic committee of the University Hospital Erlangen-Nuremberg (Nr. 3987), carried out according to the ethical guidelines of the Declaration of Helsinki and patients or their legal guardians provided their informed written consent.
Patients included in this study were referred to our memory clinic due to cognitive complaints. They underwent a psychiatric, neurological, medical and routine laboratory examination. Cognitive deficits were evaluated using the CERADplus battery24. An MRI scan was performed to evaluate brain atrophy and rule out vascular disease. The diagnosis of AD was made according to the NINCDS-ADRDA criteria taking into account the Aβ42/Aβ40-ratio, tau and phospho-tau in CSF25,26. The results of the diagnostic CSF biomarkers were interpreted according to the Erlangen Score (ES) algorithm27. Exclusively, either patients with dementia or MCI with high evidence of AD pathophysiological process (Alzheimer’s disease group, Erlangen Score ≥3) or without evidence of AD pathophysiological process (Control, Erlangen Score ≤1) were included in this study. In reference to the criteria suggested by Jack et al., the patients within the AD group are positive for amyloid and tau pathology as well as neurodegeneration (A+/T+/N+) whereas those in the control group are A-/T-/N-28. Patients with intermediate signs of AD pathophysiology were excluded. Samples analyzed within the replication cohort were recruited independently according to the same procedure but one year later than the initial cohort.
Isolation and storage of microvesicles
After the lumbar puncture, CSF was centrifuged (750 g/5 min) within 30 min. The supernatant containing the microvesicles was collected, aliquoted and stored at −80 °C until analysis. For the evaluation of the impact of centrifugation and storage temperature on the microvesicles, these parameters were varied as indicated.
Flow cytometry
The CSF containing the microvesicles was thawed and immediately incubated with human polyvalent immunoglobulin (Beriglobin, CSL Behring, Marburg, Germany) for 25 min at room temperature (RT) to avoid unspecific binding of antibodies. AxV-FITC (Immunotools, Friesoythe, Germany) and FM4-64 (ThermoFischer scientific, Waltham, MA, USA) were used to define the microvesicle population. Anti CD3-FITC (clone: UCHT-1), CD4-FITC (clone: EDU-2), CD45-FITC (clone: MEM-28) (all Immunotools, Friesoythe, Germany), CD64-FITC (clone: 10.1) (BD Pharmingen, Heidelberg, Germany), anti Aβ-AF488 (clone 6E10, BioLegend formerly Covance, San Diego, CA, USA), anti tau-1-FITC (clone PC1C6), anti amyloid precursor protein (APP)-AF488 (clone 22C11) (both Merck-Millipore, Darmstadt, Germany) or polyclonal anti beta site APP cleaving enzyme 1 (BACE-1) FITC (Sino Biological, Beijing, China) were added and incubated at 4 °C for 30 min. As recommended, unlabeled samples served to determine the total number of microparticles and the background fluorescence29. Fluorescent positive events were defined by their differentiation from antigen-negative-events in stained samples30. Antibodies of the respective immunoglobuline isotype served as additional controls. Samples were measured undiluted with a Gallios flow cytometer (Beckman Coulter, Brea, CA, USA). Excitation for fluorescence was at 488 nm and emitted fluorescence was recorded on the FL1 sensor (525/38 nm BP) as the AUC of FL1. Data analysis was performed with Kaluza software version 1.5 (Beckman Coulter, Brea, CA, USA).
Statistical analysis
Statistical analysis was carried out with Prism 6.0 (GraphPad Software Inc., La Jolla, CA, USA). As not all datasets followed a Gaussian distribution, the non-parametric, two-sided Mann Whitney U Test was applicated. In the replication cohort outliers were removed with the ROUT method (Q = 1%). Correlations were calculated with the Spearman-Test. To evaluate the diagnostic accuracy, receiver operating curves (ROC) were used. Results are presented as median with interquartile ranges and were considered to be significant at a p-value < 0.05.
Ethics approval and consent to participate
The study protocol was approved by the ethic committee of the University Hospital Erlangen-Nuremberg (Nr. 3987) and patients or their legal guardians provided their informed written consent.
