Abstract
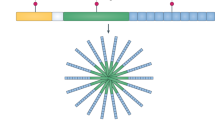
Autoinflammation as a distinct disease category was first reported in 1999 as a group of monogenic disorders characterized by recurrent episodes of systemic and organ-specific inflammation, known as periodic fever syndromes. Since this original description, the focus has shifted considerably to the inclusion of complex multifactorial conditions with an autoinflammatory basis. Furthermore, the boundaries of what are considered to be autoinflammatory disorders are constantly evolving and currently encompass elements of immunodeficiency and autoimmunity. Notable developments in the intervening 20 years include substantial progress in understanding how the different inflammasomes are activated, how infection is sensed by the innate immune system and how intracellular signalling systems are consequently activated and integrated with many different cellular functions in the autoinflammatory process. With these developments, the field of autoinflammation is moving from a gene-centric view of innate immune-mediated disease towards a systems-based concept, which describes how various convergent pathways, including pyrin and the actin cytoskeleton, protein misfolding and cellular stress, NF-κB dysregulation and interferon activation, contribute to the autoinflammatory process. The development and adoption of a systems-based concept of systemic autoinflammatory diseases is anticipated to have implications for the development of treatments that target specific components of the innate immune system.
Key points
-
The definition of autoinflammatory disease has evolved since its original description, with increasing awareness of the influence of various processes in the pathogenesis, including metabolism, cytoskeletal perturbation and infection.
-
The scope of what is considered autoinflammation is widening and now includes not only monogenic periodic fever syndromes but also polygenic conditions and disorders with autoimmune and immunodeficiency components.
-
Gene-centric classifications of disease have often been quite restrictive, and a move towards systems-based classifications would be beneficial in the investigation and management of these disorders.
-
Many autoinflammatory disorders arise, either partly or fully, because of ‘collateral damage’ caused by the innate immune system striving to maintain cellular homeostasis, such as in pyrin-linked cytoskeletal imbalance.
-
Appreciation of the complex overlap between the manifold systems related to autoinflammation, autoimmunity and immunodeficiency can enable the exploration of therapeutic interventions that were not previously considered.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Pathak, S., McDermott, M. F. & Savic, S. Autoinflammatory diseases: update on classification diagnosis and management. J. Clin. Pathol. 70, 1–8 (2017).
Beck, D. & Aksentijevich, I. J. F. Biochemistry of autoinflammatory diseases: catalyzing monogenic disease. Front. Immunol. 10, 101 (2019).
The International FMF Consortium. Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. Cell 90, 797–807 (1997).
French FMF Consortium et al. A candidate gene for familial Mediterranean fever. Nat. Genet. 17, 25–31 (1997).
Masters, S. L. et al. Familial autoinflammation with neutrophilic dermatosis reveals a regulatory mechanism of pyrin activation. Sci. Transl Med. 8, 332–345 (2016).
De Benedetti, F. et al. Canakinumab for the treatment of autoinflammatory recurrent fever syndromes. N. Engl. J. Med. 378, 1908–1919 (2018).
Moghaddas, F. et al. A novel pyrin-associated autoinflammation with neutrophilic dermatosis mutation further defines 14-3-3 binding of pyrin and distinction to familial Mediterranean fever. Ann. Rheum. Dis. 76, 2085–2094 (2017).
McGonagle, D. & McDermott, M. F. A proposed classification of the immunological diseases. PLoS Med. 3, e297 (2006).
Ben-Chetrit, E. et al. Consensus proposal for taxonomy and definition of the autoinflammatory diseases (AIDs): a Delphi study. Ann. Rheum. Dis. 77, 1558–1565 (2018).
McGonagle, D., Watad, A. & Savic, S. J. Novel immunological based classification of rheumatoid arthritis with therapeutic implications. Autoimmun. Rev. 11, 1115–1123 (2018).
Ozen, S. & Bilginer, Y. A clinical guide to autoinflammatory diseases: familial Mediterranean fever and next-of-kin. Nat. Rev. Rheumatol. 10, 135–147 (2014).
Xu, H. et al. Innate immune sensing of bacterial modifications of Rho GTPases by the pyrin inflammasome. Nature 513, 237–241 (2014).
Park, Y. H. et al. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat. Immunol. 17, 914–921 (2016).
Hong, Y. et al. Autoinflammation due to homozygous S208 MEFV mutation. Ann. Rheum. Dis. 78, 571–573 (2019).
