Abstract
Assessment of human movement performance in activities of daily living (ADL) is a key component in clinical and rehabilitation settings. Motion capture technology is an effective method for objective assessment of human movement. Existing databases capture human movement and ADL performance primarily in the Western population, and there are no Asian databases to date. This is despite the fact that Asian anthropometrics influence movement kinematics and kinetics. This paper details the protocol in the first phase of the largest Asian normative human movement database. Data collection has commenced, and this paper reports 10 healthy participants. Twelve tasks were performed and data was collected using Qualisys motion capture system, force plates and instrumented table and chair. In phase two, human movement of individuals with stroke and knee osteoarthritis will be captured. This can have great potential for benchmarking with the normative human movement captured in phase one and predicting recovery and progression of movement for patients. With individualised progression, it will offer the development of personalised therapy protocols in rehabilitation.
Measurement(s) | voluntary movement behavior • grip strength measurement • Pinch Strength |
Technology Type(s) | motion capture system • force plates • sensor • dynamometry |
Factor Type(s) | gait • Timed Get Up and Go Test • balance • reaching • key turning • hand to mouth • hand to back • hand on head • cross obstacle • folding towel • step up and down |
Sample Characteristic - Organism | Homo sapiens |
Sample Characteristic - Location | Asia |
Machine-accessible metadata file describing the reported data: https://doi.org/10.6084/m9.figshare.12808187
Similar content being viewed by others

Background & Summary
Three-dimensional motion capture system using reflective markers provides accurate and precise data to describe joints angular movement quality1,2,3. Joint movements which are hard to be quantified using traditional methods, such as shoulder elevation4, scapular movements5, and knee valgus6 can be assessed with the motion capture system during functional activities. Recent studies have adopted this technique to capture the action during activities of daily living (ADL) and functional tasks in both upper limbs4,7,8 and lower limbs9. Clinically, it is important to assess the level of impairment and function in people with movement impairment, such as individuals with stroke, to track the level of recovery and determine the efficacy of treatments. Most of the standardised clinical assessments summarise the patients’ performance with a total score or collapse a time-varying movement data into a point estimate. In doing so, most of the information including variability in temporal and spatial domains cannot be captured. As a result, these tools are insensitive in picking up subtle changes in motor performance and detecting abnormalities in patients with high function10.
One of the objectives of movement analysis is to determine whether a movement deviates from the average11,12. Knowledge about normal kinematics in extremities and trunk during functional tasks could provide a basis to evaluate the level of recovery and effect of rehabilitation interventions, as the regain of normal movement pattern is always treated as a benchmark of motor recovery7,13. For example, Aboelnasr et al.14 assessed the quality of reaching movement in children with cerebral palsy by comparing their movement with normally developing children. In addition to the overall completion time, the level of jerkiness and spatial inaccuracy of hand control were able to be captured and compared between the two groups14. Thus, this approach could maximise the information gained from clinical assessments15,16.
There are a few open access electronic databases that provide kinematic and/or kinetic data on human participants, including HuMoD Database17, Berkeley Multimodal Human Action Database18, CMU Graphics Lab Motion Capture Database19 and KIT Whole-Body Human Motion Database20. The HuMoD Database17 provides both raw and processed kinematic and kinetic data as well as electromyographical measurements. This database contains motion capture data of 8 lower limbs tasks (e.g. walking, kicking ball, squatting) which were performed by one female (27 yrs, 161 cm, 57 kg) and one male participant (32 yrs, 179 cm, 85 kg). The Berkeley Multimodal Human Action Database18 contains 11 actions performed by 12 participants (7 male and 5 female). 11 of these participants were between 23–30 years old, with one elderly participant. This database mainly comprises of actions with high dynamics such as jumping jacks, throwing and hand clapping. The CMU Graphics Lab Motion Capture Database19 provides a wide range of motion capture data, including the interaction between human participants, sports activities (e.g. basketball, dance) and ADLs (e.g. sweeping floor, washing window). There were a total of 144 participants and each participant generated different motions. The ongoing KIT Whole-Body Human Motion Database20 captures the motions from 224 participants (with 106 males, 37 females and the rest of the participants without gender specified) and 127 different objects (e.g. cup, basket) and environmental elements (e.g. staircase, seesaw) with which the participant is interacting. These open access databases have recorded numerous motion capture data of healthy individuals. Nevertheless, none of these databases attempted to capture the motion of the Asian population. Ethnicity has been reported to be influential for both body proportion and body composition21,22. In addition, anthropometry differences exist between ethnic groups23,24. Within Southeast Asia, populations from neighbouring countries have different body dimensions23,25, and so do people of historically highly associated ethnic groups in East Asia24. Up to half of the body dimensions measured were significantly different between the Singaporean and Indonesian adult25, and the former had the greatest stature compared to other Asian populations26. Differences were also found when comparing the Singaporean Chinese elderly population to those in Malaysia and Chinese living in Beijing26. Thus, establishing a movement database for Asian population is warranted.
