Abstract
The health benefits of exercise are well-recognized and are observed across multiple organ systems. These beneficial effects enhance overall resilience, healthspan and longevity. The molecular mechanisms that underlie the beneficial effects of exercise, however, remain poorly understood. Since the discovery in 2000 that muscle contraction releases IL-6, the number of exercise-associated signalling molecules that have been identified has multiplied. Exerkines are defined as signalling moieties released in response to acute and/or chronic exercise, which exert their effects through endocrine, paracrine and/or autocrine pathways. A multitude of organs, cells and tissues release these factors, including skeletal muscle (myokines), the heart (cardiokines), liver (hepatokines), white adipose tissue (adipokines), brown adipose tissue (baptokines) and neurons (neurokines). Exerkines have potential roles in improving cardiovascular, metabolic, immune and neurological health. As such, exerkines have potential for the treatment of cardiovascular disease, type 2 diabetes mellitus and obesity, and possibly in the facilitation of healthy ageing. This Review summarizes the importance and current state of exerkine research, prevailing challenges and future directions.
Key points
-
Although the benefits of exercise in enhancing health and treating disease are well-acknowledged, the molecular mechanisms underlying exercise-associated benefits remain ill-defined and are actively being investigated.
-
‘Exerkines’ encompass a broad variety of signalling moieties released in response to acute and/or chronic exercise that exert their effects through endocrine, paracrine and/or autocrine pathways.
-
Exerkines can come in many forms, such as hormones, metabolites, proteins and nucleic acids; interest is increasing in moving beyond singular changes of specific factors to profiling exerkine alterations using ‘omics’ platforms.
-
There is burgeoning interest in the role of extracellular vesicles, which are membranous structures released from cells, in serving as important carriers of molecular signals and drivers of inter-organ crosstalk related to exercise.
-
Multiple organ systems, including the cardiometabolic system, nervous system and immune system, produce exerkines and are influenced by exerkines, which probably contributes to the pleiotropic and variable response to exercise.
-
Emerging research on exerkines suggests multiple promising avenues for translational research and therapeutic modulation to capture exercise-associated benefits; enhanced rigour in experimental design will facilitate comparison between studies.
Similar content being viewed by others
Introduction
Irrefutable evidence supports the importance of physical activity, exercise and cardiorespiratory fitness in the prevention and treatment of chronic diseases, such as cardiovascular disease, obesity, type 2 diabetes mellitus, cognitive decline and many cancers, while enhancing the immune system, healthspan, longevity and resilience1 (Fig. 1). Conversely, physical inactivity poses a major public health threat, as it is associated with increased mortality2 and a notable economic burden3. Moreover, the COVID-19 pandemic clearly reinforces the relevance of physical activity for health, due to the effects of COVID-19-related reductions in physical activity4 and increases in sedentary behaviour, especially due to COVID-19-related quarantine4. Moreover, physical inactivity is associated with increased risk of severe COVID-19 outcomes5.
a | Organs and tissues that can serve as source of exerkines and that are directly affected by exercise. b | Exercise results in profound health benefits, including reductions in the presence or severity of certain diseases, as well as increases in healthspan, longevity and resilience. T2DM, type 2 diabetes mellitus.
Although the terms ‘exercise’ and ‘physical activity’ are commonly used interchangeably, exercise is typically regarded as intentional physical activity, such as aerobic training1, resistance training1 or high-intensity interval training6,7. By contrast, physical activity encompasses exercise as well as usual occupational and/or domestic activity1. Promoting physical activity remains a critical intervention to reduce the incidence and prevalence of common metabolic diseases. In the USA, official guidelines for physical activity were first published in 1995 and recommended that every US adult should accumulate at least 30 min of moderate intensity physical activity on most, preferably all, days of the week8. Subsequently, these guidelines have evolved1. In 2020, the World Health Organization stated that that all adults should aim for 150–300 min of moderate intensity physical activity per week or 75–150 min of vigorous intensity physical activity per week or an equivalent combination of moderate intensity and vigorous intensity physical activity per week9. Despite these recommendations, objective data obtained with accelerometers of physical activity in the US population indicated poor adherence to recommended guidelines, with only 5% of US adults having more than 30 min of moderate intensity physical activity per day10.
In this Review, we focus on the potential role of exerkines in driving the established benefits of exercise, such as preventing and mitigating disease, promoting health and increasing resilience. The term exerkine was coined in 2016 (ref.11), although the concept of humoral factors mediating the benefit of exercise has long been recognized. A prime example is lactic acid; its secretion from skeletal muscle was identified over 100 years ago12. In 1961, Goldstein speculated about the existence of a non-insulin humoral factor that regulates the effect of exercise on skeletal muscle and liver glucose utilization13. For the purposes of this Review, we define an exerkine as a signalling moiety released in response to acute exercise and/or chronic exercise, exerting its effects through endocrine, paracrine and/or autocrine pathways.
As skeletal muscle comprises approximately one third of body mass and has an important role in exercise14, the effects of physical activity (Fig. 1) were initially attributed to blood-borne factors, particularly muscle-secreted hormones (myokines)15. Of the myokines, IL-6 has been the most extensively studied since its discovery in 2000 (ref.16). Subsequent exerkine work has broadened to include exercise-related humoral factors arising from the heart (cardiokines), liver (hepatokines), white adipose tissue (WAT; adipokines) and brown adipose tissue (BAT; batokines) and the nervous system (neurokines), with local autocrine effects (affecting the cell of origin) and paracrine effects (affecting adjacent cells) (Table 1). Exerkines are increasingly recognized to include a broad range of signalling moieties, including cytokines, nucleic acids (microRNA17, mRNA and mitochondrial DNA), lipids and metabolites, which are frequently driven by cell-specific extracellular vesicle secretion18.
Understanding the role of exerkines in the physiological and biological response to exercise is a principal objective of many investigations sponsored by the National Institutes of Health (NIH)19, given the demonstrated benefits of exercise in enhancing and prolonging human health across the lifespan. In 2020, the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases convened a virtual 2-day public workshop inviting 21 international experts to discuss “Exerkines in Health, Resilience, and Diseases”. The workshop executive summary was published online20, laying the foundation for this article. In this Review, we summarize the importance and current state of exerkine research, the prevailing challenges and future directions.
Exercise response variability
Potential role for exerkines
The majority of exercise research has been limited to studies with genetically homogeneous animal models and/or small numbers of human participants. Moreover, the physiological response to a structured exercise training stimulus remains highly variable in humans and animals owing to a multitude of external and internal factors. In terms of external factors, the context of exercise matters, as exercise timing relative to circadian rhythms21, fed–fasting status22 or post-exercise dietary composition23 might influence metabolic outcomes. This variability is well-detailed in a study published in 2022, which included an atlas describing the time-dependent effects of exercise across multiple tissues after a single bout of treadmill exercise24. Addressing these external factors will require careful consideration of the exercise exposure, controlling the exercise exposure’s environmental context and serial sampling of blood and tissue prior, during and after exercise. This level of rigor is needed to ‘reduce the noise’ and facilitate interpretation of the temporal signatures of circulating and tissue-specific exerkines. In terms of internal factors, genetics have a critical role in the response to exercise. The Health, Risk Factors, Exercise Training and Genetics (HERITAGE) family study involved 20 weeks of supervised aerobic exercise training in 481 sedentary, healthy, white adults from 98 two-generation families, and found that the maximal heritability estimate for the aerobic capacity response was roughly 47%25. Furthermore, chronic exercise training elicited a ‘non-response’ in terms of improved aerobic capacity in ~20% of individuals25. In addition, 7–15% of individuals demonstrated an ‘adverse response’ regarding alterations in systolic blood pressure, as well as in fasting levels of HDL cholesterol, triglycerides and insulin25,26.
To drive the application of precision medicine to exercise, investigations into the mechanisms underlying the response variability to exercise are sorely needed. The contribution of exerkines to the variation in exercise response remains under active research and will be a key focus of the Molecular Transducers of Physical Activity Consortium (MoTrPAC; NCT03960827). This NIH-supported research consortium is designed to discover and broadly characterize the range of molecular transducers that underlie the variable effects of exercise in humans and animals. For humans, MoTrPAC has several unique features: its size (2,280 estimated participants); its recruitment of sedentary participants who will undergo a 12-week programme of aerobic exercise, resistance exercise or no exercise (control), with a comparison group of highly active endurance exercise or resistance exercise participants; and its time course analysis of changes in tissue (muscle and adipose tissue) and plasma metabolites19. In animals (~800 studied), the unique feature of MoTrPAC will be its focus on detailed biospecimen analysis across multiple time points and organs, which cannot be easily replicated in humans, in young (6 months) and old (18 months) male and female rats after an acute (single session) bout of treadmill exercise, or after chronic treadmill exercise (8 weeks) versus non-exercised control rats19. Identification of an exerkine or a panel of exerkines, which capture the benefits of exercise, would have potential implications for improving the health of those unable to exercise, such as those with ageing-associated exercise intolerance.
Influence of exercise exposure
Exerkines are secreted in response to acute exercise, which is usually a single episode of either aerobic or resistance exercise. Chronic exercise is also associated with altered humoral factors, even in the resting state, suggesting that exerkine alterations can reflect the effects of chronic training27.
The acute exerkine response is influenced by the type of exercise, duration of exercise, underlying fitness, fed–fasting status and sample timing after exercise. In a human model, the blood concentration of glucose typically remains stable during acute exercise, with the liver releasing glucose for brain and skeletal muscle usage28. During exercise, skeletal muscle also uses lipid as fuel, which originates from the triglycerides stored in muscle and free fatty acids (FFAs) released from WAT29. The classic exerkines released during acute exercise, as found in human and animal models, include IL-6, IL-8, IL-1 receptor antagonist (IL-1RA) and IL-10. In a study in humans in which blood samples were collected before and after a marathon, plasma levels of several cytokines (IL-6, IL-1RA, IL-10 and tumour necrosis factor (TNF)) were higher than baseline levels when collected immediately after exercise, peaking 1–2 h after exercise and remaining elevated for ~4 h after exercise30. Certainly, the type and intensity of exercise matters. As an example, the exerkine response to high-intensity interval training depends on exercise intensity; higher exercise intensity corresponds with higher plasma levels of IL-6, while IL-10 levels remain unchanged compared with the levels before exercise6. Supplementary Table 1 shows examples of singular exerkine alterations. Currently, exerkine research is evolving from measuring singular exerkine changes to characterizing metabolic profiles31, for which challenges in analysis and interpretation remain (Table 2).