Results
Study population
Patients were recruited at the memory clinic of the department of psychiatry, University Hospital Erlangen. Only those with a conclusive clinical and biomarker workup were included in the study. 15 patients were included in the AD group. All displayed an amnestic phenotype in the neuropsychological tests, suffered from a continuous cognitive decline and showed no clinical or biomarker signs of other neurodegenerative diseases. Neurochemical dementia diagnostics using the Aβ ratio, tau and p-tau were positive for all three biomarkers in each patient. In respect to disease severity, nine patients were in the stage of mild cognitive impairment, while six fulfilled the clinical criteria of mild dementia. The control group consisted of 15 patients with cognitive complaints due to depression, Parkinson’s Disease, frontotemporal lobe degeneration or vasculopathy. Neurochemical dementia diagnostics were negative for all three biomarkers for each patient (Table 1). Due to the prospective collection of samples, the age of the included patients could not be properly matched, resulting in a significant higher median age in the AD group. One patient in the control group suffered from a cold. Several others had a clinically non-significant elevation of the CRP resulting in an overall increase of CRP in the control group. In the replication cohort, consisting of 14 patients with Alzheimer’s disease (5 with MCI due to AD) and 9 controls, selected in the same way, as the initial cohort, the median age in the AD group was also about ten years higher.
No change in the total number of microvesicles in the CSF of AD patients
In this sample consisting of 15 patients with AD and 15 controls, microvesicles in CSF were quantified by flow cytometry according to the gating strategy displayed in Fig. 1 (Fig. 1). According to forward- and sidescatter characteristics a gate was defined to include events that were clearly distinct from background but had a smaller forwardscatter than 1 µm polystyrene beads. Microvesicle counts were quantified in unstained samples (without the addition of antibodies). The number of microvesicles in CSF did not differ between controls and AD patients (Fig. 2). Also, size and structure of the microvesicles, as determined by forward- and sidescatter characteristics, did not differ between the groups (Fig. 2).
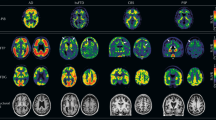
Gating of microvesicles. The respective antibody was added to CSF, incubated and measured directly and undiluted with flow cytometry. Microvesicles were defined by a gate that excluded background and particles with a higher forward scatter than 1 µm beads. The expression of CD3, CD4, CD45, CD64, Aβ, APP, BACE1, and tau was analyzed within the microvesicle gate (MV < 1 µm). Gates defining the respective antigen positive fraction were drawn in respect to an obviously antigen negative fraction within the same measurement.
Number and shape of microvesicles in AD. The number of microvesicles (A), their forward scatter (B), and their side scatter (C) was analyzed within the MV < 1 µm gate as defined in Fig. 1 in unstained samples. No change was observed between patients with Alzheimer’s disease (AD) and patients with cognitive complaints but without AD (CON). (D) Microvesicles in the CSF of 15 AD patients and 15 controls were gated as shown in Fig. 1. The fraction of microvesicles staining positive for the respective antigen is depicted in a tukey-plot. No significant differences were observed between AD patients and controls.
Composition and characterization of CSF microvesicles
Single color staining was performed to measure APP, Aβ, BACE-1, tau, CD3, CD4, CD45, and CD64 to determine the origin of the microvesicles. Within the microvesicle gate defined above, the fraction staining positive for the respective antibody was defined in comparison with a clearly distinguishable unstained population within the same measurement (Fig. 1). For intracellular antigens, the permeability of the microvesicles for the antibodies was confirmed with an α-actin antibody staining. As events within the microvesicle gate were shown to be over 80% FM4-64 and AxV positive, these stainings were not included in each measurement to avoid steric interference and fluorescent quenching (Supplementary Fig. 1).
In the 15 control samples, the most abundant fraction of microvesicles was tau-positive (30.9% [16.8–52.5]) followed by the APP-positive (26.5% [4.3–49.7]), the Aβ-positive (20.1% [6.24–45.0]) and the CD3-positive (18.3 [7.79–45.9]) population (Fig. 2D). No change in the proportion of different microvesicles was observed in AD (Fig. 2D).