The current work aims to establish a normative movement database containing kinetic and kinematic data of 500 healthy adults. It represents our latest effort in building an Asian-centric movement database that focuses on the activities of daily living. Kinematics and kinetics data of 12 upper and lower body tasks were captured. These tasks were either selected from a standardised assessment tool or were representative of daily functional activities such as reaching to grasp an object, turning a key in a lock and walking. The large sample size allows us to capture variations of normal movement patterns, which could provide sufficient data for data-driven healthcare and rehabilitation services, and building machine learning models.
The study protocol is described in this article. Data from 10 participants which captured using the described protocol are available27.
Methods
Participants
A total of 500 healthy participants (aged 21-80) of Asian ethnicity will be recruited for this study. Exclusion criteria include: (1) declared prior neurological conditions, surgeries, or medical conditions that need active medical or therapy intervention in the last three months, (2) declared depression or mental health issues affecting daily task performance, (3) declared visual problems that resulted in a recent accident, fall, or near-fall, (4) having skin lesions or known skin allergies that would hinder markers placement, (5) inability to participate normally in daily living tasks due to pain, or (6) pregnancy. In this paper, we report the protocol details and the data from ten healthy participants who have completed the trial. See Table 1 for basic demographics and body measurements. This study was approved by the Nanyang Technological University Institutional Review Board (IRB-2018-04-014). Recruitment methods include flyer advertisements posted in public areas, word of mouth, visiting organisations to share information about the study, exhibition booths at events such as conferences and various community centres. There will be an even distribution of participants for each age group range and gender. The proportion of ethnic group will mirror the ethnic group distribution in Singapore (Chinese: 75%, Malay: 13%, Indian: 9%, others: 3%)28. To ensure that all ethnic groups are captured, recruitment will include sharing information about the study at specific ethnic group associations.
Experimental set-up and equipment
All trials were conducted in the motion capture laboratory of Rehabilitation Research Institute of Singapore (RRIS).
Motion capture system
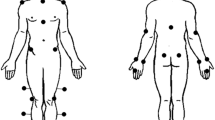
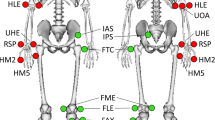
Three-dimensional human movement data was captured using sixteen 2 megapixels Miqus M3 motion capture system (Qualisys, AB, Sweden), with a field of view (FOV) of 64 × 41 degrees. Retro reflective optical markers were placed on the body of a participant according to the marker placement set (Fig. 1). The marker set was based on a modified Calibrated Anatomical System Technique (CAST), which has a diameter of 12.5 mm (for the body) and 10 mm (for finger tips). The motion capture cameras emit infrared strobe, which will be reflected back by the markers. In this way, the cameras are able to capture and record the movement trajectory of the body. The Qualisys Track Manager (QTM) v2019 served as an integrated software interface for seamless and easy-to-use data recording. QTM is capable of synchronizing the cameras with external devices, such as force plates and other electromechanical sensors. The trajectories of the markers and data from external devices were captured synchronously at 200 and 2000 Hz rate respectively.
Force plates
Two 60 × 50 x 5 cm force plates (Type 9260AA6, Kistler, Switzerland) were positioned on the floor to record the three-dimensional ground reaction force during lower limb tasks. (See Fig. 2).