Notably, the acute exerkine response does not necessarily parallel the chronic exerkine response (Supplementary Table 1). Typically, acute exercise exposure is associated with responses focused on the maintenance of metabolic homeostasis, with acute inflammation balanced by anti-inflammatory mediators30 and accommodating shifts in fuel utilization. By contrast, chronic exercise exposure is associated with responses focused on long-term metabolic adaptations and decreased inflammation27. However, when investigating chronic exercise exposure, the caveats of recent (24–72 hours prior to exercise) acute exercise or dietary composition, underlying fitness, fed–fasting status, circadian timing and training modality need to be considered. Moreover, the effects of exercise could also be influenced by alterations at the level of the exerkine receptor, in addition to alterations in plasma levels of exerkines. For example, in humans, chronic exercise training reduces plasma concentrations of IL-6; however, this effect could be partially mitigated by increased skeletal muscle mRNA expression of IL-6 receptor32.
Exerkines: technical considerations
Discovery techniques
Exerkine research is increasingly focused on measuring changes across a broad swathe of factors rather than singular change. Specifically, interest is increasing in ‘omics’ technology to capture exercise-related changes in lipids (lipidomics), metabolites (metabolomics), proteins (proteomics), gene expression (transcriptomics) and DNA alterations (epigenomics)31 (Table 2). A paper in 2020 studied humans across the spectrum of insulin sensitivity (n = 36, ranging from people with high insulin sensitivity to patients with diabetes mellitus) who performed an acute bout of treadmill-based exercise to reach peak oxygen uptake. This exercise exposure altered >50% of measured molecules, spanning platforms based on lipidomics, metabolomics, proteomics, transcriptomics and epigenomics31. Table 2 lists commonly used platforms for exerkine analysis, including their relative advantages and disadvantages. Mass spectrometry is often used for targeted and untargeted omics analysis, whereas immunoassays are commonly used for analysis of proteins and metabolites. Genetic analyses include RNA sequencing, methylation sequencing (Methyl-seq) and assay for transposase-accessible chromatin with high-throughput sequencing (ATAC-seq)33. Together, these platforms provide a rich profile of the molecular and epigenomic changes that occur in response to acute and chronic exercise.
Extracellular vesicles
In the exerkine field, interest is also intensifying in the role of extracellular vesicles as important carriers of molecular signals and drivers of inter-organ crosstalk related to exercise18. Extracellular vesicles are membranous structures that are released from almost all cell types, with cell-specific profiles. They vary in size, ranging from 150 nm to 1,000 nm, and carry an assortment of material, including proteins, nucleic acids and lipids18,34. The content of extracellular vesicles reflects the unique and varied composition of the cells from which they are released. As an example of extracellular vesicles acting as an exerkine in humans, acute exercise increases plasma levels of various microRNAs after exercise, and chronic exercise increases various microRNAs in the resting state17, supporting the possibility of microRNAs exerting their endocrine effects via extracellular vesicle-based transport11,34.
Extracellular vesicles can be routinely isolated and profiled from cell culture media. Studying the molecular cargo of plasma-derived extracellular vesicles, however, remains uniquely challenging. Critical to extracellular vesicle analysis is the careful consideration of pre-analytical steps, including proper collection and isolation. Isolation techniques include ultracentrifugation (using a differential density gradient), ultrafiltration, size exclusion chromatography, high-resolution mass spectrometry, capillary electrophoresis, asymmetric-flow field-flow fractionation and immunoaffinity capture35. Moreover, contamination at the time of collection needs to be considered as extracellular vesicles can arise from ex vivo platelet activation36,37. A 2021 paper presented an optimized size-exclusion chromatography method for proteomic analysis of plasma-derived extracellular vesicles from platelet-poor plasma; this technique has greater precision than conventional extracellular vesicle techniques and demonstrates a distinct exosome protein cargo profile after acute exercise in humans37.
Autocrine, paracrine and/or endocrine effects
Initially, exerkine research focused on changes in plasma levels of cytokines, especially before and after an acute exercise exposure30. The classic exerkines are cytokines, of which IL-6 has been the most extensively studied since its identification as a myokine in 2000 (ref.16). Subsequently, the field evolved into examining the endocrine effects of exerkines, where molecules secreted from the source tissue, traditionally viewed as skeletal muscle, affect distant tissues15. Especially within the past 15 years, interest has been increasing in the local effects of exerkines, either on the secreting tissue (autocrine) or the adjacent environment (paracrine)38 (Table 1), non-muscle exerkine sources39 (Supplementary Table 1) and exerkine profiling rather than on singular exerkine alterations31 (Table 2).
A common perception among the general scientific community is the view of exerkines as a cytokine exerting its effects in an endocrine fashion, affecting tissues distant from the originating tissue. Exerkines are not merely cytokines, however, as hormones, neurotransmitters or metabolites associated with exercise, such as catecholamines40, lactate41 or FFAs29, can also serve as exerkines with endocrine signalling potential42.
From an autocrine standpoint, exerkines affect their origin cells by coupling local energy balance to tissue growth and metabolic homeostasis (Table 1). For example, in skeletal muscle, myocytes secrete factors such as lactate41, musclin43 and myostatin44 that couple exercise to changes in mitochondrial biogenesis and myocyte substrate utilization.
Muscle and other highly metabolically active tissues can also secrete exerkines that exert local (paracrine) effects38. For example, muscle secretes vascular endothelial growth factor (VEGF)45,46, angiopoietin 1 (ref.47) and IL-8 (ref.48) to regulate tissue angiogenesis, modulate blood flow and increase nutrient availability to support tissue growth27,49,50,51,52 (Table 1). Exercise-related paracrine effects are also observed in the nervous system53, adipose tissue42,54,55,56,57,58, bone59,60,61, cartilage62, extracellular matrix63,64 and the immune system65,66.
Tissue-specific exerkine relationships
The cardiovascular system
Physical activity reduces the risk of cardiometabolic disease and mortality. Although exercise mitigates traditional cardiovascular risk factors, such as obesity and dyslipidaemia, these benefits incompletely account for the effects of exercise on cardiometabolic health. Studies in both humans and animal models support a role for exerkines potentially enhancing cardiometabolic health (Fig. 2; Table 3; Supplementary Table 1). Exerkines could also oppose multiple mechanisms associated with cardiovascular disease, such as persistent systemic inflammation, dysregulated energy balance and fuel utilization. Furthermore, the enhanced angiogenesis associated with certain exerkines could mitigate ischaemia. Notably, exercise might improve endothelial function. As the vascular endothelium lies at the interface between blood and tissue, its wide-ranging distribution and strategic positioning supports its potential role as an initiator and recipient of exerkine-related effects. For example, interplay between the endothelium and established exerkines, such as nitric oxide52 and VEGF27, has been shown to influence vascular tone, inflammation, regeneration and thrombosis, and has an important role in cardiovascular and overall resilience67.
Exerkines released after exercise into the systemic circulation (see Table 3 for tissue sources, detailed effects and relevant references), including proteins (blue lines), metabolites (yellow circles) and extracellular vesicles (green circles), affect the cardiometabolic system. The effects are wide-ranging and systemic. In the cardiovascular system, exerkines enhance vascularization and angiogenesis, as well as improve blood pressure, endothelial function and overall fitness, resulting in cardioprotection. In adipose tissue, exerkines increase fatty acid uptake, enhancing lipolysis, thermogenesis and glucose metabolism. In the liver, exerkines enhance glucose metabolism and fatty acid uptake. In skeletal muscle, exerkines enhance muscle formation, maintenance and repair, glucose uptake, lipid oxidation, mitochondrial biogenesis and muscle capillarization. In the pancreas, exerkines enhance cell viability and influence insulin secretion. Commonly described exerkines are noted. 12,13-diHOME, 12,13-dihydroxy-9Z-octadecenoic acid; BAIBA, β-aminoisobutyric acid; FGF21, fibroblast growth factor 21; GDF15, growth and differentiation factor 15; HSP72, heat shock protein 72; METRNL, meteorin-like; SDC4, syndecan 4; SPARC, secreted protein acidic and cysteine rich; TGFβ2, transforming growth factor-β2; VEGF, vascular endothelial growth factor.
Contracting skeletal muscle produces many molecules that can enhance the cardiovascular system. Studies in humans15,45,68,69,70,71,72,73,74 and animal models15,43,49,75,76 have shown that the exerkines angiopoietin 1 (refs49,68,69), fractalkine70,71, fibroblast growth factor 21 (FGF21)72,73, IL-6 (ref.15), IL-8 (refs50,74), musclin43, myonectin75 and VEGF27,45,76 are generally increased with acute exercise; however, the exerkine response to chronic training, as measured by assessing exerkines in plasma during the resting state, can be quite variable and discrepant from the acute effects. As shown in Table 3 and Supplementary Table 1, examples include angiopoietin68,69, FGF21 (refs73,77), fractalkine70, IL-6 (refs30,78) and IL-8 (refs50,74).
Adipose tissue
Exercise facilitates WAT lipolysis to provide FFA for utilization as fuel29. Although this lipolysis was typically attributed to adrenaline release40, acute exercise in humans also releases additional molecules79, such as growth and differentiation factor 15 (GDF15)80 and IL-6 (ref.81), which also affect lipolysis (Table 3; Supplementary Table 1). Lipolysis is not the only avenue by which exerkines can affect adipose tissue mass. For example, in myonectin knockout mice, WAT lipolysis is unaffected; however, dietary lipid clearance is impaired compared with lipid clearance in wild-type mice, resulting in increased WAT mass and decreased liver steatosis82.
A potential effect of exercise on WAT is ‘browning’, where WAT increases mitochondrial content, metabolic rate and heat production. WAT browning might have metabolic importance, as individuals with PET–CT-defined BAT had a decreased prevalence of cardiometabolic disease, particularly if they had overweight or obesity83. In a mouse model, fibronectin type III domain containing 5 is cleaved in the muscle cell and secreted as irisin, which induces WAT browning to increase energy expenditure and consequently reduce obesity84. Transgenic mice that overexpress muscle peroxisome proliferator-activated receptor-γ coactivator 1-α (PGC1α) have higher circulating levels of irisin and increased WAT browning than control mice84. Hence, the initial excitement regarding irisin as an exerkine, as exercise generally increases muscle PGC1α expression in both animal models85 and humans86.