For the number of microvesicles, tau, APP, Aβ, CD3, and CD4 the respective inter-and intra-assay coefficients of variation (CV) were calculated by either measuring one sample repeatedly on five consecutive days or within one experiment (Table 2). While the intraassay CV was acceptably low and exceeded 20% only for CD3, the interassay variations were high. Normalization to background did not lead to more homogeneous results. To obtain comparable data, all samples in this study were measured in a single experiment. Inter-aliquot coefficients of variation were calculated by comparing results of five different aliquots measured in one assay. The inter-aliquot CV was highest for Aβ (41.3%) and lowest for CD4 (6.7%). For tau the inter-aliquot CV was 12.0%.
Microvesicles from cerebrospinal fluid of patients with Alzheimer’s disease contain reduced amounts of tau protein
While the number of tau positive microvesicles did not vary between the groups, the mean fluorescent intensity (MFI) of tau-AF488 in tau positive microvesicles was significantly lower in AD patients (Fig. 3). When normalized to unstained microvesicles, or to microvesicles stained with an isotype control, this difference remained significant.
Reduced tau in CSF-derived microvesicles in AD. Microvesicles in the CSF of 15 AD patients and 15 controls were gated as shown in Fig. 1. The mean fluorescence intensities (MFI) for CD3+, CD4+, CD45+, CD64+, Aβ+, APP+, BACE1+, and tau+ microvesicles are shown for AD patients and controls. Differences between the groups were calculated with the non-parametric Mann-Whitney U Test. *p < 0.05.
The MFI of the APP positive microvesicles was lower in AD patients without reaching the level of significance (Fig. 3). As for tau positive microvesicles, no change in the number of APP positive microvesicles was observed. Normalization to the fluorescence intensity of unstained microvesicles or the isotype-control did not lead to different results.
Neither for the MFI of APP positive microvesicles nor for the MFI of tau positive microvesicles correlations with age or the concentrations of Aβ1–40, Aβ1–42 and tau in CSF were found. Also, the MFIs did not correlate with the number of microvesicles. There was no association with the MMSE. However, a highly significant correlation was found between the MFI of tau and APP in the microvesicles of AD patients (r = 0,88; p < 0.0001).
While no statistically significant difference in the number or fraction of Aβ, BACE1, CD3, CD4, CD45, and CD64 positive microvesicles was found, there was a trend towards a lower MFI of CD3 and CD4 in AD (Fig. 3).
Tau in CSF microvesicles as a biomarker for AD
To test whether tau in microvesicles might be a suitable biomarker for AD, receiver operating characteristic (ROC) curves were calculated. Within our sample we found an accuracy of 0.77 (0.76 when normalized on background fluorescence) for the separation of patients with high evidence of AD pathology (n = 15) from those with no biomarker evidence of AD pathology (n = 15) (Fig. 4).
Confirmation of reduced microvesicle tau and APP in a independent replication cohort
The MFI of tau on microvesicles was also reduced in the second, independent replication cohort (Table 3), (Fig. 5A). While there was only a trend for reduced microvesicle-borne APP in the initial cohort, this difference was significant in the replication study (Fig. 5B). As the laser of the flow cytometer had been replaced between the two studies, the measured values are lower in the replication study and can therefore not be combined with the first study. Outliers, identified by the ROUT method, were removed from the analysis. For tau, there were two outliers in the AD group with a measured MFI of 42.4 and 30.6. Also in the measurement of APP there were two outliers in the AD group with MFI values of 146.8 and 33.1. Without the removal of the outliers, the difference between the study groups is still significant for APP (p = 0.028) and is reduced to a trend (p = 0.083) for tau. Again, we found no correlation of microvesicle tau or APP with age, the established CSF biomarkers or with the MMSE.
Replication of reduced tau and APP in CSF-derived microvesicles in AD. Microvesicles in the CSF of 14 AD patients and 9 controls were gated as shown in Fig. 1. The mean fluorescence intensities (MFI) for tau+ (A) and APP+ (B) microvesicles are shown for AD patients and controls. Differences between the groups were calculated with the non-parametric Mann-Whitney U Test. Receiver operating characteristics for both parameters are shown in (C) and (D). **p < 0.01.
A ROC analysis in the second cohort resulted in a AUC of 0.84 (p < 0.01) for tau and 0.89 (p < 0.01) for APP (Fig. 5C,D).