Other equipment and sensorised items
Participant was seated in front of a table on a chair that was designed in-house. The sitting area of the chair was about 39 × 83 cm. The chair height could be adjusted between 41 – 59 cm, and its backrest could also be adjusted to different angles and heights to suit different participant’s torso height. The sensorised chair had a tension and compression load cell (FSH04207, FUTEK Inc., USA) installed at the backrest of the chair. See Fig. 3a,b. The chair was also connected with two mini push-button switches that were embedded in a cover to be used as left and right lap sensors (Fig. 3c).
The AmpDesk table (ErgoEdge, Singapore) with an adjustable height was customised for the study. Two load cells (C2G1, Pavone Sistemi, Italy) were embedded to measure force exerted on the table by each hand during upper limb trials. Conductive fabric (EeonTex, SparkFun Electronics) was affixed over different section of the table, a cube detection plate and also the Action Research Arm Test (ARAT) shelf (Fig. 4a). These conductive fabrics were connected to programmed microcontrollers and acted as contact capacitive touch sensors that allowed us to measure the precise moment an object comes into or is removed from contact with the hand. Conductive fabric also covered the contact surface of a cube and cylinder (Fig. 4b) used in the protocol during Forward-Reach Grasp and Lateral-Reach Grasp tasks respectively. This enabled the capacitive touch capability of the fabric on the table to be extended to the cube and cylinder.
A fixture with a key-like object was designed to capture supination and pronation of the forearm (Fig. 5) during a task that required the participant to simulate locking and unlocking a door with key. The key-like object had a sub miniature load button (FSH03879, FUTEK Inc.) embedded inside to measure the pinch force during the task. The height of the key was 97 cm from the ground which was within the Building and Construction Authority of Singapore’s recommended height of 90 cm to 110 cm29.
Dynamometer
Jamar Plus + Digital Hand Dynamometer and Jamar Digital Pinch Gauge (Sam-mons Preston, Bolingbrook, IL, USA) were used to assess grip strength and lateral pinch strength.
Procedure
Participants were encouraged to wear appropriate attire for the data collection (e.g. shorts or exercise tights and a tight fitting singlet). Clothing should be dark in colour with minimal reflective material. In cases where participants did not have appropriate attire, the research team provided clothing.
Basic anthropometry, demographic and lifestyle information were taken, e.g. height, weight, marital status, level of education. Basic strength tests for the upper limb was conducted using the Jamar dynamometer. Markers were placed onto the participant’s body according to the Marker placement protocol illustrated in Fig. 1. For the forearm markers, they were affixed onto a rigid body that was modified to capture forearm movements more effectively (See Fig. 6)30.
After the markers were placed on the participant, a static trial was taken so that all markers could be seen. A static calibration pose (shoulder abduction 45 degrees, elbow fully extended, palms facing forward) was held for at least two seconds.
Following the static trial, participants went through a series of 12 tasks, consisting of 6 upper limb and 6 lower limb tasks. The sequence of the task was based on block randomization, which was determined by throwing a dice prior to the trial. This randomization was done to minimize bias due to mental and physical fatigue during the trial. Table 2 details the sequence of tasks in each block.
In each task, the participant was first provided with a short explanation and shown task demonstrations by an experimenter. This was followed by a few familiarization and practice trials. The actual trial would commence once the participant confirmed that the instructions given had been understood.
For the upper limb tasks, participants repeated each action for 6 times per limb, that is, the dominant then non-dominant limb. For the lower limb tasks, participants repeated each action for 3 times per limb. A 10-15 minute break was given to the participants between upper and lower limb tasks. The 12 tasks were selected based on expert advice from occupational therapists and physiotherapists. Each task represented an important movement required to complete everyday functional tasks.
For all the six upper limb tasks detailed below, the chair was set up so that the participant’s hip and knee flexion was at approximately 90 degrees and participants were instructed to keep their feet flat on the ground throughout the tasks31. For tasks three to five, participants were instructed to keep their back against the backrest.
The following section describes the 12 tasks in the protocol. Figures 7 and 8 are images of the task being performed by an internal staff of the research institute. Written consent was obtained from the staff for the use of his image.
-
1.
Folding Towel
Folding towel was a test extracted from a standardised assessment known as the Wolf-Motor Function Test32. This task assessed the participant’s ability in manipulating objects used with daily living. Bilateral limb coordination could be evaluated since synchronization of hands movement was required in performing this task. The participants were required to fold the towel, that has a size of 55.5 x 29 cm, once from top to bottom, and then fold it another time from one side to another.