Gao, W. et al. Site-specific phosphorylation and microtubule dynamics control pyrin inflammasome activation. Proc. Natl Acad. Sci. USA 113, 4857–4866 (2016).
Van Gorp, H. et al. Familial Mediterranean fever mutations lift the obligatory requirement for microtubules in pyrin inflammasome activation. Proc. Natl Acad. Sci. USA 113, 14384–14389 (2016).
Jamilloux, Y. et al. Familial Mediterranean fever mutations are hypermorphic mutations that specifically decrease the activation threshold of the pyrin inflammasome. Rheumatology 57, 100–111 (2017).
Drenth, J. P. et al. Mutations in the gene encoding mevalonate kinase cause hyper-IgD and periodic fever syndrome. International Hyper-IgD Study Group. Nat. Genet. 22, 178–181 (1999).
Houten, S. M. et al. Mutations in MVK, encoding mevalonate kinase, cause hyperimmunoglobulinaemia D and periodic fever syndrome. Nat. Genet. 22, 175–177 (1999).
Seabra, M. Membrane association and targeting of prenylated Ras-like GTPases. Cell Signal. 10, 167–172 (1998).
Ozen, S. et al. International retrospective chart review of treatment patterns in severe familial Mediterranean fever, tumor necrosis factor receptor-associated periodic syndrome, and mevalonate kinase deficiency/hyperimmunoglobulinemia D syndrome. Arthritis Care Res. 69, 578–586 (2017).
ter Haar, N. M. et al. The phenotype and genotype of mevalonate kinase deficiency: a series of 114 cases from the Eurofever registry. Arthritis Rheum. 68, 2795–2805 (2016).
Lachmann, H. J. Periodic fever syndromes. Best Pract. Res. Clin. Rheumatol. 31, 596–609 (2017).
Waite, A. L. et al. Pyrin modulates the intracellular distribution of PSTPIP1. PLoS One 4, 6147 (2009).
Waite, A. L. et al. Pyrin and ASC co-localize to cellular sites that are rich in polymerizing actin. Exp. Biol. Med. 234, 40–52 (2009).
Manukyan, G. et al. Activated phenotype of circulating neutrophils in familial Mediterranean fever. Immunobiology 218, 892–898 (2013).
Vicente-Manzanares, M. & Sanchez-Madrid, F. Role of the cytoskeleton during leukocyte responses. Nat. Rev. Immunol. 4, 110–122 (2004).
Alghamdi, M. Familial Mediterranean fever, review of the literature. Clin. Rheumatol. 36, 1707–1713 (2017).
Wise, C. A. et al. Mutations in CD2BP1 disrupt binding to PTP PEST and are responsible for PAPA syndrome, an autoinflammatory disorder. Hum. Mol. Genet. 11, 961–969 (2002).
Yeon, H. B. et al. Pyogenic arthritis, pyoderma gangrenosum, and acne syndrome maps to chromosome 15q. Am. J. Hum. Genet. 66, 1443–1448 (2000).
Starnes, T. W. et al. The F-BAR protein PSTPIP1 controls extracellular matrix degradation and filopodia formation in macrophages. Blood 123, 2703–2714 (2014).
Shoham, N. G. et al. Pyrin binds the PSTPIP1/CD2BP1 protein, defining familial Mediterranean fever and PAPA syndrome as disorders in the same pathway. Proc. Natl Acad. Sci. USA 100, 13501–13506 (2003).
Pfajfer, L. et al. Mutations affecting the actin regulator WD repeat-containing protein 1 lead to aberrant lymphoid immunity. J. Allergy Clin. Immunol. 142, 1589–1604 (2018).
Kim, M. L. et al. Aberrant actin depolymerization triggers the pyrin inflammasome and autoinflammatory disease that is dependent on IL-18, not IL-1β. J. Exp. Med. 212, 927–938 (2015).
Volpi, S. et al. A combined immunodeficiency with severe infections, inflammation, and allergy caused by ARPC1B deficiency. J. Allergy Clin. Immunol. 143, 2296–2299 (2019).
Lee, P. P. et al. Wiskott–Aldrich syndrome protein regulates autophagy and inflammasome activity in innate immune cells. Nat. Commun. 8, 1576 (2017).