As the irisin findings and exercise-induced browning of WAT concepts were re-evaluated in humans, the initial excitement was subsequently tempered. Although acute exercise in humans generally increases plasma levels of irisin87, the effect of chronic exercise training remains highly variable. A meta-analysis of several randomized controlled trials even showed lower levels of irisin after training than before training88. Trained athletes have lower BAT activity and no difference in WAT browning markers compared with lean, sedentary men89; this observation is supported by a study in humans of chronic exercise training, which did not find any browning of WAT (as assessed by biopsy)90. Thus, whether exercise can brown WAT in humans, especially through an irisin-mediated pathway, remains controversial55,83,84,90.
Adipose tissue can also secrete exerkines. A prime example is 12,13-dihydroxy-9Z-octadecenoic acid (12,13-diHOME), which is secreted from BAT and increases skeletal muscle oxidative capacity91. In humans, circulating levels of 12,13-diHOME are inversely associated with adipose tissue mass, fasting blood levels of insulin and blood levels of triacylglycerol92. A 2021 study showed that BAT transplantation in mice increased plasma levels of 12,13-diHOME and improved cardiac haemodynamics93. These findings suggest that a sustained increase in plasma levels of 12,13-diHOME preserves cardiac function and remodelling and increases cardiac haemodynamics through a direct effect on the cardiomyocyte. These findings were reinforced by observations in humans, in whom the presence of cardiovascular disease is associated with decreased plasma levels of 12,13-diHOME93.
Interestingly, skeletal muscle can influence the adipose tissue response to exercise via lactate secretion. The prototypical example is transforming growth factor-β2 (TGFβ2)42. In a mouse model, specific lactate exposure in vitro and in vivo increased adipocyte expression of TGFβ2 (ref.42). Furthermore, the same study found that in a mouse model of chronic exercise, increased adipocyte levels of TGFβ2 expression and secretion were associated with improvements in glucose metabolism, lipid oxidation and a possible reduction of adipose tissue inflammation. Parallel findings were also observed in humans undertaking chronic exercise, albeit to a less pronounced degree than the animal model observations42. Nevertheless, these findings demonstrate the possibility of lactate mediating tissue-to-tissue communication during exercise.
Skeletal muscle
Exerkines originating from multiple tissues have demonstrated the capacity to improve skeletal muscle function and growth (Table 3; Supplementary Table 1). Apelin is an example of a myokine affecting muscle function. In both humans and animal models, exercise increases muscle mRNA levels of apelin94 and possibly serum levels of apelin95,96. In an animal model, skeletal muscle95,96 served as a source of apelin secretion, which improved skeletal muscle function in the setting of ageing, supporting the potential of apelin as a therapeutic to combat age-related sarcopenia94,95,96. Specifically in old mice, increased apelin exposure (by daily injection or skeletal muscle overexpression) stimulated muscle mitochondrial biogenesis, muscle protein synthesis and enhancement of muscle stem cells to stimulate muscle regeneration96. 12,13-diHOME is an example of a batokine with muscle effects. In both humans and mouse models, exercise facilitates BAT secretion of 12,13-diHOME, which enhances skeletal muscle FFA uptake and oxidation91. The hepatokines follistatin and fetuin-A also affect muscle function. For example, in both humans97,98,99 and mouse models100, acute exercise97,100 and chronic exercise98 increase liver-secreted follistatin, which has been reported to antagonize the effects of myostatin99. Decreased function of myostatin enhances skeletal muscle growth and improves whole-body glycaemic control44,99. Furthermore, fetuin-A worsens peripheral insulin resistance by reducing insulin signalling and glucose transporter type 4 trafficking39. Although acute exercise in humans does not alter plasma levels of fetuin-A97, chronic exercise might decrease plasma levels of fetuin-A72,101. Additional exerkines involved in muscle growth and development include the following: IL-7 (ref.102), IL-15 (ref.99), follistatin97, leukaemia inhibitory factor103, syndecan 4 (ref.104) and myostatin44,73.
The liver and the gut
Exercise reduces hepatic steatosis independently of weight loss105. The liver is recognized as a source for many circulating proteins, with ~2,500 liver-secreted proteins identified using modern liquid chromatography and mass spectroscopy technologies39. Not surprisingly, the liver is the source of many acute exercise-responsive cytokines (Supplementary Table 1). These exerkines affect glucose and/or lipid metabolism (for example, angiopoietin-like protein 4 in humans and animal models39,79), browning of WAT (FGF21 in a mouse model106), lipolysis (FGF21 in humans and a mouse model77) and the maintenance of cellular homeostasis (heat shock protein 72 in humans107).
Exercise also alters the gut microbiome108. Chronic exercise in humans and animal models alters the composition and functional capacity of the gut microbiota, independently of diet; these exercise-dependent changes in the microbiota might be independent of weight while being contingent on exercise intensity, modality and sustainment108. In humans, chronic exercise altered the gut microbiome to increase availability of short chain fatty acids, particularly butyrate109. Once these participants ceased training, exercise-induced changes in the microbiota were largely reversed when re-measured after a 6-week sedentary period109. The mechanisms by which exercise might alter the gut microbiome remain numerous, including altering the gene expression of intraepithelial lymphocytes for a more favourable inflammatory profile110, influencing blood flow in the gut111 or changing bile acid excretion112.
The endocrine system
As exercise has established benefits in improving dysglycaemia, this section focuses specifically on exerkines affecting glucose homeostasis (Table 3; Supplementary Table 1). In humans, circulating levels of β-aminoisobutyric acid (BAIBA) increased with chronic training55 and inversely correlated with insulin resistance55. In wild-type mice, BAIBA treatment reduced insulin resistance and suppressed inflammation55. In another study using C2C12 mouse myocytes and a wild-type mouse model (palmitate or high-fat diet exposure), BAIBA treatment attenuated insulin resistance, reduced inflammation and increased fatty acid oxidation through AMP-activated protein kinase (AMPK) and a AMPK–PPARδ-dependent pathway in skeletal muscle113. Limited human data show that an acute exercise bout increases plasma and muscle expression levels of fractalkine (encoded by CX3CL1)70, which is a chemokine that favourably regulates glucose-stimulated insulin secretion by enhancing β-cell function114. Chronic exercise in humans also reduces circulating levels of fetulin-A72,101. Fetulin-A has been shown to impair β-cell sensing by reducing glucose-stimulated insulin secretion115.
In humans, both acute exercise97 and chronic exercise98 increase circulating levels of follistatin. The extent to which follistatin might improve glycaemic measures remains controversial. After bariatric surgery, improvements in HbA1c have been observed in the setting of reduced levels of follistatin116. Furthermore, inactivating hepatic follistatin in a mouse model improved WAT sensitivity and reduced hepatic glucose production116. In vitro, irisin prevented excessive lipogenesis of mouse islets under glucolipotoxic conditions, resulting in improved insulin secretion, inhibition of apoptosis and restored β-cell function-related gene expression117.
The myokine IL-6 is also associated with favourable alterations in glucose homeostasis. In humans, IL-6 infusion delays gastric emptying and lowers postprandial glucose levels118. In rodents, increasing IL-6 by exercise or by IL-6 injection increases the production of glucagon-like peptide 1 by intestinal L cells and pancreatic α-cells to enhance glucose-stimulated insulin secretion. These benefits of IL-6 in enhancing insulin secretion were seen across multiple rodent models of T2DM119. In healthy humans, IL-6 infusion to levels similar to those seen with strenuous exercise enhances insulin-stimulated glucose-uptake but does not alter whole-body lipolysis or lipid oxidation120. However, another study of IL-6 infusion into humans found that IL-6 stimulates lipolysis and lipid oxidation54,121. Further research into these seemingly conflicting findings is warranted to establish the effect of exerkines on glucose metabolism.
The immune system
The broad effects of exercise on immune function implicate mobilization and altered function of cytokines and immune cells, such as neutrophils, leukocytes and natural killer cells (Fig. 3; Supplementary Table 1)30,122,123. The effects of chronic exercise on the immune system might depend on intensity, with immune enhancement by moderate exercise and possible impairment by strenuous exercise124. As shown in humans, an acute bout of exercise might be initially pro-inflammatory, but subsequently this effect is offset by an anti-inflammatory response30,124. The exercise-induced acute increase in circulating levels of IL-6 increases plasma levels of anti-inflammatory cytokines, such as IL-1RA and IL-10 (ref.125). IL-1RA inhibits IL-1β signal transduction126, whereas IL-10 inhibits production of pro-inflammatory cytokines, such as TNF127. In healthy humans, one bout of exercise or an IL-6 infusion blunted the increase in circulating levels of TNF induced by infusion of lipopolysaccharide128. Thus, an acute bout of exercise induces anti-inflammatory effects that might in part be mediated by IL-6, possibly in conjunction with other known anti-inflammatory factors, such as adrenaline and cortisol122. As a pleiotropic factor, the effect of IL-6 on metabolism and inflammation remains context-dependent. Although IL-6 is transiently increased after acute exercise, the baseline (or ‘resting’) circulating levels of IL-6 are lower in exercise-trained individuals than in untrained individuals78. Future studies focusing on tissue and cell type-specific effects as well as different exercise regimens will help delineate the temporal and spatial requirement of IL-6 in mediating exercise benefits.
Exercise induces lipid oxidation, mitochondrial biogenesis and local injury, which stimulates exerkine release into the circulation to influence the immune system. See Supplementary Table 1 for detailed effects and relevant references. These include proteins (blue lines), metabolites (yellow circles) and extracellular vesicles (green circles), which have a multitude of effects on the immune system (generically represented by a monocyte). Acutely, exercise increases cytokines such as circulating levels of transforming growth factor β1 (TGFβ1) and IL-6 relative to the resting state. This change results in acute inflammation, characterized by increases in tumour necrosis factor (TNF) and IL-6. Once the acute exercise-induced effects have diminished, an increase in anti-inflammatory cytokines (such as IL-10 and IL-1 receptor antagonist (IL-1RA)) occurs in response to the acute inflammatory response. Chronic training is associated with a reduction in systemic and tissue inflammation, as characterized by lower circulating levels of TNF and IL-6 in the resting state, relative to sedentary individuals. Reduced insulin resistance and tumour growth has been attributed to the effects of chronic training on decreasing systemic and/or tissue inflammation.