-
2.
Forward Reach-grasp
This task was extracted from Action Research Arm Test31. This test assessed the participant’s ability in manipulating the cube including controlled grasp and release. The voluntary control of shoulder flexion combined with elbow extension was also assessed. In patient with brain lesions, this movement pattern is sometimes impaired due to the abnormal shoulder-elbow coupling. The participants were required to grasp a cube (7.5 cm3) with conductive fabric on the table and transport it to the top of the shelf. The cube would then remain on the shelf while the hand would return to the starting position. The grip used to grasp the cube had to be with the forearm in a neutral position and a grip over the top of the block was not permitted. The experimenter brought the block down to starting position and participant waited for the cue from the experimenter to repeat the subsequent movement.
-
3.
Lateral reach-grasp
This test assessed the participant’s ability in performing a cylinder grip and transferring an object across the body midline. Truncal compensation would also be observed since it is one of the indicators of dynamic sitting balance33. The starting position was similar to the forward reach-grasp task. Here, the participant would reach across the midline to grasp the object positioned in line with the opposite shoulder at maximum reach. Once grasped, the object was transported horizontally to be in line with the shoulder of the arm being tested. The positioning of the object was marked prior to the task to ensure it was consistent across the trials. During the task, the position of the supporting hand remained on the table.
-
4.
Hand to mouth
This task was extracted from Action Research Arm Test31 which simulated the gross movement during feeding. The activity was to lift the hand, place the hand on the mouth and then back to the initial position on the lap.
-
5.
Hand to head
This task was extracted from Action Research Arm Test31 which simulated the gross movement during hair combing. Participants lifted up the hand to place it on the top of the head, and brought it back to the initial position on the lap.
-
6.
Hand to back
This task simulated the movement during back washing. This movement is important, for example, for showering or personal hygiene. The task began with the hands pronated on the lap. The participants moved their hand being tested towards their lower back, targeting the middle of their lower back with their palm. During the task, the position of the supporting hand remained on the lap.
-
7.
Timed Up and Go (TUG)
The TUG is one of the standardised tests in assessing functional mobility in clinical setting34,35,36. Multiple transitional movements, including sit-to-stand and turning, were involved in the test which make the performance of the test highly relevant to the locomotion function in ADLs36. The participant was seated and the starting position of the feet was on the force plate.
-
8.
Key turning
Participants performed this task in standing, with the body erect and feet at hip distance apart, facing towards the key rig and both arms relaxed in neutral position at side of body. The participants brought the hand to hold the key, and turned the key in a clockwise direction to simulate locking the door followed by an anticlockwise direction to simulate unlocking the door.
-
9.
Balance
This task was extracted from the Berg Balance Scale37. The task challenged the participant’s anticipatory postural adjustment and the ability to move the center of gravity in the superoinferior direction. A previous study has shown that this item demonstrated the strongest power in differentiating faller from non-faller in elderly38. This item is rated on a 5‐point ordinal scale in the Berg Balance Scale clinically. In this particular task, participants to stand upright with hands relaxed at their sides and each foot on either side of the force plate. Following a cue, they had to bend downwards to pick up an object off the floor. Once the object was grasped, they had to return to the standing position and pass the object to the experimenter. Both feet remained in the same position throughout unless the participant self-initiated a compensatory strategy by adjusting their foot position in order to perform the task.
-
10.
Obstacle crossing
This task was used to simulate crossing an obstacle, for example, in a bathroom. The ability to clear foot from floor and the coordination between stance and swing limb would be assessed in this task39. The participant began standing facing the direction of the walkway with both hands relaxed at the side. Participant would step over the obstacle placed across the walkway with one foot at a time. The movement was completed when both feet were on the other side of the obstacle.
-
11.
Step up and down
Stepping up and down is essential for community ambulation and functional independence. The task can be demanding for people with motor impairment since it required high level of dynamic balance ability and at the same time challenging their concentric and eccentric lower-limbs muscle strength40. The task involved a standing platform (60 cm length x 50 cm width x 15 cm height) that was placed on the force plate area. During the task, the participants were required to step from the flat ground onto the platform one leg at a time. They would then walk to the edge of the platform before stepping off the step. This task simulated daily activities involving crossing a kerb.
