Abstract
The development of hand osteoarthritis (HOA) could be linked to hyperlipidaemia. No longitudinal studies have addressed the relationship between serum lipid profile and HOA. The study aim was to determine the association between serum lipid profile and the incidence of radiographic hand osteoarthritis (RHOA). All women in a prospective population-based cohort from the Chingford study with available baseline lipid measurements and without RHOA on a baseline were included. Study outcome was the incidence of RHOA in year 11 of follow-up. Serum lipid profile variables were analysed as continuous variables and categorised into quartiles. The association between serum lipid profile and RHOA was modeled using multivariable logistic regression. Overall RHOA incidence was 51.6% (45.7–57.4%). An inverse association between HDL cholesterol levels and the incidence of RHOA was observed by quartile: OR of 0.36 [95%CI 0.17–0.75], 0.52 [95%CI 0.26–1.06], and 0.48 [95%CI 0.22–1.03]. Triglycerides levels showed a significant trend. No relationship was found with total or LDL cholesterol. Higher levels of HDL cholesterol appear to protect against RHOA after 11 years of follow-up. More research is needed to elucidate HOA risk factors, the mechanisms related to the lipid pathway, and the effects of lipid-lowering agents on reducing the incidence of OA.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a prevalent and disabling disease that contributes to increased co-morbidity and is more common in the elderly. The association between OA and cardiovascular disease (CVD) has attracted a large portion of research attention in recent years. These two health conditions frequently co-exist and the disease burden is only partly explained by age. Cardiovascular mortality is increased in individuals with OA1 and a high prevalence of CVD risk factors has been described in these individuals2,3,4, suggesting the existence of common pathogenic mechanisms. However, the causal association is not clear5.
Substantial evidence has also linked obesity and metabolic syndrome with OA6,7,8,9,10,11,12. In addition, recent experimental and epidemiological studies suggest that the biological mechanisms involved in the development of OA could be linked to atherosclerosis and the lipid metabolic pathway13,14,15,16, particularly in non-weight-bearing joints like those of the hand17,18,19. The estimated prevalence of radiological hand osteoarthritis (RHOA) in the elderly is about 80%, and there is evidence of sex-related and genetic predisposition. Risk factors such as age, manual labour, repetitive movement of the hand, overweight, smoking, and age at menopause have been associated with RHOA20. However, no longitudinal studies have addressed the relationship between serum lipid profile and OA in non-weight-bearing joints.
Our study aimed to determine if serum lipid profile is associated with incident radiographic hand osteoarthritis (RHOA).
Methods
Setting and participants
Participants were selected from the Chingford Women’s Study, a prospective, population-based cohort study that has been described in detail elsewhere21. Briefly, all women aged 45–64 years registered at a large general practice in Chingford, North London (UK), were contacted in 1988–1989 and asked to participate in a population-based study to evaluate risk factors for osteoporosis and OA. Of 1,353 women contacted, 1,003 (78%) attended the baseline visit (Y1) and signed their informed consent to participate. All women without RHOA on a baseline hand X-ray were included. The study participants were similar to women in the UK general population in terms of weight, height, and body mass index (BMI)12.
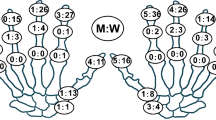
Radiographic assessment of RHOA
A standard hand X-ray was carried out at Y1 and at Y11. At both timepoints, RHOA was scored according to the Kellgren and Lawrence (K & L) scale by a single trained observer (DJH), blinded to clinical details, using the figures and legends of the original atlas22. The protocols used for radiographic classification and reproducibility have been previously reported23, 24. Briefly, observer kappa statistics for both the interphalangeal and carpo-metacarpal joint groups ranged from 0.7 to 1.0 without any significant differences in the reproducibility of the clinical and radiological measures. RHOA was considered to be present if the women had either proximal or distal interphalangeal joint OA (PIP and DIP, respectively) with a K & L score ≥2 in two or more joints. The outcome was defined as having RHOA at Y11.