An emerging frontier in exercise biology involves exerkine-induced immune effects in increasing resilience to cancer or as co-adjuvant to cancer therapy. The anticancer effects of exercise might not be limited to its effect on body weight. A meta-analysis pooled data from 12 prospective cohorts with self-reported physical activity and found that increased physical activity levels are associated with decreased risk of incident cancer across multiple types; many of these associations remained even after adjusting for BMI129. Acute exercise creates a unique exerkine milieu that lasts several hours after exercise cessation, which provides a temporal window for immune function stimulation31. For this reason, exercise could potentially serve as a co-adjuvant treatment for cancer therapy. In tumour-bearing mouse models (across five tumour models), mice that undertook voluntary wheel running had a reduction of more than 60% in tumour incidence and tumour growth compared with sedentary mice. Further analysis of these mouse models showed that adrenaline and IL-6 induced natural killer cell mobilization, redistribution and tumour infiltration to inhibit tumour growth123. Another mouse model found that exercise metabolites such as lactate and possibly tricarboxylic acid intermediates enhance the antitumour effector profile of CD8+ lymphocytes130. Of note, exercise is associated with enhanced secreted protein acidic and rich in cysteine (SPARC) secretion in humans and animal models131; this matricellular protein regulates cell function and tissue remodelling, while inhibiting proliferation and promoting apoptosis of a mouse colon cancer cell line132.
Crosstalk exists between skeletal muscle and the immune system. Contemporary views towards skeletal muscle now consider muscle as an immunoregulatory organ that especially affects lymphocyte and neutrophil trafficking and inflammation. During acute exercise, immune cells are mobilized by muscle secretion of exerkines such as fractalkine to enhance regeneration (in humans)133 or meteorin-like (METRNL) to increase beige adipose tissue thermogenesis (animal model)134. As previously noted, one bout of exercise or an IL-6 infusion in humans blunts the increase in circulating levels of TNF that are induced by lipopolysaccharide infusion128.
IL-13 is an important main T helper 2 (TH2) cell cytokine that mediates the anti-inflammatory polarization of resident macrophages in WAT135. IL-13 is also an exerkine, increasing in the circulation after exercise training in humans and mice136. Mice lacking IL-13 show reduced running capacity and do not show certain beneficial effects of exercise training, such as improvements in glucose tolerance and endurance running capacity136. Unlike IL-6, IL-13 is produced by type 2 innate lymphoid cells (ILC2s) in skeletal muscle. As IL-13-deficient mice show defective muscle fatty acid utilization after acute exercise and fail to show increased muscle mitochondrial biogenesis after chronic exercise, the ILC2 to IL-13 axis might have an important role in the metabolic adaptation to exercise training136. Interestingly, ILC2 and TH2 cell cytokines also control beige adipocyte recruitment in rodents137, suggesting that ILC2 to TH2 signalling might partially mediate exercise-induced beiging of WAT. The stimulants within skeletal muscle or WAT that activate ILC2s during exercise remain to be identified.
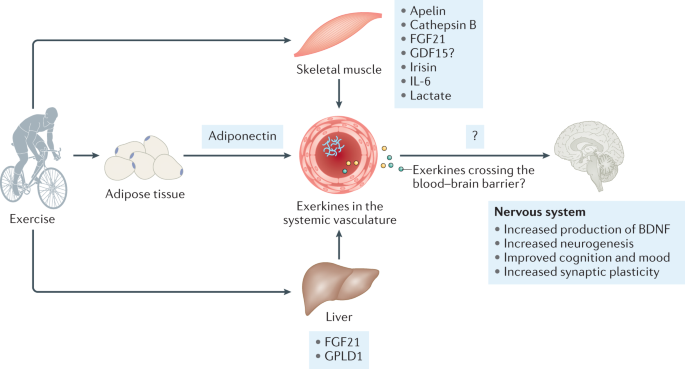
The nervous system
Exercise is a promising non-pharmacological strategy to maintain and improve brain function138. Figure 4 presents an overview of the purported effects of exercise on the nervous system (Supplementary Table 1). Of note, evidence for the benefits of exercise on cognition remains variable, probably owing to the lack of randomized controlled trials throughout the lifespan with standardized exercise interventions and comparable methods for cognitive assessment139,140,141,142. The effects of exercise on the brain are most apparent in the hippocampus, a part of the brain involved in learning and memory143. In older adults (aged 55–80 years), participation in an aerobic walking programme increased hippocampal volume and improved memory144. Moreover, accumulating evidence suggests that physical activity, as shown in preclinical, observational and interventional studies in humans, can prevent or delay the onset of neurodegenerative conditions138. In humans, acute exercise increases plasma levels of brain-derived neurotrophic factor (BDNF)7, whereas chronic exercise training has been shown to not alter140, increase or even decrease plasma levels of BDNF140,145. In rodents, chronic exercise upregulates BDNF in the hippocampus, which is essential for adult hippocampal neurogenesis and neural plasticity146. Chronic exercise in rodents also enhances hippocampal synaptic plasticity, adult neurogenesis and neurotrophin levels, as well as memory function147. In addition, voluntary wheel running in rodents increases the number of new hippocampal neurons, enhances morphological maturation, such as dendritic branching and spine density, and alters the circuitry of adult-born neurons147.
Exercise stimulates the production of exerkines from tissues, such as skeletal muscle, adipose tissue or the liver, to affect the nervous system. See Supplementary Table 1 for detailed effects and relevant references. These exerkines are released into the circulation and include proteins (blue lines), metabolites (yellow circles) and extracellular vesicles (green circles), which have a multitude of purported effects on the nervous system. These effects include increasing production of brain-derived neurotrophic factor (BDNF), enhancing neurogenesis (even in adults), cognition, mood and synaptic plasticity. The extent to which exerkines cross the blood–brain barrier to exert their effects remains unknown, symbolized by the question mark. There is uncertainty with GDF15, as symbolized by the question mark, as pharmacological GDF15 inhibits appetite and reduces activity, whereas physiological induction of GDF15 by exercise does not200. Commonly described exerkines are noted. FGF21, fibroblast growth factors 21; GDF15, growth and differentiation factor 15; GPLD1, glycosylphosphatidylinositol-specific phospholipase D1.
There is increasing recognition that peripheral factors might trigger the effects of exercise on the brain. In the past 20 years, researchers have begun to test the hypothesis that metabolites, peptides and proteins released from liver, adipocytes, blood cells (particularly platelets) and muscle might influence the central nervous system138,148,149. Since 2020, several studies have transferred plasma from exercised animals into sedentary animals, with subsequent improvements in cognitive function, supporting the presence of a transferable factor in improving cognitive function148,149. Evidence is now accumulating that factors released from non-neuronal tissue148,149,150,151,152 and delivered via the vasculature to the brain might have important roles in synaptic plasticity, memory function and mood regulation150. Adiponectin is an adipocyte-secreted protein that seems to have neuroprotective effects151, in addition to its insulin-sensitizing, anti-inflammatory and anti-atherogenic effects151,153. In mice, adiponectin was demonstrated to pass through the blood–brain barrier and was associated with increased neurogenesis and reduced depression-like behaviours151. Interestingly, discrepancies can exist between the plasma levels of adiponectin and levels in the cerebrospinal fluid. For example, in humans, acute exercise increases plasma levels of adiponectin but decreases cerebrospinal fluid levels of adiponectin154. The mechanisms underlying the beneficial effects of exercise on brain structure and function remain an active area of investigation.
Muscle–brain crosstalk
Myokines seem to have an important role in hippocampal neurogenesis (animal model) and neurotrophin levels (animal model), and enhanced cognition and mood (animal model and humans) (Supplementary Table 1). For instance, in mice, increasing intrinsic irisin expression in neurons or increasing plasma levels of irisin elevates hippocampal Bdnf gene expression152. Irisin administration in a mouse model of Alzheimer disease improves synaptic plasticity and memory function155,156. In both animal models and humans, plasma levels of cathepsin B, a lysosomal thiol proteinase produced by muscle, is positively associated with hippocampus-dependent memory145,157. Studies in humans have shown that acute exercise does not clearly increase plasma levels of cathepsin B7, although chronic exercise does increase plasma levels of cathepsin B145,157. These same studies also showed that acute exercise increases plasma levels of BDNF7, whereas chronic exercise does not increase BDNF140,145 suggesting that investigation of local neuronal effects remains warranted.
Liver–brain crosstalk
The liver secretes factors that are important for brain function. Kynurenine is a metabolite of the amino acid L-tryptophan and is primarily synthesized in the liver. In both mice and humans, chronic aerobic training increases muscle expression of kynurenine aminotransferase, which facilitates conversion of kynurenine into kynurenic acid, a metabolite that is unable to cross the blood–brain barrier. This shift in kynurenine metabolism is able to protect the brain from stress-induced depression150.
Exchanging plasma from exercising aged mice to sedentary aged mice enhances adult hippocampal neurogenesis and memory function148. Upon further investigation, plasma proteomic analysis led to the identification of a novel hepatokine, glycosylphosphatidylinositol-specific phospholipase D1 (GPLD1), which increases after exercise and correlates with improved cognitive function in aged mice. These findings are supported in humans, as concentrations of GPLD1 in blood were higher in active, healthy older adults (n = 20, >66 years old) than in their sedentary counterparts148. Investigations into the underlying mechanisms indicate that GPLD1 does not cross the blood–brain barrier148. Hence, the benefit of GPLD1 (ref.148) and other exerkines on brain structure and function might relate to its peripheral effects, such as the complement signalling cascade149,158, or coagulation159. Additional exercise studies are needed to better appreciate the exercise–liver–brain axis.