-
12.
10 m Walk
The 10 m Walk test is considered one of the core assessments for lower-limb function in rehabilitation41,42. Kinetic and kinematics information obtained from this walking task would allow the participant’s gait to be analysed. Clinically, gait analysis has been used to diagnose pathology and evaluate the effectiveness of intervention43. The participant was required to walk a total distance of 10 metres, which was mapped out with a demarcated start and finish line along the walkway. Throughout the task, the participant was instructed not to look at the ground, where the force plates were installed, but to look straight ahead to a far distance object.
Data Records
Raw data captured consisted of the marker coordinates that were synchronized with information recorded by the force plate and sensorised items. Markers were labelled and missing data were gap filled using the QTM software (Qualisys Track Manager, proprietary software that comes with Qualisys MOCAP). Data were saved in.qtm format (which is a proprietary file format for Qualisys) but converted to c3d format for data sharing. c3d format is widely supported in many motion capture systems (Qualisys, Vicon), analysis software (Visual3D), or commonly used language library (python, R, Matlab). The benefit of saving in c3d format is that most information can be saved in a single file (marker trajectories, analog data, force data). 10 trials data are publicly available at NTU Dataverse (https://doi.org/10.21979/N9/7VF22X)27.
One unique folder was created for each participant which contain data files (in c3d format) from both lower limb and upper limb tasks and the static pose. The folders were labelled ‘SNxxx’, where xxx is an integer value representing the participant number (for example SN001). Each file was systematically named as ‘SNxxx_<file-number>_<abbreviated-task-name>_<side><recording-number>’. For example, SN001_0028_towel_R02 denotes the data file for participant SN001 performing the folding towel task using the right arm in the second recording. Full lists of task name used in file naming are shown in Table 3.
Each c3d file contained multiple data stored into a single file: marker trajectories data (under Video Data group), sensor data (under Analog Data group, see Table 4 for full list of sensors used) and force data (under Analog Data group, see Table 5 for full list of force signal). Important parameters were saved under respective group as well (POINT, ANALOG, FORCE_PLATFORM). For example POINT:RATE referred to the sampling rate used in MOCAP. Force data consisted of raw output signal from the sensor embedded in the force plate. Ground reaction force and center of pressure (COP) were derived from output signal using the formula provided (https://isbweb.org/software/movanal/vaughan/kistler.pdf).
Technical Validation
To ensure that the data collection procedure is reliable, the markers were placed by researchers who are trained by clinicians. The clinicians provided training and hands-on guidance and ensured that the researcher is competent to do so on their own.
The reliability of marker placement had been evaluated in a separate trial to ensure the data collection procedure is repeatable. Two testers placed the anatomical markers on the same participant in an alternative order twice. Thereby, the inter-tester reliability and the intra-tester reliability of the two testers were assessed. The absolute mean differences in joint angle and the R2 deduced from the Linear Fit Method were used to evaluate the reliabilities. The inter-rater reliability was assessed by comparing the gait kinematics after the first trial of markers placement of each tester.
The participant performed the 10 m walking test and 10 strides from 3 – 4 records were extracted for the analysis of the reliability of gait kinematics. The 10 m walking test was selected because the reliability of the 3-dimensional gait kinematics has been well studied. For example, the and minimal detectable changes44 and similarity index45 of gait kinematics have been suggested previously. Therefore, the results of our technical validation study could be compared with the results of the existing literature.
The absolute mean differences in lower-limbs joint angles at heel stride, toe-off, maximal flexion and maximal extension were used to assess the repeatability of the data collection procedure.
The minimal detectable changes of gait kinematics reported by Meldrum et.al.44 was used to define the limit of agreement. All absolute mean joint angles differences were smaller than the reported minimal detectable changes (Tables 6–8)44.