Sampling and storage conditions
Optimized treatment and storage conditions were established prior to this study. Therefore, the total number of FM4-64+/AxV+ microvesicles were assessed by flow cytometry. Storing the uncentrifugated samples at 4 °C or −20 °C increased the number of microvesicles up to threefold. Centrifugation of CSF at 750 g/5 min within 30 min after sampling only marginally reduced the total number of microvesicles. Subsequent storage at RT, 4 °C or −20 °C for up to 72 h did not change the number of microvesicles relevantly (Supplementary Fig. 2). Therefore, the samples within this study were centrifugated at 750 g/5 min and stored frozen until the analysis.
Discussion
This study detected a similar distribution of the counts of CSF-borne microvesicles from AD patients and controls. Microvesicles derived from CSF of patients with AD had a reduced concentration of tau and APP protein. The results were replicated in an independent cohort.
This is one of the first studies that describe changes in the composition of neuronal microvesicles in the context of AD. Due to a high cell turnover and activation in patients with AD we expected an elevation of the microvesicle count. However, the inter-assay and inter-aliquot variability was high and may have obscured these differences. Since the relatively small cohorts allowed only the detection of large differences, we were intrigued that the tau and APP content differed significantly between patients with AD and controls and concluded that this is a pretty robust biomarker for AD.
Another problem is the age-difference of more than ten years between the study groups in both cohorts. The difference occurred because the samples had to be collected prospectively at the time of the lumbar puncture, when the diagnosis was not yet known. A balanced matching was not possible afterwards. However, as no correlation of age with the measurement parameters was found, it seems unlikely that the age difference interfered with the results. Nonetheless, the results need validation in a larger, age matched cohort.
As high inter-assay coefficients of variations were also reported in other studies, the question arises if flow cytometry is an appropriate method to quantify microvesicles31. Much effort has been undertaken to answer that question and the discussion is still controversial. While difficulties in standardization, measuring at the lower limit of detection, differentiation from background, swarming and fluorescent cross talk are serious problems, flow cytometry is still the only method which can distinguish membrane coated vesicles from other particles, determine the origin of the vesicle and allow the analysis of their size and form at the same time29. We propose not to use the particle count but the antigen detection (e.g. of tau) as diagnostic marker.
In previous studies, especially the impacts of the choice of a triggering signal as well as preanalytical handling have been investigated32. Linear fluorescence as trigger event is not recommended due to the unfavorable ratio of particle size to laser beam. This way, large amounts of unbound dye are registered together with the particle leading to a high background fluorescence and weakening the signal to noise ratio. Even AxV, a dye with a very high affinity cannot fully differentiate a microvesicle from background32. Furthermore, it is even in doubt, if all microvesicles bind AxV33,34. As a consequence, an unbiased triggering by front scatter combined with bead-based definition of particle size is recommended32. The Beckman & Coulter Gallios flow cytometer, used in this study was previously described as a superior instrument for measuring microvesicles based on forward scatter35.
Sampling, centrifugation and storage were reported to be critical for correct microvesicle analysis29,36. As recommended, samples within this study were processed within 30 minutes after sampling, agitation was avoided and centrifugation was optimized. For the measurement of microvesicles in blood, it was previously shown that low centrifugation is essential for absolute quantification but impairs separation from background noise37. In accordance with our data, others reported that no centrifugation leads to fragmentation of cells during freezing, but too high centrifugation reduced microvesicle counts considerably32,37. However the compromise, an intermedium centrifugation speed, as performed in our study, may lead to a higher variability in microvesicle counts when samples are frozen29. This holds also true for our experiments with inter-aliquot coefficients of variation of up to 41.3%. Therefore, the high inter-assay variation may in great parts be explained by the high inter-aliquot variations.
As specified above, microvesicles are expected to have a plethora of functions. Therefore, one can only speculate on the pathophysiological implications of our findings. As can be concluded from the missing correlation between soluble tau in CSF and the tau in microvesicles, the two parameters reflect different aspects of the tau pathology in AD. For soluble tau it is broadly accepted that it is released into the CSF during neuronal injury26,28. As microvesicles contain the cytoplasm of their cells of origin, microvesicle tau is supposed to display changes of intracellular tau metabolism.
On one hand, the reduced tau immunofluorescence may indicate that the binding epitope of the antibody is masked by phosphorylation, agglutination or by binding to carrier proteins38. This would be of special interest in terms of the hypothesis that microvesicles may also spread prion-like proteins39,40.