Bone
Exercise, especially resistance exercise, increases bone mineral desnity160. Multiple mechanisms exist, although mechanical loading is considered a major factor161. Noted exercise-associated bone-derived factors affecting bone formation include TGFβ1 (ref.162) and sclerostin163. Sclerostin inhibits bone formation163,164 and blood levels of sclerostin are lower in highly active humans than in sedentary humans163. Emerging data demonstrate that crosstalk exists between bone and muscle, probably mediated by secretory factors165. Noted myokines affecting the bone include apelin166, myostatin61, irisin167, IL-6 (ref.168), IL-7 (ref.60) and BAIBA59 (Supplementary Table 1).
Gaps and future opportunities
Gaps in exerkine science
Contentious questions remain that temper the enthusiasm regarding exerkines (Box 1). These controversies include the lack of consistency between the acute and chronic exercise response, discrepancies between humans and animal models of exercise and interpretation challenges due to variability in outcomes and sampling. These knowledge gaps set the stage for future opportunities in exerkine research.
Despite the acceleration in exerkine-related research since the identification of IL-6 as a myokine in 2000 (ref.16), much remains to be done in the scientific areas of research, technology and therapeutic interventions (Box 1). Specifically, a critical need exists to move beyond the ‘skeletal muscle-centric’ view of exerkines and focus more on their roles in inter-organ communication, tissue regeneration, immune regulation, metabolic adaptation, cardiovascular fitness, psychological health and overall health across the lifespan. The vasculature and endothelium are emerging as a probable central facilitator, which enables systemic exerkines to exert their specific effects within the various local environments, as well as being a direct target and source of exerkines. Understanding the system-wide effects of exercise and the myriad of exercise-related improvements is essential for understanding resilience. Such knowledge will provide new translational research opportunities to develop novel, targeted interventions that increase physiological reserve, maintain and/or enhance resiliency and thus promote healthy ageing, as well as interventions that prevent and treat comorbidities and chronic disease.
Many more exerkines, and their sources, targets and mechanisms, remain to be discovered. In 2016, the MoTrPAC project was launched to uncover novel exerkines through deep omics profiling of biomaterial from humans and rodents before and after acute exercise as well as chronic exercise training. As potential candidate transducers are uncovered, follow-up mechanistic studies will be required to delineate their function. In addition to molecular discoveries, substantial work remains to decipher the dosage and type of exercise needed to elicit positive health outcomes. Intervention studies are needed to investigate the effect of different types of exercise on resilience to various conditions, with guidance available from the NIH in designing resilience-based studies. To address these knowledge gaps, detailed studies are needed to identify and validate the exerkine responses after exercise (acute, chronic or intermittent) exposure, including a detailed post-exercise response. Certainly, the demographics and phenotypes of the population will matter, as the response in healthy participants can vary greatly from that in participants with comorbidities. Further work in these areas will advance our understanding of ageing, health and disease prevention.
Opportunities for new technologies
Technology gaps also remain in exerkine research. One emerging area is the use of wearable technologies and devices to capture quantitative and dynamic phenotypes over long periods of time in healthy individuals as well as in those with mild or severe diseases. For instance, wearable technology could provide valuable information regarding physical activity levels and exercise capacity during and following COVID-19 illness and recovery, adding to the description of post-acute sequelae of SARS-CoV-2 infection, which is under active investigation. Currently, non-invasive and minimally invasive devices have enabled the monitoring of many behavioural and physiological phenotypes, including heart rate and electrical activity in the heart (ECG), body temperature, physical activity and sedentary behaviour, peripheral blood oxygen saturation and blood concentrations of glucose. These devices enable the real-time monitoring of the effects of exercise in natural and controlled settings at an unprecedented level. Moreover, wearable technologies can be scaled to the analysis of over a million people and can enable ‘citizen science’ whereby individuals with devices can readily participate in studies. These measurements, when combined with molecular measurements such as exerkines, have the potential to greatly improve our understanding of exercise adaptations in large cohorts with deep phenotyping across a broad age range.
Although wearable devices are powerful, multiple challenges remain in data interpretation and analysis. These challenges include device accuracy as well as device standardization and a lack of readily available high-resolution data from the manufacturers. In addition, many wearable devices do not characterize the environmental context associated with data capture. For example, if a device does not sense any physical activity, one explanation could be the lack of movement by the wearer while another explanation could be device removal. A remaining challenge entails approval and regulation from entities such as the FDA before widespread use of wearables as therapeutic interventions.
In addition to wearables, the technology, analysis and approach for exerkine discovery needs to be further developed. Deep omics profiling (transcriptome, metabolome, proteome and lipidome) of human and animal-based exerkines is occurring in MoTrPAC; this effort is expected to reveal novel molecules and mechanisms involved in exercise by providing a more comprehensive view of the multi-omics landscape of exerkines to the research community. Extracellular vesicle analysis, especially of exosomes, will be a critical component of MoTrPAC’s analysis owing to burgeoning interest in the role of extracellular vesicles as carriers of molecular signals and drivers of inter-organ crosstalk.
Data reporting and data sharing
To promote comparison between studies and enhance translation, a crucial need exists for the establishment of community-wide standards for data reporting and data sharing. As an example, capturing physical activity and body composition (for example, adipose tissue mass) in the electronic health record will facilitate electronic health record data mining to examine clinical outcomes outside a structured clinical study. Cross-study comparisons of exercise studies will be facilitated by setting standards for a minimum metadata set, for consistent documentation and of covariates, such as time of day, diet or exercise exposure. Advances in computational modelling will accelerate our understanding of the physiological process of exercise and exerkine effects. Establishing a uniform knowledge base remains a critical next step in driving this process.
Exerkines as therapeutics
The health benefits of exercise are well documented. However, not all individuals are able to benefit from exercise owing to physical limitations, such as paraplegia, or imposed limitations, such as quarantining during the current COVID-19 pandemic. Moreover, in humans, metabolic non-response or even adverse responses to exercise have been described26. As the role of exerkines and their biological effects are increasingly clarified, exerkines could potentially be harnessed to mimic the benefits of exercise in individuals who are limited in their exercise capacity or to counterbalance a metabolic non-response or adverse response to exercise. Although this ‘exercise in a pill’ is currently wishful thinking, it remains a tantalizing goal for future research directions.
Conclusions
Although exercise exerts many beneficial effects across multiple organ systems, our understanding of the mechanisms driving the benefits of exercise and the variability in these benefits remains rudimentary. Much of the initial exerkine research has been focused on skeletal muscle; however, contemporary research is now rapidly expanding to include non-skeletal muscle-based sources and targets for exerkines that contribute to maintaining and restoring health. Exerkines are increasingly recognized as critical mediators of exercise-related changes and health benefits, particularly in their role in inter-organ and systemic communication and coordination. Yet, much remains to be done. To improve translation of results, the heterogeneity across studies needs to be minimized by reducing exposure variability and using standardized, consistent outcome measures. Large-scale, structured studies will be key resources in providing a structured environment to pursue future exerkine-related questions. In summary, exerkines are a highly promising direction for future research initiatives, with high potential as biomarkers to predict outcomes, facilitate personalized exercise programmes to improve health, reduce disease and promote resilience across the lifespan.
References
Piercy, K. L. et al. The physical activity guidelines for Americans. J. Am. Med. Assoc. 320, 2020–2028 (2018).
Katzmarzyk, P. T., Church, T. S., Craig, C. L. & Bouchard, C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med. Sci. Sports Exerc. 41, 998–1005 (2009).
Ding, D. et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 388, 1311–1324 (2016).
Trabelsi, K. et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol. Sport. 38, 495–506 (2021).
Sallis, R. et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br. J. Sports Med. 55, 1099–1105 (2021).
Cullen, T., Thomas, A. W., Webb, R. & Hughes, M. G. Interleukin-6 and associated cytokine responses to an acute bout of high-intensity interval exercise: the effect of exercise intensity and volume. Appl. Physiol. Nutr. Metab. 41, 803–808 (2016).
Nicolini, C. et al. A single bout of high-intensity interval exercise increases corticospinal excitability, brain-derived neurotrophic factor, and uncarboxylated osteolcalcin in sedentary, healthy males. Neuroscience 437, 242–255 (2020).
Pate, R. R. et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. J. Am. Med. Assoc. 273, 402–407 (1995).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Troiano, R. P. et al. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 40, 181–188 (2008).
Safdar, A., Saleem, A. & Tarnopolsky, M. A. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat. Rev. Endocrinol. 12, 504–517 (2016). This paper coined the concept of ‘exerkines’, molecules that are altered in response to acute and chronic exercise, and mediate the systemic adaptations to exercise.
Ransom, F. A contribution to the study of muscle-enzymes. J. Physiol. 40, 1–16 (1910).
Goldstein, M. S. Humoral nature of the hypoglycemic factor of muscular work. Diabetes 10, 232–234 (1961).
Janssen, I., Heymsfield, S. B., Wang, Z. & Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 89, 81–88 (2000).
Pedersen, B. K. Muscle as a secretory organ. Compr. Physiol. 3, 1337–1362 (2013).
Steensberg, A. et al. Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6. J. Physiol. 529, 237–242 (2000). A key paper demonstrating that IL-6 is secreted by contracting muscle, identifying IL-6 as the first ‘myokine’.
Baggish, A. L. et al. Dynamic regulation of circulating microRNA during acute exhaustive exercise and sustained aerobic exercise training. J. Physiol. 589, 3983–3994 (2011).
Vechetti, I. J. Jr, Valentino, T., Mobley, C. B. & McCarthy, J. J. The role of extracellular vesicles in skeletal muscle and systematic adaptation to exercise. J. Physiol. 599, 845–861 (2021).
Sanford, J. A. et al. Molecular Transducers of Physical Activity Consortium (MoTrPAC): mapping the dynamic responses to exercise. Cell 181, 1464–1474 (2020).
National Heart, Lung, and Blood Institute. NHLBI and NIDDK Workshop: exerkines in health, resilience, and diseases executive summary, https://www.nhlbi.nih.gov/events/2020/nhlbi-and-niddk-workshop-exerkines-health-resilience-and-diseases-executive-summary (2020).
Gabriel, B. M. & Zierath, J. R. Circadian rhythms and exercise–re-setting the clock in metabolic disease. Nat. Rev. Endocrinol. 15, 197–206 (2019).