Serum lipid profile measurements
The exposure of interest was the fasting serum lipid profile at the baseline visit (Y1): Total cholesterol (TC), HDL-cholesterol (HDL-c), LDL-cholesterol (LDL-c) and triglycerides (TG) at baseline, following a previously published protocol11.
Study variables and covariates
The following variables were characterized at baseline and included in the analysis: age, any current medication, diabetes medication, statins use, hormone replacement therapy (HRT), previous CVD, menopause, age at menopause, smoking, extent of job-related activity, body mass index (BMI), and systolic and diastolic blood pressure. Age, age at menopause, BMI, and systolic and diastolic blood pressure were treated as continuous variables. Smoking was classified as never smoked, ex-smoker, or currently smoking. Extent of activity on the job was classified as sedentary, half sedentary and half active, and predominantly manual, obesity as BMI ≥ 30, and daily sports activity as none, light (1 hour walking, bowling, golf, badminton, cycling, or swimming), moderate (2 hours of light sport or 1 hour keep-fit or aerobics activity) and intensive (>1 hour keep-fit or aerobics, squash).
Statistical analysis
Continuous variables were described as mean and standard deviation and categorical variables as percentages. Differences between groups were based on the t-test or chi-square, as appropriate. Cumulative incidence and 95% confidence intervals (CI) for RHOA were also calculated for a 11-year follow-up period.
Logistic regression models were used to evaluate the association between lipid serum profile and incidence of RHOA at Y11. Lipid serum profile was considered as both a continuous and categorical set of variables to evaluate the effect of a potential dose-response relationship with RHOA. Three different models were built to explore this association: Model 1 was non-adjusted, Model 2 was age-adjusted, and Model 3 added the potential confounders that were epidemiologically relevant or statistically significant in the bivariate analysis. Log-rank test was used to contrast the dose-response relationship within serum lipid profile categories.
We used STATA software (version 12) for all the analysis, with two-sided tests. P-values < 0.05 were considered statistically significant.
The study was approved by the Outer North East London Research Ethic Committee and conducted according the rules of good research practices of the Declaration of Helsinki. Each study participant provided written informed consent before participating.
Results
Of the 1,003 women participating at baseline, 306 were lost to follow-up (30%) and 697 completed the year 11 follow-up, of which 313 (45%) had RHOA at baseline and 107 (15%) had no baseline lipid serum profile measurements data. The final sample available for analysis was 277 (40%) participants. Baseline participant characteristics are reported in Table 1 and the study flowchart is shown in Fig. 1.
The final study population was younger and had a healthier cardiovascular profile than women lost to follow-up and those without serum lipid profile measurements, although the percentages of smokers and of women with manual-labour jobs were higher in the final study population, compared to those without lipid profile measurements.
The mean age of the final study population was 50.4 (SD: 4.8) years and BMI was 24.8 (SD: 3.9). About 59% were post-menopausal, 19% had a predominantly manual-labour job, and just 8.6% were classified as obese.
Association between lipid serum profile and RHOA
Overall cumulative RHOA incidence was 51.6% [45.7–57.4%]. Compared to those without RHOA at Y11, incident RHOA women were older (51.1 [SD: 5.0]), more likely to take blood pressure medication (13.95% vs 7.9%) and had higher mean levels of triglycerides at baseline [1.0 (0.6) vs (1.2 (0.7)], with no other significant differences (Table 2).
Crude data and age- and fully adjusted logistic regression modelling results are detailed in Table 3. No significant association was found between continuous HDL-c and incident RHOA. HDL-c levels were inversely associated with the incidence of RHOA, with crude OR 0.32 [95%CI 0.16–0.66], 0.50 [95%CI 0.25–0.99], and 0.50 [95%CI 0.23–1.04] for the 2nd, 3rd, and 4th quartiles compared to the 1st quartile (reference group); this association remained unchanged and showed a significant trend after adjusting for all pre-specified confounders (OR: 0.36 [95%CI 0.17–0.75], 0.52 [95%CI 0.26–1.06], and 0.48 [95%CI 0.22–1.03], respectively).