On the other hand a reduced tau concentration in microvesicles may be explained by an altered distribution of intracellular proteins. Li and colleagues have shown that the phosphorylation of tau leads to reduced concentrations in the axonal compartment and its accumulation in the somato-dendritic compartment41. As synaptic activity includes the generation of microvesicles, reduced axonal tau may explain reduced microvesicle tau5,42. Also, an impaired sorting of tau into exosomes has been observed after mTor dysregulation typically found in AD43. The observation that tau found in exosomes from early AD patients is highly phosphorylated also hints towards a relation between AD, tau phosphorylation and its sorting to extracellular vesicles44,45. The reduced concentration of tau in microvesicles may therefore correspond to the intra-neuronal tau hyperphosphorylation and accumulation in AD.
Interestingly, others found decreased synaptic proteins in exosomes of AD patients46. Together with our observations that several other proteins also tended to be less prevalent in microvesicles of AD and that the reduced levels of tau were highly correlated with the reduced levels of APP, a general disruption of the sorting process of proteins into microvesicles can be postulated. Recently, a mass spectrometry study revealed reduced concentrations of proteins associated with the function of extracellular vesicles in AD brains47. The authors also hypothesized a disturbed cellular clearance by a lack of function of extracellular vesicles.
Apart from the pathophysiological implications, the question was whether CSF microvesicles could serve as a biomarker for AD. With an area under the curves (AUC) between of 0.77 and 0.89 in our study, this seems possible. An advantage of this study was that the control group did not consist of healthy individuals but of patients who also presented with memory complaints but were not diagnosed with AD. The AUC has therefore to be interpreted in the context of differential diagnosis, a field in which established biomarkers also loose diagnostic accuracy48. However, due to the high coefficients of variation associated with the methodology, improvements in standardization have to be achieved until a diagnostic application is possible.
While this is the first study which shows changes in neuronal microvesicles, others have already shown increased numbers of myeloid exosomes and microvesicles in AD19,49. Therefore, CSF microvesicles as biomarkers for AD seem to be a promising option which deserves further methodological developments. Especially a replication in a larger and age-matched sample is needed. It will be interesting to see, whether neuronal microvesicles can also be detected in blood as it was previously shown for exosomes50.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ciregia, F., Urbani, A. & Palmisano, G. Extracellular Vesicles in Brain Tumors and Neurodegenerative Diseases. Frontiers in molecular neuroscience 10, 276, https://doi.org/10.3389/fnmol.2017.00276 (2017).
van der Pol, E., Boing, A. N., Gool, E. L. & Nieuwland, R. Recent developments in the nomenclature, presence, isolation, detection and clinical impact of extracellular vesicles. Journal of thrombosis and haemostasis: JTH 14, 48–56, https://doi.org/10.1111/jth.13190 (2016).
Beyer, C. & Pisetsky, D. S. The role of microparticles in the pathogenesis of rheumatic diseases. Nature reviews. Rheumatology 6, 21–29, https://doi.org/10.1038/nrrheum.2009.229 (2010).
Pan, B. T. & Johnstone, R. M. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell 33, 967–978 (1983).
Antonucci, F. et al. Microvesicles released from microglia stimulate synaptic activity via enhanced sphingolipid metabolism. Embo J 31, 1231–1240, https://doi.org/10.1038/emboj.2011.489 (2012).
Mahmoud, A. M. et al. Endothelial microparticles prevent lipid-induced endothelial damage via Akt/eNOS signaling and reduced oxidative stress. FASEB J 31, 4636–4648, https://doi.org/10.1096/fj.201601244RR (2017).
Kreutter, G. et al. Endothelial microparticles released by activated protein C protect beta cells through EPCR/PAR1 and annexin A1/FPR2 pathways in islets. Journal of cellular and molecular medicine 21, 2759–2772, https://doi.org/10.1111/jcmm.13191 (2017).
Colombo, E., Borgiani, B., Verderio, C. & Furlan, R. Microvesicles: novel biomarkers for neurological disorders. Frontiers in physiology 3, 63, https://doi.org/10.3389/fphys.2012.00063 (2012).