The Linear Fit Method proposed by Iosa et.al.45 was used to assess the waveform similarity in gait kinematics. The coefficient of determination R2 that deduced from the Linear Fit Method indicated the goodness of fit. Since there is no consensus on defining the acceptable value of R2, values of the lower boundary of 95% CI of the R2 reported by Iosa et.al.45 were used to guide the interpretation of the R2 in this technical validation study. The R2 for sagittal hip, knee, and ankle kinematics were close to 1 (Table 9) in both inter-rater and intra-rater conditions, and indicated an almost perfect waveform similarity. Besides, all R2 values were greater or equal to the lower boundary of 95% CI of the R2 reported by Iosa et.al.45 (Ankle: 0.86, Knee: 0.96; Hip:0.98).
References
Hicks, G. E., Fritz, J. M., Delitto, A. & Mishock, J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch. Phys. Med. Rehabil. 84, 1858–1864, https://doi.org/10.1016/s0003-9993(03)00365-4 (2003).
Krebs, D. E., Edelstein, J. E. & Fishman, S. Reliability of observational kinematic gait analysis. Phys. Ther. 65, 1027–1033 (1985).
Patterson, T. S., Bishop, M. D., McGuirk, T. E., Sethi, A. & Richards, L. G. Reliability of upper extremity kinematics while performing different tasks in individuals with stroke. J. Motor. Behav. 43, 121–130, https://doi.org/10.1080/00222895.2010.548422 (2011).
Lovern, B. et al. Motion analysis of the glenohumeral joint during activities of daily living. Comput. Methods. Biomech. Biomed. Engin. 13, 803–809, https://doi.org/10.1080/10255841003630637 (2010).
van Andel, C., van Hutten, K., Eversdijk, M., Veeger, D. & Harlaar, J. Recording scapular motion using an acromion marker cluster. Gait Posture 29, 123–128, https://doi.org/10.1016/j.gaitpost.2008.07.012 (2009).
Barrios, J. A. et al. Three-dimensional hip and knee kinematics during walking, running, and single-limb drop landing in females with and without genu valgum. Clin. Biomech. 31, 7–11, https://doi.org/10.1016/j.clinbiomech.2015.10.008 (2016).
Valevicius, A. M. et al. Characterization of normative angular joint kinematics during two functional upper limb tasks. Gait Posture 69, 176–186, https://doi.org/10.1016/j.gaitpost.2019.01.037 (2019).
Gates, D. H., Walters, L. S., Cowley, J., Wilken, J. M. & Resnik, L. Range of motion requirements for upper-limb activities of daily living. Am. J. Occup. Ther. 70, 7001350010p7001350011–7001350010p7001350010, https://doi.org/10.5014/ajot.2016.015487 (2016).
Worsley, P., Stokes, M. & Taylor, M. Predicted knee kinematics and kinetics during functional activities using motion capture and musculoskeletal modelling in healthy older people. Gait Posture 33, 268–273, https://doi.org/10.1016/j.gaitpost.2010.11.018 (2011).
Schwarz, A., Kanzler, C. M., Lambercy, O., Luft, A. R. & Veerbeek, J. M. Systematic review on kinematic assessments of upper limb movements after stroke. Stroke 50, 718–727, https://doi.org/10.1161/STROKEAHA.118.023531 (2019).
Majernik, J. Normative human gait databases. Stat. Res. Lett. 2, 69–74 (2013).
Cortes, J. C. et al. A short and distinct time window for recovery of arm motor control early after stroke revealed with a global measure of trajectory kinematics. Neurorehabil. Neural. Re. 31, 552–560, https://doi.org/10.1177/1545968317697034 (2017).
Valevicius, A. M., Jun, P. Y., Hebert, J. S. & Vette, A. H. Use of optical motion capture for the analysis of normative upper body kinematics during functional upper limb tasks: a systematic review. J. Electromyogr. Kines. 40, 1–15, https://doi.org/10.1016/j.jelekin.2018.02.011 (2018).
Aboelnasr, E. A., Hegazy, F. A. & Altalway, H. A. Kinematic characteristics of reaching in children with hemiplegic cerebral palsy: a comparative study. Brain. Inj. 31, 83–89, https://doi.org/10.1080/02699052.2016.1210230 (2017).
Kontson, K. L. et al. Assessing kinematic variability during performance of Jebsen-Taylor Hand Function Test. J. Hand. Ther., https://doi.org/10.1016/j.jht.2018.10.002 (2019).