Poli, M. C. et al. Heterozygous truncating variants in POMP escape nonsense-mediated decay and cause a unique immune dysregulatory syndrome. Am. J. Hum. Genet. 102, 1126–1142 (2018).
Fricke, B. et al. The proteasome maturation protein POMP facilitates major steps of 20S proteasome formation at the endoplasmic reticulum. EMBO Rep. 8, 1170–1175 (2007).
Chakraborty, P. K. et al. Mutations in TRNT1 cause congenital sideroblastic anemia with immunodeficiency, fevers, and developmental delay (SIFD). Blood 124, 2867–2871 (2014).
Wiseman, D. H. et al. A novel syndrome of congenital sideroblastic anemia, B-cell immunodeficiency, periodic fevers, and developmental delay (SIFD). Blood 122, 112–123 (2013).
Giannelou, A. et al. Aberrant tRNA processing causes an autoinflammatory syndrome responsive to TNF inhibitors. Ann. Rheum. Dis. 77, 612–619 (2018).
Dickie, L. J. et al. Involvement of X-box binding protein 1 and reactive oxygen species pathways in the pathogenesis of tumour necrosis factor receptor-associated periodic syndrome. Ann. Rheum. Dis. 71, 2035–2043 (2012).
Scambler, T. et al. ENaC-mediated sodium influx exacerbates NLRP3-dependent inflammation in cystic fibrosis. eLife 8, e49248 (2019).
Agyemang, A. F. et al. Protein misfolding and dysregulated protein homeostasis in autoinflammatory diseases and beyond. Semin. Immunopathol. 37, 335–347 (2015).
Cherubini, M. & Wade-Martins, R. Convergent pathways in Parkinson’s disease. Cell Tissue Res. 373, 79–90 (2018).
Lenart, N., Brough, D. & Denes, A. Inflammasomes link vascular disease with neuroinflammation and brain disorders. J. Cereb. Blood Flow Metab. 36, 1668–1685 (2016).
Sen, R. & Baltimore, D. J. Multiple nuclear factors interact with the immunoglobulin enhancer sequences. Cell 46, 705–716 (1986).
Sen, R. & Baltimore, D. J. C. Inducibility of κ immunoglobulin enhancer-binding protein NF-κB by a posttranslational mechanism. Cell 47, 921–928 (1986).
Mussbacher, M. et al. Cell type-specific roles of NF-κB linking inflammation and thrombosis. Front. Immunol. 10, 85 (2019).
Tak, P. P. & Firestein, G. S. NF-κB: a key role in inflammatory diseases. J. Clin. Invest. 107, 7–11 (2001).
Lawrence, T. The nuclear factor NF-κB pathway in inflammation. Cold Spring Harb. Perspect. Biol. 1, a001651 (2009).
Croston, G. E., Cao, Z. & Goeddel, D. V. NF-κB activation by interleukin-1 (IL-1) requires an IL-1 receptor-associated protein kinase activity. J. Biol. Chem. 270, 16514–16517 (1995).
Rea, I. M. et al. Age and age-related diseases: role of inflammation triggers and cytokines. Front. Immunol. 9, 586 (2018).
Beg, A. A. & Baldwin, A. S. Activation of multiple NF-κB/Rel DNA-binding complexes by tumor necrosis factor. Oncogene 9, 1487–1492 (1994).
Newton, K. & Dixit, V. M. Signaling in innate immunity and inflammation. Cold Spring Harb. Perspect. Biol. 4, 3 (2012).
Kabe, Y. et al. Redox regulation of NF-κB activation: distinct redox regulation between the cytoplasm and the nucleus. Antioxid. Redox Signal. 7, 395–403 (2005).
Devary, Y. et al. NF-κB activation by ultraviolet light not dependent on a nuclear signal. Science 261, 1442–1445 (1993).
Jarosz-Griffiths, H. H. et al. TNF receptor signalling in autoinflammatory diseases. Int. Immunol. 31, 639–648 (2019).
Hayden, M. S. & Ghosh, S. Regulation of NF-κB by TNF family cytokines. Semin. Immunol. 26, 253–266 (2014).
Zonana, J. et al. A novel X-linked disorder of immune deficiency and hypohidrotic ectodermal dysplasia is allelic to incontinentia pigmenti and due to mutations in IKK-gamma (NEMO). Am. J. Hum. Genet. 67, 1555–1562 (2000).