Huttner, H. B. et al. Increased membrane shedding–indicated by an elevation of CD133-enriched membrane particles–into the CSF in partial epilepsy. Epilepsy research 99, 101–106, https://doi.org/10.1016/j.eplepsyres.2011.10.029 (2012).
Huttner, H. B. et al. The stem cell marker prominin-1/CD133 on membrane particles in human cerebrospinal fluid offers novel approaches for studying central nervous system disease. Stem cells 26, 698–705, https://doi.org/10.1634/stemcells.2007-0639 (2008).
Lackner, P. et al. Cellular microparticles as a marker for cerebral vasospasm in spontaneous subarachnoid hemorrhage. Stroke 41, 2353–2357, https://doi.org/10.1161/STROKEAHA.110.584995 (2010).
Sheremata, W. A. et al. Evidence of platelet activation in multiple sclerosis. J Neuroinflammation 5, 27, https://doi.org/10.1186/1742-2094-5-27 (2008).
Lewczuk, P. et al. Cerebrospinal fluid and blood biomarkers for neurodegenerative dementias: An update of the Consensus of the Task Force on Biological Markers in Psychiatry of the World Federation of Societies of Biological Psychiatry. World J Biol Psychiatry, 1–85, https://doi.org/10.1080/15622975.2017.1375556 (2017).
Selkoe, D. J. & Hardy, J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med 8, 595–608, https://doi.org/10.15252/emmm.201606210 (2016).
Thompson, A. G. et al. Extracellular vesicles in neurodegenerative disease - pathogenesis to biomarkers. Nat Rev Neurol 12, 346–357, https://doi.org/10.1038/nrneurol.2016.68 (2016).
Joshi, P., Benussi, L., Furlan, R., Ghidoni, R. & Verderio, C. Extracellular vesicles in Alzheimer’s disease: friends or foes? Focus on abeta-vesicle interaction. International journal of molecular sciences 16, 4800–4813, https://doi.org/10.3390/ijms16034800 (2015).
Wang, Y. et al. The release and trans-synaptic transmission of Tau via exosomes. Mol Neurodegener 12, 5, https://doi.org/10.1186/s13024-016-0143-y (2017).
Vingtdeux, V., Sergeant, N. & Buee, L. Potential contribution of exosomes to the prion-like propagation of lesions in Alzheimer’s disease. Frontiers in physiology 3, 229, https://doi.org/10.3389/fphys.2012.00229 (2012).
Joshi, P. et al. Microglia convert aggregated amyloid-beta into neurotoxic forms through the shedding of microvesicles. Cell death and differentiation 21, 582–593, https://doi.org/10.1038/cdd.2013.180 (2014).
Yuyama, K. et al. A potential function for neuronal exosomes: sequestering intracerebral amyloid-beta peptide. FEBS Lett 589, 84–88, https://doi.org/10.1016/j.febslet.2014.11.027 (2015).
Blennow, K. & Zetterberg, H. The past and the future of Alzheimer’s disease CSF biomarkers-a journey toward validated biochemical tests covering the whole spectrum of molecular events. Frontiers in neuroscience 9, 345, https://doi.org/10.3389/fnins.2015.00345 (2015).
McGhee, D. J. et al. A systematic review of biomarkers for disease progression in Alzheimer’s disease. PLoS One 9, e88854, https://doi.org/10.1371/journal.pone.0088854 (2014).
Cummings, J., Lee, G., Mortsdorf, T., Ritter, A. & Zhong, K. Alzheimer’s disease drug development pipeline: 2017. Alzheimer’s & dementia 3, 367–384, https://doi.org/10.1016/j.trci.2017.05.002 (2017).
Morris, J. C., Mohs, R. C., Rogers, H., Fillenbaum, G. & Heyman, A. Consortium to establish a registry for Alzheimer’s disease (CERAD) clinical and neuropsychological assessment of Alzheimer’s disease. Psychopharmacology bulletin 24, 641–652 (1988).
Albert, M. S. et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7, 270–279, https://doi.org/10.1016/j.jalz.2011.03.008 (2011).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7, 263–269, https://doi.org/10.1016/j.jalz.2011.03.005 (2011).
Lewczuk, P. et al. Validation of the Erlangen Score Algorithm for the Prediction of the Development of Dementia due to Alzheimer’s Disease in Pre-Dementia Subjects. J Alzheimers Dis 48, 433–441, https://doi.org/10.3233/JAD-150342 (2015).