Parr, E. B., Heilbronn, L. K. & Hawley, J. A. A time to eat and a time to exercise. Exerc. Sport. Sci. Rev. 48, 4–10 (2020).
van Loon, L. J. et al. Influence of prolonged endurance cycling and recovery diet on intramuscular triglyceride content in trained males. Am. J. Physiol. Endocrinol. Metab. 285, E804–E811 (2003).
Sato, S. et al. Atlas of exercise metabolism reveals time-dependent signatures of metabolic homeostasis. Cell Metab. 34, 329–345.e8 (2022). Using a mouse model, this paper presents a detailed atlas of the response to a single bout of exercise at different times, highlighting the influence of exercise timing on tissue changes and exerkine secretion.
Bouchard, C. et al. Familial aggregation of V˙O2max response to exercise training: results from the HERITAGE Family Study. J. Appl. Physiol. 87, 1003–1008 (1999).
Bouchard, C. et al. Adverse metabolic response to regular exercise: is it a rare or common occurrence? PLoS ONE 7, e37887 (2012).
Leuchtmann, A. B., Adak, V., Dilbaz, S. & Handschin, C. The role of the skeletal muscle secretome in mediating endurance and resistance training adaptations. Front. Physiol. 12, 709807 (2021).
Wahren, J., Felig, P., Ahlborg, G. & Jorfeldt, L. Glucose metabolism during leg exercise in man. J. Clin. Invest. 50, 2715–2725 (1971).
Horowitz, J. F. & Klein, S. Lipid metabolism during endurance exercise. Am. J. Clin. Nutr. 72, 558s–563s (2000).
Ostrowski, K., Rohde, T., Asp, S., Schjerling, P. & Pedersen, B. K. Pro- and anti-inflammatory cytokine balance in strenuous exercise in humans. J. Physiol. 515, 287–291 (1999). One of the earliest papers to examine the effect of acute strenuous exercise, marathon running, on plasma concentrations of pro-inflammatory and anti-inflammatory cytokines.
Contrepois, K. et al. Molecular choreography of acute exercise. Cell 181, 1112–1130.e16 (2020).
Keller, C. et al. Effect of exercise, training, and glycogen availability on IL-6 receptor expression in human skeletal muscle. J. Appl. Physiol. 99, 2075–2079 (2005).
Reuter, J. A., Spacek, D. V. & Snyder, M. P. High-throughput sequencing technologies. Mol. Cell 58, 586–597 (2015).
Safdar, A. & Tarnopolsky, M. A. Exosomes as mediators of the systemic adaptations to endurance exercise. Cold Spring Harb. Perspect. Med. 8, a029827 (2018).
Liangsupree, T., Multia, E. & Riekkola, M.-L. Modern isolation and separation techniques for extracellular vesicles. J. Chromatogr. A 1636, 461773 (2021).
Artoni, A. et al. Residual platelets are the main determinants of microparticles count in frozen-thawed plasma. Thrombosis Res. 130, 561–562 (2012).
Vanderboom, P. M. et al. A size-exclusion-based approach for purifying extracellular vesicles from human plasma. Cell Rep. Methods 1, 100055 (2021).
Giudice, J. & Taylor, J. M. Muscle as a paracrine and endocrine organ. Curr. Opin. Pharmacol. 34, 49–55 (2017).
Watt, M. J., Miotto, P. M., De Nardo, W. & Montgomery, M. K. The liver as an endocrine organ–linking NAFLD and insulin resistance. Endocr. Rev. 40, 1367–1393 (2019).
Kjær, M., Secher, N. H. & Galbo, H. Physical stress and catecholamine release. Baillières Clin. Endocrinol. Metab. 1, 279–298 (1987).
Nalbandian, M. & Takeda, M. Lactate as a signaling molecule that regulates exercise-induced adaptations. Biology 5, 38 (2016).
Takahashi, H. et al. TGF-β2 is an exercise-induced adipokine that regulates glucose and fatty acid metabolism. Nat. Metab. 1, 291–303 (2019). This paper demonstrated that TGFβ2 is secreted from adipose tissue in response to exercise and improves glucose tolerance.
Subbotina, E. et al. Musclin is an activity-stimulated myokine that enhances physical endurance. Proc. Natl Acad. Sci. USA 112, 16042–16047 (2015).
McPherron, A. C., Lawler, A. M. & Lee, S. J. Regulation of skeletal muscle mass in mice by a new TGF-p superfamily member. Nature 387, 83–90 (1997). This is a key paper describing myostatin (GDF8), which inhibits muscle growth.
Jensen, L., Bangsbo, J. & Hellsten, Y. Effect of high intensity training on capillarization and presence of angiogenic factors in human skeletal muscle. J. Physiol. 557, 571–582 (2004).
Richardson, R. S. et al. Exercise adaptation attenuates VEGF gene expression in human skeletal muscle. Am. J. Physiol. Heart Circ. Physiol. 279, H772–H778 (2000).
Kim, I. et al. Angiopoietin-1 regulates endothelial cell survival through the phosphatidylinositol 3′-kinase/Akt signal transduction pathway. Circ. Res. 86, 24–29 (2000).
Frydelund-Larsen, L. et al. Exercise induces interleukin-8 receptor (CXCR2) expression in human skeletal muscle. Exp. Physiol. 92, 233–240 (2007).
Ding, Y. H. et al. Cerebral angiogenesis and expression of angiogenic factors in aging rats after exercise. Curr. Neurovasc Res. 3, 15–23 (2006).
Pedersen, B. K. Muscles and their myokines. J. Exp. Biol. 214, 337–346 (2011).
McConell, G. K., Rattigan, S., Lee-Young, R. S., Wadley, G. D. & Merry, T. L. Skeletal muscle nitric oxide signaling and exercise: a focus on glucose metabolism. Am. J. Physiol. Endocrinol. Metab. 303, E301–E307 (2012).
Tejero, J., Shiva, S. & Gladwin, M. T. Sources of vascular nitric oxide and reactive oxygen species and their regulation. Physiol. Rev. 99, 311–379 (2019).
Koliatsos, V. E., Clatterbuck, R. E., Winslow, J. W., Cayouette, M. H. & Price, D. L. Evidence that brain-derived neurotrophic factor is a trophic factor for motor neurons in vivo. Neuron 10, 359–367 (1993).
Knudsen, J. G. et al. Skeletal muscle IL-6 regulates muscle substrate utilization and adipose tissue metabolism during recovery from an acute bout of exercise. PLoS ONE 12, e0189301 (2017).
Roberts, L. D. et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell Metab. 19, 96–108 (2014). Using a mouse model, this paper demonstrated that a myokine, BAIBA, can ‘brown’ WAT to improve glucose homeostasis.
Fisher, F. M. et al. FGF21 regulates PGC-1α and browning of white adipose tissues in adaptive thermogenesis. Genes Dev. 26, 271–281 (2012).
Nielsen, A. R. et al. Association between interleukin-15 and obesity: interleukin-15 as a potential regulator of fat mass. J. Clin. Endocrinol. Metab. 93, 4486–4493 (2008).
Yamauchi, T. et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat. Med. 8, 1288–1295 (2002).
Kitase, Y. et al. β-aminoisobutyric Acid, l-BAIBA, is a muscle-derived osteocyte survival factor. Cell Rep. 22, 1531–1544 (2018).
Weitzmann, M. N., Roggia, C., Toraldo, G., Weitzmann, L. & Pacifici, R. Increased production of IL-7 uncouples bone formation from bone resorption during estrogen deficiency. J. Clin. Invest. 110, 1643–1650 (2002).
Dankbar, B. et al. Myostatin is a direct regulator of osteoclast differentiation and its inhibition reduces inflammatory joint destruction in mice. Nat. Med. 21, 1085–1090 (2015).
Watanabe-Takano, H. et al. Mechanical load regulates bone growth via periosteal osteocrin. Cell Rep. 36, 109380 (2021).
Melouane, A., Yoshioka, M., Kanzaki, M. & St-Amand, J. Sparc, an EPS-induced gene, modulates the extracellular matrix and mitochondrial function via ILK/AMPK pathways in C2C12 cells. Life Sci. 229, 277–287 (2019).
Heinemeier, K. M., Bjerrum, S. S., Schjerling, P. & Kjaer, M. Expression of extracellular matrix components and related growth factors in human tendon and muscle after acute exercise. Scand. J. Med. Sci. Sports 23, e150–e161 (2013).
Kim, J. & Lee, J. Role of transforming growth factor-β in muscle damage and regeneration: focused on eccentric muscle contraction. J. Exerc. Rehabil. 13, 621–626 (2017).
Imai, T. et al. Identification and molecular characterization of fractalkine receptor CX(3)CR1, which mediates both leukocyte migration and adhesion. Cell 91, 521–530 (1997).
Gao, Y. & Galis, Z. S. Exploring the role of endothelial cell resilience in cardiovascular health and disease. Arterioscler. Thromb. Vasc. Biol. 41, 179–185 (2020).
Cullberg, K. B. et al. Effect of weight loss and exercise on angiogenic factors in the circulation and in adipose tissue in obese subjects. Obesity 21, 454–460 (2013).
Gavin, T. P., Drew, J. L., Kubik, C. J., Pofahl, W. E. & Hickner, R. C. Acute resistance exercise increases skeletal muscle angiogenic growth factor expression. Acta Physiol. 191, 139–146 (2007).
Catoire, M., Mensink, M., Kalkhoven, E., Schrauwen, P. & Kersten, S. Identification of human exercise-induced myokines using secretome analysis. Physiol. Genomics 46, 256–267 (2014).
Wong, B. W. C., Wong, D. & McManus, B. M. Characterization of fractalkine (CX3CL1) and CX3CR1 in human coronary arteries with native atherosclerosis, diabetes mellitus, and transplant vascular disease. Cardiovasc. Pathol. 11, 332–338 (2002).
Keihanian, A., Arazi, H. & Kargarfard, M. Effects of aerobic versus resistance training on serum fetuin-A, fetuin-B, and fibroblast growth factor-21 levels in male diabetic patients. Physiol. Int. 106, 70–80 (2019).
He, Z. et al. Myokine response to high-intensity interval vs. resistance exercise: an individual approach. Front. Physiol. 9, 1735 (2018).
Nieman, D. C. et al. Cytokine changes after a marathon race. J. Appl. Physiol. 91, 109–114 (2001).