Israel, A. The IKK complex, a central regulator of NF-κB activation. Cold Spring Harb. Perspect. Biol. 2, 1–14 (2010).
Jin, D. Y. & Jeang, K. T. Isolation of full-length cDNA and chromosomal localization of human NF-κB modulator NEMO to Xq28. J. Biomed. Sci. 6, 115–120 (1999).
Kere, J. et al. X-linked anhidrotic (hypohidrotic) ectodermal dysplasia is caused by mutation in a novel transmembrane protein. Nat. Genet. 13, 409–416 (1996).
Courtois, G. et al. A hypermorphic IκBα mutation is associated with autosomal dominant anhidrotic ectodermal dysplasia and T cell immunodeficiency. J. Clin. Invest. 112, 1108–1115 (2003).
Orange, J. S. & Geha, R. S. Finding NEMO: genetic disorders of NF-κB activation. J. Clin. Invest. 112, 983–985 (2003).
Nenci, A. et al. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature 446, 557–561 (2007).
Vlantis, K. et al. NEMO prevents RIP kinase 1-mediated epithelial cell death and chronic intestinal inflammation by NF-κB-dependent and -independent functions. Immunity 44, 553–567 (2016).
Zaph, C. et al. Epithelial-cell-intrinsic IKK-β expression regulates intestinal immune homeostasis. Nature 446, 552–556 (2007).
Cuchet-Lourenco, D. et al. Biallelic RIPK1 mutations in humans cause severe immunodeficiency, arthritis, and intestinal inflammation. Science 361, 810–813 (2018).
Tao, P. et al. A dominant autoinflammatory disease caused by non-cleavable variants of RIPK1. Nature 577, 109–114 (2020).
Lalaoui, N. et al. Mutations that prevent caspase cleavage of RIPK1 cause autoinflammatory disease. Nature 577, 103–108 (2020).
Boisson, B. et al. Immunodeficiency, autoinflammation and amylopectinosis in humans with inherited HOIL-1 and LUBAC deficiency. Nat. Immunol. 13, 1178–1186 (2012).
Ikeda, F. et al. SHARPIN forms a linear ubiquitin ligase complex regulating NF-κB activity and apoptosis. Nature 471, 637–641 (2011).
Aksentijevich, I. & Zhou, Q. NF-κB pathway in autoinflammatory diseases: dysregulation of protein modifications by ubiquitin defines a new category of autoinflammatory diseases. Front. Immunol. 8, 399 (2017).
Zhou, Q. et al. Biallelic hypomorphic mutations in a linear deubiquitinase define otulipenia, an early-onset autoinflammatory disease. Proc. Natl Acad. Sci. USA 113, 10127–10132 (2016).
Damgaard, R. B. et al. OTULIN deficiency in ORAS causes cell type-specific LUBAC degradation, dysregulated TNF signalling and cell death. EMBO Mol. Med. 11, 3 (2019).
Aksentijevich, I. & McDermott, M. F. Lessons from characterization and treatment of the autoinflammatory syndromes. Curr. Opin. Rheumatol. 29, 187–194 (2017).
Zhou, Q. et al. Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat. Genet. 48, 67–73 (2016).
Shembade, N. & Harhaj, E. W. Regulation of NF-κB signaling by the A20 deubiquitinase. Cell. Mol. Immunol. 9, 123–130 (2012).
Wu, Y. et al. Ubiquitination regulation of inflammatory responses through NF-κB pathway. Am. J. Transl Res. 10, 881–891 (2018).
Aeschlimann, F. A. et al. A20 haploinsufficiency (HA20): clinical phenotypes and disease course of patients with a newly recognised NF-κB-mediated autoinflammatory disease. Ann. Rheum. Dis. 77, 728–735 (2018).
Lawless, D. et al. A case of adult-onset Still’s disease caused by a novel splicing mutation in TNFAIP3 successfully treated with tocilizumab. Front. Immunol. 9, 1527 (2018).
Badran, Y. R. et al. Human RELA haploinsufficiency results in autosomal-dominant chronic mucocutaneous ulceration. J. Exp. Med. 214, 1937–1947 (2017).
Faruqi, A. J. et al. RELA/p65 haploinsufficiency as a novel cause of primary immune disorder. J. Immunol. 198, 59.17 (2017).
Liu, T. et al. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2, 17023 (2017).