Jack, C. R. Jr. et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547, https://doi.org/10.1212/WNL.0000000000002923 (2016).
Chandler, W. L. Measurement of microvesicle levels in human blood using flow cytometry. Cytometry. Part B, Clinical cytometry 90, 326–336, https://doi.org/10.1002/cyto.b.21343 (2016).
Trummer, A., De Rop, C., Tiede, A., Ganser, A. & Eisert, R. Isotype controls in phenotyping and quantification of microparticles: a major source of error and how to evade it. Thrombosis research 122, 691–700, https://doi.org/10.1016/j.thromres.2008.01.005 (2008).
Lacroix, R. et al. Standardization of pre-analytical variables in plasma microparticle determination: results of the International Society on Thrombosis and Haemostasis SSC Collaborative workshop. Journal of thrombosis and haemostasis: JTH. https://doi.org/10.1111/jth.12207 (2013).
Poncelet, P. et al. Tips and tricks for flow cytometry-based analysis and counting of microparticles. Transfusion and apheresis science: official journal of the World Apheresis Association: official journal of the European Society for Haemapheresis 53, 110–126, https://doi.org/10.1016/j.transci.2015.10.008 (2015).
Connor, D. E., Exner, T., Ma, D. D. & Joseph, J. E. The majority of circulating platelet-derived microparticles fail to bind annexin V, lack phospholipid-dependent procoagulant activity and demonstrate greater expression of glycoprotein Ib. Thrombosis and haemostasis 103, 1044–1052, https://doi.org/10.1160/TH09-09-0644 (2010).
Rousseau, M. et al. Detection and quantification of microparticles from different cellular lineages using flow cytometry. Evaluation of the impact of secreted phospholipase A2 on microparticle assessment. PLoS One 10, e0116812, https://doi.org/10.1371/journal.pone.0116812 (2015).
Robert, S. et al. High-sensitivity flow cytometry provides access to standardized measurement of small-size microparticles–brief report. Arteriosclerosis, thrombosis, and vascular biology 32, 1054–1058, https://doi.org/10.1161/ATVBAHA.111.244616 (2012).
Lacroix, R. et al. Impact of pre-analytical parameters on the measurement of circulating microparticles: towards standardization of protocol. Journal of thrombosis and haemostasis: JTH 10, 437–446, https://doi.org/10.1111/j.1538-7836.2011.04610.x (2012).
Dey-Hazra, E. et al. Detection of circulating microparticles by flow cytometry: influence of centrifugation, filtration of buffer, and freezing. Vascular health and risk management 6, 1125–1133, https://doi.org/10.2147/VHRM.S13236 (2010).
Bancher, C. et al. Tau and ubiquitin immunoreactivity at different stages of formation of Alzheimer neurofibrillary tangles. Progress in clinical and biological research 317, 837–848 (1989).
Fevrier, B. et al. Cells release prions in association with exosomes. Proc Natl Acad Sci USA 101, 9683–9688, https://doi.org/10.1073/pnas.0308413101 (2004).
Smalheiser, N. R. Exosomal transfer of proteins and RNAs at synapses in the nervous system. Biology direct 2, 35, https://doi.org/10.1186/1745-6150-2-35 (2007).
Li, X. et al. Novel diffusion barrier for axonal retention of Tau in neurons and its failure in neurodegeneration. Embo J 30, 4825–4837, https://doi.org/10.1038/emboj.2011.376 (2011).
Frohlich, D. et al. Multifaceted effects of oligodendroglial exosomes on neurons: impact on neuronal firing rate, signal transduction and gene regulation. Philosophical transactions of the Royal Society of London. Series B, Biological sciences 369, https://doi.org/10.1098/rstb.2013.0510 (2014).
Tang, Z. et al. mTor mediates tau localization and secretion: Implication for Alzheimer’s disease. Biochim Biophys Acta 1853, 1646–1657, https://doi.org/10.1016/j.bbamcr.2015.03.003 (2015).
Fiandaca, M. S. et al. Identification of preclinical Alzheimer’s disease by a profile of pathogenic proteins in neurally derived blood exosomes: A case-control study. Alzheimers Dement 11, 600–607 e601, https://doi.org/10.1016/j.jalz.2014.06.008 (2015).