Otaka, N. et al. Myonectin is an exercise-induced myokine that protects the heart from ischemia-reperfusion injury. Circ. Res. 123, 1326–1338 (2018).
Fabel, K. et al. VEGF is necessary for exercise-induced adult hippocampal neurogenesis. Eur. J. Neurosci. 18, 2803–2812 (2003).
Kim, K. H. et al. Acute exercise induces FGF21 expression in mice and in healthy humans. PLoS ONE 8, e63517 (2013).
Pedersen, B. K. & Febbraio, M. A. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
Catoire, M. et al. Fatty acid-inducible ANGPTL4 governs lipid metabolic response to exercise. Proc. Natl Acad. Sci. USA 111, E1043–E1052 (2014).
Laurens, C. et al. Growth and differentiation factor 15 is secreted by skeletal muscle during exercise and promotes lipolysis in humans. JCI Insight 5, e131870 (2020).
Wedell-Neergaard, A.-S. et al. Exercise-induced changes in visceral adipose tissue mass are regulated by IL-6 signaling: a randomized controlled trial. Cell Metab. 29, 844–855.e3 (2019).
Little, H. C. et al. Myonectin deletion promotes adipose fat storage and reduces liver steatosis. FASEB J. 33, 8666–8687 (2019).
Becher, T. et al. Brown adipose tissue is associated with cardiometabolic health. Nat. Med. 27, 58–65 (2021).
Boström, P. et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481, 463–468 (2012). The first paper to describe irisin, a PGC1α-dependent myokine, that drives ‘browning’ of WAT in an animal model; the extent to which these results might apply to humans remains under investigation.
Terada, S. et al. Effects of low-intensity prolonged exercise on PGC-1 mRNA expression in rat epitrochlearis muscle. Biochem. Biophys. Res. Commun. 296, 350–354 (2002).
Pilegaard, H., Saltin, B. & Neufer, P. D. Exercise induces transient transcriptional activation of the PGC-1α gene in human skeletal muscle. J. Physiol. 546, 851–858 (2003).
Fox, J. et al. Effect of an acute exercise bout on immediate post-exercise irisin concentration in adults: a meta-analysis. Scand. J. Med. Sci. Sports 28, 16–28 (2018).
Qiu, S. et al. Chronic exercise training and circulating irisin in adults: a meta-analysis. Sports Med. 45, 1577–1588 (2015).
Vosselman, M. J. et al. Low brown adipose tissue activity in endurance-trained compared with lean sedentary men. Int. J. Obes. 39, 1696–1702 (2015).
Tsiloulis, T. et al. No evidence of white adipocyte browning after endurance exercise training in obese men. Int. J. Obes. 42, 721–727 (2017).
Stanford, K. I. et al. 12,13-diHOME: an exercise-induced lipokine that increases skeletal muscle fatty acid uptake. Cell Metab. 27, 1357–1357 (2018). This paper demonstrated that levels of a lipokine produced from brown adipose tissue increase with acute and chronic training to affect white adipose tissue lipolysis.
Vasan, S. K. et al. The proposed systemic thermogenic metabolites succinate and 12,13-diHOME are inversely associated with adiposity and related metabolic traits: evidence from a large human cross-sectional study. Diabetologia 62, 2079–2087 (2019).
Pinckard, K. M. et al. A novel endocrine role for the BAT-released lipokine 12,13-diHOME to mediate cardiac function. Circulation 143, 145–159 (2021).
Besse-Patin, A. et al. Effect of endurance training on skeletal muscle myokine expression in obese men: identification of apelin as a novel myokine. Int. J. Obes. 38, 707–713 (2014).
Kwak, S. E. et al. Effects of exercise-induced apelin on muscle function and cognitive function in aged mice. Exp. Gerontol. 127, 110710 (2019).
Vinel, C. et al. The exerkine apelin reverses age-associated sarcopenia. Nat. Med. 24, 1360–1371 (2018).
Sargeant, J. A. et al. The influence of adiposity and acute exercise on circulating hepatokines in normal-weight and overweight/obese men. Appl. Physiol. Nutr. Metab. 43, 482–490 (2018).
Seo, M. W. et al. Effects of 16 weeks of resistance training on muscle quality and muscle growth factors in older adult women with sarcopenia: a randomized controlled trial. Int. J. Env. Res. Public Health 18, 6762 (2021).
Domin, R. et al. Effect of various exercise regimens on selected exercise-induced cytokines in healthy people. Int. J. Env. Res. Public Health 18, 1261 (2021).
Peppler, W. T. et al. Regulation of hepatic follistatin expression at rest and during exercise in mice. Med. Sci. Sports Exerc. 51, 1116–1125 (2019).
Malin, S. K., del Rincon, J. P., Huang, H. & Kirwan, J. P. Exercise-induced lowering of fetuin-A may increase hepatic insulin sensitivity. Med. Sci. Sports Exerc. 46, 2085–2090 (2014).
Haugen, F. et al. IL-7 is expressed and secreted by human skeletal muscle cells. Am. J. Physiol. Cell Physiol. 298, C807–C816 (2010).
Broholm, C. et al. LIF is a contraction-induced myokine stimulating human myocyte proliferation. J. Appl. Physiol. 111, 251–259 (2011).
Rønning, S. B. et al. Syndecan-4 regulates muscle differentiation and is internalized from the plasma membrane during myogenesis. PLoS One 10, e0129288 (2015).
Takahashi, H., Kotani, K., Tanaka, K., Egucih, Y. & Anzai, K. Therapeutic approaches to nonalcoholic fatty liver disease: exercise intervention and related mechanisms. Front. Endocrinol. 9, 588 (2018).
Keipert, S. et al. Skeletal muscle mitochondrial uncoupling drives endocrine cross-talk through the induction of FGF21 as a myokine. Am. J. Physiol. Endocrinol. Metab. 306, E469–E482 (2014).
Febbraio, M. A. et al. Exercise induces hepatosplanchnic release of heat shock protein 72 in humans. J. Physiol. 544, 957–962 (2002). Using sophisticated arterial-venous sampling techniques, this paper demonstrated that the splanchnic tissue bed, rather than the muscle, releases HSP72 during acute exercise in humans.
Mailing, L. J., Allen, J. M., Buford, T. W., Fields, C. J. & Woods, J. A. Exercise and the gut microbiome: a review of the evidence, potential mechanisms, and implications for human health. Exerc. Sport. Sci. Rev. 47, 75–85 (2019).
Allen, J. M. et al. Exercise alters gut microbiota composition and function in lean and obese humans. Med. Sci. Sports Exerc. 50, 747–757 (2018).
Packer, N. & Hoffman-Goetz, L. Exercise training reduces inflammatory mediators in the intestinal tract of healthy older adult mice. Can. J. Aging 31, 161–171 (2012).
van Wijck, K. et al. Exercise-induced splanchnic hypoperfusion results in gut dysfunction in healthy men. PLoS ONE 6, e22366 (2011).
Meissner, M. et al. Voluntary wheel running increases bile acid as well as cholesterol excretion and decreases atherosclerosis in hypercholesterolemic mice. Atherosclerosis 218, 323–329 (2011).
Jung, T. W. et al. BAIBA attenuates insulin resistance and inflammation induced by palmitate or a high fat diet via an AMPK–PPARδ-dependent pathway in mice. Diabetologia 58, 2096–2105 (2015).
Lee, Y. S. et al. The fractalkine/CX3CR1 system regulates β cell function and insulin secretion. Cell 153, 413–425 (2013).
Gerst, F. et al. Metabolic crosstalk between fatty pancreas and fatty liver: effects on local inflammation and insulin secretion. Diabetologia 60, 2240–2251 (2017).
Tao, R. et al. Inactivating hepatic follistatin alleviates hyperglycemia. Nat. Med. 24, 1058–1069 (2018).
Zhang, D., Xie, T. & Leung, P. S. Irisin ameliorates glucolipotoxicity-associated β-cell dysfunction and apoptosis via AMPK signaling and anti-inflammatory actions. Cell Physiol. Biochem. 51, 924–937 (2018).
Lang Lehrskov, L. et al. Interleukin-6 delays gastric emptying in humans with direct effects on glycemic control. Cell Metab. 27, 1201–1211.e3 (2018).
Ellingsgaard, H. et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat. Med. 17, 1481–1489 (2011).
Carey, A. L. et al. Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes 55, 2688–2697 (2006).
van Hall, G. et al. Interleukin-6 stimulates lipolysis and fat oxidation in humans. J. Clin. Endocrinol. Metab. 88, 3005–3010 (2003).
Benatti, F. B. & Pedersen, B. K. Exercise as an anti-inflammatory therapy for rheumatic diseases–myokine regulation. Nat. Rev. Rheumatol. 11, 86–97 (2015).
Pedersen, L. et al. Voluntary running suppresses tumor growth through epinephrine- and IL-6-dependent NK cell mobilization and redistribution. Cell Metab. 23, 554–562 (2016).
Pedersen, B. K. & Toft, A. D. Effects of exercise on lymphocytes and cytokines. Br. J. Sports Med. 34, 246–251 (2000).
Steensberg, A., Fischer, C. P., Keller, C., Møller, K. & Pedersen, B. K. IL-6 enhances plasma IL-1ra, IL-10, and cortisol in humans. Am. J. Physiol. Endocrinol. Metab. 285, E433–E437 (2003).
Dinarello, C. A. The interleukin-1 family: 10 years of discovery. FASEB J. 8, 1314–1325 (1994).
de Waal Malefyt, R., Abrams, J., Bennett, B., Figdor, C. G. & de Vries, J. E. Interleukin 10 (IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytes. J. Exp. Med. 174, 1209–1220 (1991).
Starkie, R., Ostrowski, S. R., Jauffred, S., Febbraio, M. & Pedersen, B. K. Exercise and IL-6 infusion inhibit endotoxin-induced TNF-α production in humans. FASEB J. 17, 884–886 (2003). An important paper demonstrating that increasing IL-6 either by exercise or by infusion blunts the inflammatory effect of TNF.
Moore, S. C. et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern. Med. 176, 816–825 (2016).
Rundqvist, H. et al. Cytotoxic T-cells mediate exercise-induced reductions in tumor growth. eLife 9, e59996 (2020).