Conversely, TG levels were directly associated with RHOA incidence in the unadjusted continuous logistic model but the association was not significant after adjustment for age. Test for linear trend was significant in the fully adjusted categorical logistic model. No associations were found with TC and LDL-c levels and RHOA over 11 years of follow-up.
Discussion
In this population-based cohort study, higher levels of HDL-c were found to be associated with a lower incidence of RHOA over 11 years of follow-up. Conversely, the effect size observed in each TG category showed an increased, but not significant, risk for HOA. However, TG levels seem to confer a higher risk of RHOA according to the trend in test results.
Our results disagree with those of a previous cross-sectional study in the Chingford cohort11, in which the authors found an association between radiological knee OA and moderately elevated TC but no association between knee OA and higher levels of LDL-c, TG, or HDL-c. In a subanalysis in women with both hand and knee OA, no association was found between any of the components of the serum profile and OA. Our study, based on the same cohort, showed a significant association and a trend in HDL-c because of differences in study design and baseline characteristics of the women included. In the previous study, women with previous RHOA were included, and they were older and had a worse CVD profile, compared to our study participants.
Other studies have shown contradictory results on the relationships between TC, TG, LDL-C and OA incidence. The Rotterdam study8, which aimed to analyse the connection between HOA and overweight, detected no association between HOA and TC/HDL-c ratio, whereas our findings that HDL-c levels and TG levels were associated with HOA are consistent with other studies such as those of Davis-Tuck, who found higher levels of TC and TG associated with bone marrow lesions in asymptomatic middle-aged women25 and Frey, who showed an association between incident HOA and hyperlipidaemia, particularly at younger ages but could not analyse the effect of serum lipid profile on HOA as it was modified because of statin exposure26. Our study population was similar in age and cardiovascular profile to all three of these earlier studies.
Mechanisms through which lipid metabolism could lead to OA still must be fully elucidated. There is evidence that higher HDL-c levels in the synovial fluid have a protective effect27, vascular insults affecting the bone marrow next to the cartilage25, and the toxic effect of cholesterol at the joint itself 28 might contribute to the development of OA. We were able to detect the protective effect of HDL-c and TG on RHOA as a trend in our population, but not an increased risk of RHOA with high TC or LDL-c levels. High HDL-c levels might be present in healthier individuals with better physical status and lower prevalence of comorbid conditions29, which could also lead to a lower prevalence and incidence of OA. Women in our study were younger and had normal weight to overweight, better cardiovascular profile, and no previous cardiovascular disease, compared to other studies7, 11, 17, 18.
Potential limitations of this study should be mentioned. First, the power of the study to show significant effects might be limited as we only included 40% of the total eligible population, given the combination of high baseline prevalence (45%) of RHOA and the lack of data on cholesterol levels for 15% of the patients. Differences between these 277 participants and the rest of the women included must be considered and could limit the generalizability of our findings. Women included in the study were healthier and younger than those excluded, which might partly explain the lack of association between incident RHOA and certain components of the lipid serum profile, but also might explain the observed association with other components of serum profile, such as TG and HDL-c levels25, 26.
Secondly, serum lipid profile was only measured at Y1, and we were not able to determine if the lipid levels detected were previously present or simply reflected an increase at the time of measurement that could be influenced by day-to-day diet and random error. In the same way, changes in lipid serum levels between Y1 and Y11 were not reported, which prevented us from drawing any conclusion regarding the possible impact of serum lipid variations on the outcome or the time lapse between the increase or decrease of these lipids and the outcome. Nonetheless, baseline risk factors may be connected in the overall life-course trajectories.
Thirdly, other unmeasured confounders, such as diet, activity of daily living, or socioeconomic status could have influenced our results.
Finally, we had no information on lipid-lowering drugs taken by our population at either baseline or during follow-up, which could have influenced the nonsignificant association observed between TC and RHOA. We would speculate, however, that the proportion of women treated with such therapies was low at the time of recruitment, as statins had not yet been launched on the market.