Saman, S. et al. Exosome-associated tau is secreted in tauopathy models and is selectively phosphorylated in cerebrospinal fluid in early Alzheimer disease. J Biol Chem 287, 3842–3849, https://doi.org/10.1074/jbc.M111.277061 (2012).
Goetzl, E. J. et al. Decreased synaptic proteins in neuronal exosomes of frontotemporal dementia and Alzheimer’s disease. FASEB J 30, 4141–4148, https://doi.org/10.1096/fj.201600816R (2016).
Musunuri, S. et al. Increased Levels of Extracellular Microvesicle Markers and Decreased Levels of Endocytic/Exocytic Proteins in the Alzheimer’s Disease Brain. J Alzheimers Dis 54, 1671–1686, https://doi.org/10.3233/JAD-160271 (2016).
Ewers, M. et al. CSF biomarkers for the differential diagnosis of Alzheimer’s disease: A large-scale international multicenter study. Alzheimers Dement 11, 1306–1315, https://doi.org/10.1016/j.jalz.2014.12.006 (2015).
Agosta, F. et al. Myeloid microvesicles in cerebrospinal fluid are associated with myelin damage and neuronal loss in mild cognitive impairment and Alzheimer disease. Ann Neurol 76, 813–825, https://doi.org/10.1002/ana.24235 (2014).
Mustapic, M. et al. Plasma Extracellular Vesicles Enriched for Neuronal Origin: A Potential Window into Brain Pathologic Processes. Frontiers in neuroscience 11, 278, https://doi.org/10.3389/fnins.2017.00278 (2017).
Acknowledgements
This work is supported by Grants from the Interdisciplinary Center for Clinical Research (IZKF), Erlangen. The research leading to these results also received support from the Innovative Medicines Initiative Joint Undertaking under EMIF Grant Agreement Nr. 115372, resources of which are composed of financial contribution from the European Union’s Seventh Framework Program (FP7/2007-2013) and EFPIA companies’ kind contributions. This work was partially supported by the German Research Foundation (DFG) (CRC1181 project C03) and by Ardea Biosciences, Inc. We acknowledge support from Deutsche Forschungsgemeinschaft (DFG) and Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) within the funding program Open Access Publishing. The present work was performed in fulfillment of the requirements for obtaining the degree “Dr. med” of LMR. We acknowledge support from Deutsche Forschungsgemeinschaft (DFG) and Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) within the funding program Open Access Publishing. We thank Janine Utz for proof reading the article.
Author information
Authors and Affiliations
Contributions
P.S., L.M.R., L.E.M., M.H. and J.M.M. designed the study. P.S., T.J.O., P.L., J.K. and J.M.M. investigated the patients and collected the samples. P.S., L.M.R., T.J.O. and L.E.M. carried out the experiments. M.H. provided permanent support as an expert of flow cytometric analysis of subcellular particles. Data was analyzed and evaluated by P.S., L.M.R., T.J.O., L.M., P.L., J.K., M.H. and J.M.M. The statistics were carried out by P.S. and L.M.R. P.S., L.M.R. and J.M.M. drafted the manuscript. All authors critically reviewed the manuscript and provided constructive comments to improve the quality of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
P.L. received consultation and lectures honoraria from Innogenetics, I.B.L. International, A.J. Roboscreen and Roche. P.S., L.M.R., T.J.O., L.M., J.K., M.H. and J.M.M. declare no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spitzer, P., Mulzer, LM., Oberstein, T.J. et al. Microvesicles from cerebrospinal fluid of patients with Alzheimer’s disease display reduced concentrations of tau and APP protein. Sci Rep 9, 7089 (2019). https://doi.org/10.1038/s41598-019-43607-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43607-7
This article is cited by
-
A new paradigm for diagnosis of neurodegenerative diseases: peripheral exosomes of brain origin
Translational Neurodegeneration (2022)
-
The localization of amyloid precursor protein to ependymal cilia in vertebrates and its role in ciliogenesis and brain development in zebrafish
Scientific Reports (2021)
-
Mechanisms of secretion and spreading of pathological tau protein
Cellular and Molecular Life Sciences (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.