Kaustio, M. et al. Damaging heterozygous mutations in NFKB1 lead to diverse immunologic phenotypes. J. Allergy Clin. Immunol. 140, 782–796 (2017).
Alnemri, E. S. Sensing cytoplasmic danger signals by the inflammasome. J. Clin. Immunol. 30, 512–519 (2010).
Uggenti, C., Lepelley, A. & Crow, Y. J. Self-awareness: nucleic acid-driven inflammation and the type I interferonopathies. Ann. Rev. Immunol. 37, 247–267 (2019).
Sanchez, G. A. M. et al. JAK1/2 inhibition with baricitinib in the treatment of autoinflammatory interferonopathies. J. Clin. Invest. 128, 3041–3052 (2018).
Briand, C. et al. Efficacy of JAK1/2 inhibition in the treatment of chilblain lupus due to TREX1 deficiency. Ann. Rheum. Dis. 78, 431–433 (2019).
McLellan, K. E. et al. JAK 1/2 blockade in MDA5 gain-of-function. J. Clin. Immunol. 38, 844–846 (2018).
Banchereau, R. et al. Personalized immunomonitoring uncovers molecular networks that stratify lupus patients. Cell 165, 1548–1550 (2016).
Baechler, E. C. et al. Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc. Natl Acad. Sci. USA 100, 2610–2615 (2003).
Hjelmervik, T. O. R. et al. Gene expression profiling of minor salivary glands clearly distinguishes primary Sjögren’s syndrome patients from healthy control subjects. Arthritis Rheum. 52, 1534–1544 (2005).
Higgs, B. W. et al. Patients with systemic lupus erythematosus, myositis, rheumatoid arthritis and scleroderma share activation of a common type I interferon pathway. Ann. Rheum. Dis. 70, 2029–2036 (2011).
van der Pouw Kraan, T. C. et al. Rheumatoid arthritis subtypes identified by genomic profiling of peripheral blood cells: assignment of a type I interferon signature in a subpopulation of patients. Ann. Rheum. Dis. 66, 1008–1014 (2007).
Rigolet, M. et al. Distinct interferon signatures stratify inflammatory and dysimmune myopathies. Rheum. Musculoskelet. Dis. 5, e000811 (2019).
Li, T. & Chen, Z. J. The cGAS–cGAMP–STING pathway connects DNA damage to inflammation, senescence, and cancer. J. Exp. Med. 215, 1287–1299 (2018).
Liu, Y. et al. Activated STING in a vascular and pulmonary syndrome. N. Engl. J. Med. 371, 507–518 (2014).
Ablasser, A. & Chen, Z. J. cGAS in action: expanding roles in immunity and inflammation. Science 363, eaat8657 (2019).
Luksch, H. et al. STING-associated lung disease in mice relies on T cells but not type I interferon. J. Allergy Clin. Immunol. 144, 254–266 (2019).
Warner, J. D. et al. STING-associated vasculopathy develops independently of IRF3 in mice. J. Exp. Med. 214, 3279–3292 (2017).
Sivick, K. E. et al. Magnitude of therapeutic STING activation determines CD8+ T cell-mediated anti-tumor immunity. Cell Rep. 25, 3074–3085 (2018).
Cerboni, S. et al. Intrinsic antiproliferative activity of the innate sensor STING in T lymphocytes. J. Exp. Med. 214, 1769–1785 (2017).
Srikanth, S. et al. The Ca2+ sensor STIM1 regulates the type I interferon response by retaining the signaling adaptor STING at the endoplasmic reticulum. Nat. Immunol. 20, 152–162 (2019).
Rice, L. et al. A report of novel STIM1 deficiency and 6 year follow up of two previous cases associated with mild immunological phenotype. J. Clin. Immunol. 3, 249–256 (2018).
Feske, S., Picard, C. & Fischer, A. Immunodeficiency due to mutations in ORAI1 and STIM1. Clin. Immunol. 135, 169–182 (2010).
Jeremiah, N. et al. Inherited STING-activating mutation underlies a familial inflammatory syndrome with lupus-like manifestations. J. Clin. Invest. 124, 5516–5520 (2014).
Konno, H. et al. Pro-inflammation associated with a gain-of-function mutation (R284S) in the innate immune sensor STING. Cell Rep. 23, 1112–1123 (2018).
Saldanha, R. G. et al. A mutation outside the dimerization domain causing atypical STING-associated vasculopathy with onset in infancy. Front. Immunol. 9, 1535 (2018).