Kontson, K., Marcus, I., Myklebust, B. & Civillico, E. Targeted box and blocks test: normative data and comparison to standard tests. Plos One 12, e0177965, https://doi.org/10.1371/journal.pone.0177965 (2017).
Wojtusch, J. & Stryk, O. V. In 2015 IEEE-RAS 15th International Conference on Humanoid Robots (Humanoids). 74–79 (IEEE, 2015).
Ofli, F., Chaudhry, R., Kurillo, G., Vidal, R. & Bajcsy, R. In 2013 IEEE Workshop on Applications of Computer Vision (WACV). 53–60 (IEEE, 2013).
Carnegie Mellon University. CMU Graphics Lab Motion Capture Database, http://mocap.cs.cmu.edu/ (2003).
Mandery, C., Terlemez, Ö., Do, M., Vahrenkamp, N. & Asfour, T. In International Conference on Advanced Robotics (ICAR). 329–336 (IEEE, 2015).
Wang, J. et al. Asians have lower-body mass index (BMI) but higher percent body-fat than do whites: comparisons of anthropometric measurements. Am. J. Clin. Nutr. 60, 23–28, https://doi.org/10.1093/ajcn/60.1.23 (1994).
Huxley, R. et al. Ethnic comparisons of the cross‐sectional relationships between measures of body size with diabetes and hypertension. Obes. Rev. 9, 53–61, https://doi.org/10.1111/j.1467-789x.2007.00439.x (2008).
Rahman, N. I. A., Dawal, S. Z. M., Yusoff, N. & Kamil, N. S. M. Anthropometric measurements among four Asian countries in designing sitting and standing workstations. Sādhanā 43, 10 (2018).
Lin, Y.-C., Wang, M.-J. J. & Wang, E. M. The comparisons of anthropometric characteristics among four peoples in East Asia. Appl. Ergon. 35, 173–178 (2004).
Tan, K. C., Hartono, M. & Kumar, N. Anthropometry of the Singaporean and Indonesian populations. Int. J. Ind. Ergon. 40, 757–766 (2010).
Lee, Y.-C., Chen, C.-H. & Lee, C.-H. Body anthropometric measurements of Singaporean adult and elderly population. Measurement 148, 106949 (2019).
Liang, P. et al. Normative data. DR-NTU (Data), https://doi.org/10.21979/N9/7VF22X (2020).
Ministry of Trade and Industry Singapore - Department of Statistics. Singapore Residents By Age Group, Ethnic Group And Gender, End June, Annual, https://data.gov.sg/dataset/resident-population-by-ethnicity-gender-and-age-group?view_id=8ff89d3f-48c8-46e4-8a4d-a8b9f152976f&resource_id=f9dbfc75-a2dc-42af-9f50-425e4107ae84%20 (2019)
Building and Construction Authority. Code On Accessibility In The Built Environment. (Building and Construction Authority, 2019).
Liang, P. et al. A novel rigid cluster to capture forearm movements. Manuscript submitted for publication. (2019).
Yozbatiran, N., Der Yeghiaian, L. & Cramer, S. A standardized approach to performing the Action Research Arm. Test. Neurorehab. Neural. Re. 22, 78–90, https://doi.org/10.1177/1545968307305353 (2008).
Wolf, S. L., Lecraw, D. E., Barton, L. A. & Jann, B. B. Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients. Exp. Neurol. 104, 125–132, https://doi.org/10.1016/s0014-4886(89)80005-6 (1989).
Nagaraja, V. H., Bergmann, J. H., Andersen, M. S. & Thompson, M. S. In XV International Symposium on 3-D Analysis of Human Movement. 228–230 (University of Salford, 2018).
Podsiadlo, D. & Richardson, S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39, 142–148, https://doi.org/10.1111/j.1532-5415.1991.tb01616.x (1991).
Ng, S. S. & Hui-Chan, C. W. The timed up & go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch. Phys. Med. Rehabil. 86, 1641–1647, https://doi.org/10.1016/j.apmr.2005.01.011 (2005).
Podsiadlo, D. & Richardson, S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39, 142–148 (1991).
Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I. & Maki, B. Measuring balance in the elderly: validation of an instrument. Can. J. Public Health 83, S7–S11 (1992).