Conclusion
No significant associations between serum lipid profile and RHOA were found after 10 years of follow-up, although significant trends were observed in HDL-c and TG associations. Higher HDL-c levels appear to be protective and higher TG levels seem to confer a higher risk of RHOA.
Treatments available today for RHOA are mainly focused on the symptomatic relief and functional improvement of the joints affected. The burden of OA is bound to increase due to the lack of effective disease-modifying therapies. With this in view, more research is needed to elucidate the aetiology and risk factors of HOA and, specifically, the mechanisms related to the lipid pathway as well as to the potential effects of lipid-lowering agents on the reduction of OA incidence. New pharmacological interventions, especially at early stages, could reduce OA incidence and influence the progression of the disease.
References
Hawker, G. A. et al. All-Cause Mortality and Serious Cardiovascular Events in People with Hip and Knee Osteoarthritis: A Population Based Cohort Study. PloS One. 9(3), e91286 (2014).
Nielen, M. M. J. et al. Cardiovascular disease prevalence in patients with inflammatory arthritis, diabetes mellitus and osteoarthritis: a cross-sectional study in primary care. BMC Musculoskelet Disord 13, 150 (2012).
Singh, G., Miller, J. D., Lee, F. H., Pettitt, D. & Russell, M. W. Prevalence of cardiovascular disease risk factors among US adults with self-reported osteoarthritis: data from the Third National Health and Nutrition Examination Survey. Am J Manag Care 8(15 Suppl), S383–91 (2002).
Kadam, U. T., Holmberg, A., Blagojevic, M., Nilsson, P. M. & Akesson, K. Risk factors for cardiovascular disease and future osteoarthritis-related arthroplasty: a population-based cohort study in men and women from Malmö, Sweden. Scand J Rheumatol 40(6), 478–85 (2011).
Conaghan, P. G., Vanharanta, H. & Dieppe, P. A. Is progressive osteoarthritis an atheromatous vascular disease? Ann Rheum Dis 64(11), 1539–41 (2005).
Engström, G., Gerhardsson de Verdier, M., Rollof, J., Nilsson, P. M. & Lohmander, L. S. Protein, metabolic syndrome and incidence of severe hip and knee osteoarthritis. A population-based cohort study. Osteoarthritis Cartilage 17(2), 168–73 (2009).
Yoshimura, N. et al. Accumulation of metabolic risk factors such as overweight, hypertension, dyslipidaemia, and impaired glucose tolerance raises the risk of occurrence and progression of knee osteoarthritis: a 3-year follow-up of the ROAD study. Osteoarthritis Cartilage 20(11), 1217–26 (2012).
Dahaghin, S., Bierma-Zeinstra, S. M. A., Koes, B. W., Hazes, J. M. W. & Pols, H. A. P. Do metabolic factors add to the effect of overweight on hand osteoarthritis? The Rotterdam Study. Ann Rheum Dis 66(7), 916–20 (2007).
Stürmer, T., Günther, K. P. & Brenner, H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol 53(3), 307–13 (2000).
Grotle, M., Hagen, K. B., Natvig, B., Dahl, F. A. & Kvien, T. K. Obesity and osteoarthritis in knee, hip and/or hand: an epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet Disord 9, 132 (2008).
Hart, D. J., Doyle, D. V. & Spector, T. D. Association between metabolic factors and knee osteoarthritis in women: the Chingford Study. J Rheumatol 22(6), 1118–23 (1995).
Hart, D. J. & Spector, T. D. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. J Rheumatol 20(2), 331–5 (1993).
Gkretsi, V., Simopoulou, T. & Tsezou, A. Lipid metabolism and osteoarthritis: lessons from atherosclerosis. Prog Lipid Res 50(2), 133–40 (2011).
Dumond, H. et al. Evidence for a key role of leptin in osteoarthritis. Arthritis Rheum 48(11), 3118–29 (2003).
Aspden, R. M., Scheven, B. A. & Hutchison, J. D. Osteoarthritis as a systemic disorder including stromal cell differentiation and lipid metabolism. Lancet 357(9262), 1118–20 (2001).
de Munter, W. et al. Cholesterol accumulation caused by low density lipoprotein receptor deficiency or a cholesterol-rich diet results in ectopic bone formation during experimental osteoarthritis. Arthritis Res Ther 15(6), R178 (2013).