Arakelyan, A. et al. Autoimmunity and autoinflammation: a systems view on signaling pathway dysregulation profiles. PLoS One 12, 1–21 (2017).
Grateau, G. et al. How should we approach classification of autoinflammatory diseases? Nat. Rev. Rheumatol. 9, 624–629 (2013).
Savic, S. & McDermott, M. F. Clinical genetics in 2014: new monogenic diseases span the immunological disease continuum. Nat. Rev. Rheumatol. 11, 67–68 (2015).
Savic, S., Dickie, L. J., Wittmann, M. & McDermott, M. F. Autoinflammatory syndromes and cellular responses to stress: pathophysiology, diagnosis and new treatment perspectives. Best Pract. Res. Clin. Rheumatol. 26, 505–533 (2012).
Donath, M. Y. & Shoelson, S. E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 11, 98–107 (2011).
Dennis, G. Jr et al. Synovial phenotypes in rheumatoid arthritis correlate with response to biologic therapeutics. Arthritis Res. Ther. 16, R90 (2014).
Liston, A. & Masters, S. L. Homeostasis-altering molecular processes as mechanisms of inflammasome activation. Nat. Rev. Immunol. 17, 208–214 (2017).
Yan, M. H., Wang, X. & Zhu, X. Mitochondrial defects and oxidative stress in Alzheimer disease and Parkinson disease. Free Radic. Biol. Med. 62, 90–101 (2013).
Mills, E. L. et al. Itaconate is an anti-inflammatory metabolite that activates Nrf2 via alkylation of KEAP1. Nature 556, 113–117 (2018).
O’Neill, L. & Artyomov, M. N. Itaconate: the poster child of metabolic reprogramming in macrophage function. Nat. Rev. Immunol. 19, 273–281 (2019).
Lara-Reyna, S. et al. Metabolic reprogramming of cystic fibrosis macrophages via the IRE1a arm of the unfolded protein response results in exacerbated inflammation. Front. Immunol. 10, 1789 (2019).
Lukens, J. R. et al. Dietary modulation of the microbiome affects autoinflammatory disease. Nature 516, 246–249 (2014).
Fishman, J. & Thomson, A. Clinical implications of basic science discoveries: immune homeostasis and the microbiome—dietary and therapeutic modulation and implications for transplantation. Am. J. Transplant. 15, 1755–1758 (2015).
McDermott, M. F. et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell 97, 133–144 (1999).
McDermott, M. F. & Aksentijevich, I. The autoinflammatory syndromes. Curr. Opin. Allergy Clin. Immunol. 2, 511–516 (2002).
Sarrauste de Menthière, C. et al. INFEVERS: the registry for FMF and hereditary inflammatory disorders mutations. Nucleic Acids Res. 31, 282–285 (2003).
Tang, D. et al. PAMPs and DAMPs: signal 0s that spur autophagy and immunity. Immunol. Rev. 249, 158–175 (2012).
Takeuchi, O. & Akira, S. J. C. Pattern recognition receptors and inflammation. Cell 140, 805–820 (2010).
Martinon, F. et al. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-β. Mol. Cell 10, 417–426 (2002).
Lamkanfi, M. & Dixit, V. M. Inflammasomes and their roles in health and disease. Annu. Rev. Cell Dev. Biol. 28, 137–161 (2012).
Strowig, T. et al. Inflammasomes in health and disease. Nature 481, 278–286 (2012).
Vanaja, S. K. et al. Mechanisms of inflammasome activation: recent advances and novel insights. Trends Cell Biol. 25, 308–315 (2015).
Sutterwala, F. S. et al. Mechanism of NLRP3 inflammasome activation. Ann. N. Y. Acad. Sci. 1319, 82–95 (2014).
Mangan, M. S. et al. Targeting the NLRP3 inflammasome in inflammatory diseases. Nat. Rev. Drug Discov. 17, 588–606 (2018).
Nakamura, S. et al. Identification of baseline gene expression signatures predicting therapeutic responses to three biologic agents in rheumatoid arthritis: a retrospective observational study. Arthritis Res. Ther. 18, 159 (2016).
Tasaki, S. et al. Multi-omics monitoring of drug response in rheumatoid arthritis in pursuit of molecular remission. Nat. Commun. 9, 2755 (2018).