Chiu, A. Y., Au-Yeung, S. S. & Lo, S. K. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil. Rehabil. 25, 45–50, https://doi.org/10.1080/dre.25.1.45.50 (2003).
Lu, T., Yen, H. & Chen, H. Comparisons of the inter-joint coordination between leading and trailing limbs when crossing obstacles of different heights. Gait Posture 27, 309–315, https://doi.org/10.1016/j.gaitpost.2007.04.007 (2008).
Jacobs, J. V. A review of stairway falls and stair negotiation: lessons learned and future needs to reduce injury. Gait Posture 49, 159–167, https://doi.org/10.1016/j.gaitpost.2016.06.030 (2016).
van Peppen, R. P., Hendriks, H. J., van Meeteren, N. L., Helders, P. J. & Kwakkel, G. The development of a clinical practice stroke guideline for physiotherapists in The Netherlands: a systematic review of available evidence. Disabil. Rehabil. 29, 767–783, https://doi.org/10.1080/09638280600919764 (2007).
Kwakkel, G. et al. Standardized measurement of sensorimotor recovery in stroke trials: consensus-based core recommendations from the Stroke Recovery and Rehabilitation Roundtable. Int. J. Stroke. 12, 451–461, https://doi.org/10.1177/1747493017711813 (2017).
Roberts, M., Mongeon, D. & Prince, F. Biomechanical parameters for gait analysis: a systematic review of healthy human gait. Phys. Ther. Rehabil. 4, 6, https://doi.org/10.7243/2055-2386-4-6 (2017).
Meldrum, D., Shouldice, C., Conroy, R., Jones, K. & Forward, M. Test–retest reliability of three dimensional gait analysis: including a novel approach to visualising agreement of gait cycle waveforms with Bland and Altman plots. Gait Posture 39, 265–271 (2014).
Iosa, M. et al. Assessment of waveform similarity in clinical gait data: the linear fit method. Biomed. Res. Int. 2014, 214156, https://doi.org/10.1155/2014/214156 (2014).
Acknowledgements
The authors would like to thank the sponsorship of Nanyang Technological University (NTU), Agency for Science, Technology and Research (A*STAR) and National Healthcare Group (NHG).
Author information
Authors and Affiliations
Contributions
Dr. Phyllis Liang contributed to the design of the protocol, provided clinical input, led the team in conducting the project and is the clinical Principal Investigator of the project. Dr. Kwong Wai Hang contributed to the design of the protocol, provided clinical input and led the technical validation of the protocol. Dr. Ananda Sidarta contributed to the design of the protocol and provided technical input. Mr. Yap Choon Kong contributed to the design of the protocol and led the team in data management. Mr. Tan Wee Kiat contributed to the design of the protocol and provided engineering input. Mr Lim Lek Syn contributed to the design of the protocol and provided technical input. Ms. Chan Pui Yee contributed to the design of the protocol and provided clinical input. Mr. Christopher Wee Keong Kuah contributed to the design of the protocol and provided clinical input. Dr. Wee Seng Kwee contributed to the design of the protocol and provided clinical input. Dr. Karen Chua contributed to the design of the protocol and provided clinical input. Dr. Colin Quek contributed to the design of the protocol, provided oversight to the project and is the technical Principal investigator of the project. Prof. Ang Wei Tech conceptualised the vision and direction of the protocol, contributed to the design of the protocol, provided technical input, provided oversight to the project and is the lead Principal Investigator of the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
The Creative Commons Public Domain Dedication waiver http://creativecommons.org/publicdomain/zero/1.0/ applies to the metadata files associated with this article.
About this article
Cite this article
Liang, P., Kwong, W.H., Sidarta, A. et al. An Asian-centric human movement database capturing activities of daily living. Sci Data 7, 290 (2020). https://doi.org/10.1038/s41597-020-00627-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41597-020-00627-7
This article is cited by
-
Sit-to-walk strategy classification in healthy adults using hip and knee joint angles at gait initiation
Scientific Reports (2023)
-
Versatile clinical movement analysis using statistical parametric mapping in MovementRx
Scientific Reports (2023)
-
Database covering the prayer movements which were not available previously
Scientific Data (2023)