Stürmer, T. et al. Serum cholesterol and osteoarthritis. The baseline examination of the Ulm Osteoarthritis Study. J Rheumatol 25(9), 1827–32 (1998).
Hoeven, T. A. et al. Association of atherosclerosis with presence and progression of osteoarthritis: the Rotterdam Study. Ann Rheum Dis 72(5), 646–51 (2013).
Jonsson, H. et al. Hand osteoarthritis in older women is associated with carotid and coronary atherosclerosis: the AGES Reykjavik study. Ann Rheum Dis 68(11), 1696–700 (2009).
Kalichman, L. & Hernández-Molina, G. Hand Osteoarthritis: An Epidemiological Perspective. Semin Arthritis Rheum 39(6), 465–76 (2010).
Schwarz, K. The Chingford Study. Public Health Nov 95(6), 347–52 (1981).
The Epidemiology of Chronic Rheumatism: Atlas of Standard Radiographs of Arthritis. (Blackwell Scientific, 1963).
Hart, D. J. et al. Clinical signs of early osteoarthritis: reproducibility and relation to x ray changes in 541 women in the general population. Ann Rheum Dis 50(7), 467–70 (1991).
Hart, D., Spector, T., Egger, P., Coggon, D. & Cooper, C. Defining osteoarthritis of the hand for epidemiological studies: the Chingford Study. Ann Rheum Dis 53(4), 220–3 (1994).
Davies-Tuck, M. L. et al. Total cholesterol and triglycerides are associated with the development of new bone marrow lesions in asymptomatic middle-aged women - a prospective cohort study. Arthritis Res Ther 11(6), R181 (2009).
Frey, N., Hügle, T., Jick, S. S., Meier, C. R. & Spoendlin, J. Hyperlipidaemia and incident osteoarthritis of the hand: a population-based case-control study. Osteoarthritis ad Cartilage: 1–6 (2017).
Oliviero, F. et al. Apolipoprotein A-I and cholesterol in synovial fluid of patients with rheumatoid arthritis, psoriatic arthritis and osteoarthritis. Clin Exp Rheumatol 27(1), 79–83 (2009).
Tabas, I. Consequences of cellular cholesterol accumulation: basic concepts and physiological implications. J Clin Invest 110(7), 905–11 (2002).
Ko, D. T. et al. High-Density Lipoprotein Cholesterol and Cause-Specific Mortality in Individuals Without Previous Cardiovascular Conditions: The CANHEART Study. J Am Coll Cardiol 68(19), 2073–83 (2016).
Author information
Authors and Affiliations
Contributions
N.A., T.S., and D.H. contributed to the intellectual conception and the design of the study and approved the final version of the manuscript. N.A. has significantly contributed to the interpretation of the results. D.P., M.G.G., M.S., R.R., and C.R. have contributed to the statistical analysis, interpretation of the results, to manuscript writing and review, and have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garcia-Gil, M., Reyes, C., Ramos, R. et al. Serum Lipid Levels and Risk Of Hand Osteoarthritis: The Chingford Prospective Cohort Study. Sci Rep 7, 3147 (2017). https://doi.org/10.1038/s41598-017-03317-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03317-4
This article is cited by
-
Metabolic syndrome increases osteoarthritis risk: findings from the UK Biobank prospective cohort study
BMC Public Health (2024)
-
The association between lipid biomarkers and osteoarthritis based on the National Health and Nutrition Examination Survey and Mendelian randomization study
Scientific Reports (2024)
-
Risk of metabolic abnormalities in osteoarthritis: a new perspective to understand its pathological mechanisms
Bone Research (2023)
-
Inflammaging and Osteoarthritis
Clinical Reviews in Allergy & Immunology (2022)
-
The CH25H–CYP7B1–RORα axis of cholesterol metabolism regulates osteoarthritis
Nature (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.