Konttinen, Y. et al. Osteoarthritis as an autoinflammatory disease caused by chondrocyte-mediated inflammatory responses. Arthritis Rheum. 64, 613–616 (2012).
Berenbaum, F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr. Cartil. 21, 16–21 (2013).
Gilbert, S. J. & Blain, E. J. in Mechanobiology in Health and Disease (ed. Verbruggen, S.) 99–126 (Elsevier, 2018).
Kalaitzoglou, E. et al. Innate immune responses and osteoarthritis. Curr. Rheumatol. Rep. 19, 45 (2017).
Nefla, M. et al. The danger from within: alarmins in arthritis. Nat. Rev. Rheumatol. 12, 669–683 (2016).
Geyer, M. & Schönfeld, C. Novel insights into the pathogenesis of osteoarthritis. Curr. Rheumatol. Rev. 14, 98–107 (2018).
Rigante, D., Vitale, A., Lucherini, O. M. & Cantarini, L. The hereditary autoinflammatory disorders uncovered. Autoimmun. Rev. 13, 892–900 (2014).
Berteau, F. et al. Autosomic dominant familial Behçet disease and haploinsufficiency A20: a review of the literature. Autoimmun. Rev. 17, 809–815 (2018).
Cowen, E. W. & Goldbach-Mansky, R. DIRA, DITRA, and new insights into pathways of skin inflammation: what’s in a name? Arch. Dermatol. 148, 381–384 (2012).
Rossi-Semerano, L. et al. First clinical description of an infant with interleukin-36-receptor antagonist deficiency successfully treated with anakinra. Pediatrics 132, 1043–1047 (2013).
Acknowledgements
The authors are supported by the EU Horizon 2020 research and innovation programme (ImmunAID; grant agreement number 779295). The authors thank T. Scambler, F. Berenbaum and S. Lara-Reyna for critical reading of the manuscript.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
S.S. declares that he has received a travel grant and honoraria from SOBI and Novartis. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Rheumatology thanks I. Touitou, M. Gattorno, T. Vogel and S. Masters for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Pattern recognition receptor
-
A protein that recognizes conserved molecular structures either found in pathogens, such as bacteria and viruses (pathogen-associated molecular patterns), or released by damaged cells (damage-associated molecular patterns).
- Filamentous actin
-
(F-actin). Actin is the most abundant protein in eukaryotic cells and can be present in either a linear polymeric form or as filamentous actin.
- Autophagy
-
A highly regulated process of ‘self-eating’ whereby cell organelles and their contents can be repurposed for other uses.
- Hypomorphic mutations
-
Types of mutation that cause a partial loss of gene function or in which the wild-type gene product is expressed at a reduced level.
- Anhidrotic ectodermal dysplasia
-
A form of ectodermal dysplasia characterized by abnormal development of ectodermal tissues including the skin, hair, teeth and sweat glands, resulting in an inability to sweat (anhidrosis).
- Stop-gain variant
-
A mutation resulting in a premature termination codon (that is, a stop was gained), which signals the end of translation and results in a shortened protein product.
- Itaconate
-
A derivate of the tricarboxylic acid cycle, which has a key role in the regulation of macrophage function; it has been shown to decrease production of pro-inflammatory mediators in lipopolysaccharide-treated macrophages and to ameliorate sepsis and psoriasis in animal models, revealing a novel biological action beyond its regular roles in antimicrobial defences.
Rights and permissions
About this article
Cite this article
Savic, S., Caseley, E.A. & McDermott, M.F. Moving towards a systems-based classification of innate immune-mediated diseases. Nat Rev Rheumatol 16, 222–237 (2020). https://doi.org/10.1038/s41584-020-0377-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-020-0377-5
This article is cited by
-
Caudal DMN neurons innervate the spleen and release CART peptide to regulate neuroimmune function
Journal of Neuroinflammation (2023)
-
Inflammation across tissues: can shared cell biology help design smarter trials?
Nature Reviews Rheumatology (2023)
-
The caspase-1 inhibitor VX765 upregulates connexin 43 expression and improves cell–cell communication after myocardial infarction via suppressing the IL-1β/p38 MAPK pathway
Acta Pharmacologica Sinica (2022)
-
Disorders of ubiquitylation: unchained inflammation
Nature Reviews Rheumatology (2022)
-
Autoinflammatorische Erkrankungen – ein expandierendes Spektrum
Monatsschrift Kinderheilkunde (2022)