Matsuo, K. et al. A mechanism underlying preventive effect of high-intensity training on colon cancer. Med. Sci. Sports Exerc. 49, 1805–1816 (2017).
Aoi, W. et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut 62, 882–889 (2013).
Strömberg, A. et al. CX3CL1–a macrophage chemoattractant induced by a single bout of exercise in human skeletal muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 310, R297–R304 (2016).
Rao, R. R. et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell 157, 1279–1291 (2014).
Kang, K. et al. Adipocyte-derived Th2 cytokines and myeloid PPARδ regulate macrophage polarization and insulin sensitivity. Cell Metab. 7, 485–495 (2008).
Knudsen, N. H. et al. Interleukin-13 drives metabolic conditioning of muscle to endurance exercise. Science 368, eaat3987 (2020). This paper showed that type 2 innate lymphoid cells (ILC2s) in skeletal muscle secrete IL-13 to affect the metabolic adaptation to exercise training.
Brestoff, J. R. et al. Group 2 innate lymphoid cells promote beiging of white adipose tissue and limit obesity. Nature 519, 242–246 (2015).
Valenzuela, P. L. et al. Exercise benefits on Alzheimer’s disease: state-of-the-science. Ageing Res. Rev. 62, 101108 (2020).
Etnier, J. L., Shih, C.-H. & Piepmeier, A. T. in Exercise-Cognition Interaction (ed. McMorris, T.) 29–42 (Academic Press, 2016).
Voss, M. W. et al. Exercise and hippocampal memory systems. Trends Cogn. Sci. 23, 318–333 (2019).
Etnier, J. L. et al. The influence of physical fitness and exercise upon cognitive functioning: a meta-analysis. J. Sport. Exerc. Psychol. 19, 249–277 (1997).
Colcombe, S. & Kramer, A. F. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol. Sci. 14, 125–130 (2003).
Neylan, T. C. Memory and the medial temporal lobe. J. Neuropsychiatry Clin. Neurosci. 12, 103 (2000).
Erickson, K. I. et al. Exercise training increases size of hippocampus and improves memory. Proc. Natl Acad. Sci. USA 108, 3017–3022 (2011). This was a randomized controlled trial in older adults that showed that chronic exercise training increases hippocampal size and improves memory function.
Gaitán, J. M. et al. Effects of aerobic exercise training on systemic biomarkers and cognition in late middle-aged adults at risk for Alzheimer’s disease. Front. Endocrinol. 12, 660181 (2021).
Liu, P. Z. & Nusslock, R. Exercise-mediated neurogenesis in the hippocampus via BDNF. Front. Neurosci. 12, 52 (2018).
Vivar, C. & van Praag, H. Running changes the brain: the long and the short of it. Physiology 32, 410–424 (2017).
Horowitz, A. M. et al. Blood factors transfer beneficial effects of exercise on neurogenesis and cognition to the aged brain. Science 369, 167–173 (2020). This paper demonstrated that transfer of plasma from exercised aged mice to sedentary aged mice can confer benefits on the ageing brain, including improvements in cognitive function.
De Miguel, Z. et al. Exercise plasma boosts memory and dampens brain inflammation via clusterin. Nature 600, 494–499 (2021). This paper demonstrated that plasma transfer from exercised young mice to sedentary young mice reduces brain inflammation and improves cognitive function, supporting the potential of transferable anti-inflammatory exerkines in improving brain function.
Agudelo, L. Z. et al. Skeletal muscle PGC-1α1 modulates kynurenine metabolism and mediates resilience to stress-induced depression. Cell 159, 33–45 (2014).
Yau, S. Y. et al. Physical exercise-induced hippocampal neurogenesis and antidepressant effects are mediated by the adipocyte hormone adiponectin. Proc. Natl Acad. Sci. USA 111, 15810–15815 (2014).
Wrann, C. D. et al. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 18, 649–659 (2013).
Fu, Y. C., Luo, N. L., Klein, R. L. & Garvey, W. T. Adiponectin promotes adipocyte differentiation, insulin sensitivity, and lipid accumulation. J. Lipid Res. 46, 1369–1379 (2005).
Schön, M. et al. Effects of running on adiponectin, insulin and cytokines in cerebrospinal fluid in healthy young individuals. Sci. Rep. 9, 1959 (2019).
Lourenco, M. V. et al. Exercise-linked FNDC5/irisin rescues synaptic plasticity and memory defects in Alzheimer’s models. Nat. Med. 25, 165–175 (2019).
Islam, M. R. et al. Exercise hormone irisin is a critical regulator of cognitive function. Nat. Metab. 3, 1058–1070 (2021).
Moon, H. Y. et al. Running-induced systemic cathepsin B secretion is associated with memory function. Cell Metab. 24, 332–340 (2016).
Naito, A. T. et al. Complement C1q activates canonical Wnt signaling and promotes aging-related phenotypes. Cell 149, 1298–1313 (2012).
Baker, S. K. et al. Blood-derived plasminogen drives brain inflammation and plaque deposition in a mouse model of Alzheimer’s disease. Proc. Natl Acad. Sci. USA 115, E9687–E9696 (2018).
Heinonen, A. et al. Bone mineral density of female athletes in different sports. Bone Min. 23, 1–14 (1993).
Bergmann, P. et al. Loading and skeletal development and maintenance. J. Osteoporos. 2011, 786752 (2010).
Janssens, K., ten Dijke, P., Janssens, S. & Van Hul, W. Transforming growth factor-β1 to the bone. Endocr. Rev. 26, 743–774 (2005).
Amrein, K. et al. Sclerostin and its association with physical activity, age, gender, body composition, and bone mineral content in healthy adults. J. Clin. Endocrinol. Metab. 97, 148–154 (2012).
Silverman, S. L. Sclerostin. J. Osteoporos. 2010, 941419 (2010).
Li, G. et al. Muscle-bone crosstalk and potential therapies for sarco-osteoporosis. J. Cell Biochem. 120, 14262–14273 (2019).
Luo, J., Liu, W., Feng, F. & Chen, L. Apelin/APJ system: a novel therapeutic target for locomotor system diseases. Eur. J. Pharmacol. 906, 174286 (2021).
Kim, H. et al. Irisin mediates effects on bone and fat via αV integrin receptors. Cell 175, 1756–1768.e17 (2018).
Harmer, D., Falank, C. & Reagan, M. R. Interleukin-6 interweaves the bone marrow microenvironment, bone loss, and multiple myeloma. Front. Endocrinol. 9, 788 (2019).
Lynes, M. D. et al. The cold-induced lipokine 12,13-diHOME promotes fatty acid transport into brown adipose tissue. Nat. Med. 23, 631–637 (2017).
Neeper, S. A., Gómez-Pinilla, F., Choi, J. & Cotman, C. Exercise and brain neurotrophins. Nature 373, 109 (1995).
Matthews, V. B. et al. Brain-derived neurotrophic factor is produced by skeletal muscle cells in response to contraction and enhances fat oxidation via activation of AMP-activated protein kinase. Diabetologia 52, 1409–1418 (2009).
Lin, Z. et al. Adiponectin mediates the metabolic effects of FGF21 on glucose homeostasis and insulin sensitivity in mice. Cell Metab. 17, 779–789 (2013).
Chung, J. et al. HSP72 protects against obesity-induced insulin resistance. Proc. Natl Acad. Sci. USA 105, 1739–1744 (2008).
Fujimoto, T. et al. Overexpression of interleukin-15 exhibits improved glucose tolerance and promotes GLUT4 translocation via AMP-activated protein kinase pathway in skeletal muscle. Biochem. Biophys. Res. Commun. 509, 994–1000 (2019).
Willkomm, L. et al. Lactate regulates myogenesis in C2C12 myoblasts in vitro. Stem Cell Res. 12, 742–753 (2014).
Shimomura, M. et al. Decreased muscle-derived musclin by chronic resistance exercise is associated with improved insulin resistance in rats with type 2 diabetes. Physiol. Rep. 9, e14823 (2021).
Thomas, G. et al. Osteocrin, a novel bone-specific secreted protein that modulates the osteoblast phenotype. J. Biol. Chem. 278, 50563–50571 (2003).
Ataman, B. et al. Evolution of osteocrin as an activity-regulated factor in the primate brain. Nature 539, 242–247 (2016).
Palmer, R. M. J., Ferrige, A. G. & Moncada, S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327, 524–526 (1987). This paper described the vasodilatory role of nitric oxide.
Davies, K. J. A., Quintanilha, A. T., Brooks, G. A. & Packer, L. Free radicals and tissue damage produced by exercise. Biochem. Biophys. Res. Commun. 107, 1198–1205 (1982).
Aoi, W. et al. Secreted protein acidic and rich in cysteine (SPARC) improves glucose tolerance via AMP-activated protein kinase activation. FASEB J. 33, 10551–10562 (2019).
Li, Y. et al. Transforming growth factor-β1 induces the differentiation of myogenic cells into fibrotic cells in injured skeletal muscle: a key event in muscle fibrogenesis. Am. J. Pathol. 164, 1007–1019 (2004).
Hunt, L. C., Upadhyay, A., Jazayeri, J. A., Tudor, E. M. & White, J. D. An anti-inflammatory role for leukemia inhibitory factor receptor signaling in regenerating skeletal muscle. Histochem. Cell Biol. 139, 13–34 (2013).
Ito, Y. et al. Differential temporal expression of mRNAs for ciliary neurotrophic factor (CNTF), leukemia inhibitory factor (LIF), interleukin-6 (IL-6), and their receptors (CNTFRα, LIFRβ, IL-6Rα and gp130) in injured peripheral nerves. Brain Res. 793, 321–327 (1998).
Lee, S., Kolset, S. O., Birkeland, K. I., Drevon, C. A. & Reine, T. M. Acute exercise increases syndecan-1 and -4 serum concentrations. Glycoconj. J. 36, 113–125 (2019).
Bouassida, A. et al. Review on leptin and adiponectin responses and adaptations to acute and chronic exercise. Br. J. Sports Med. 44, 620–630 (2010).
Barlow, J. P. et al. Beta-aminoisobutyric acid is released by contracting human skeletal muscle and lowers insulin release from INS-1 832/3 cells by mediating mitochondrial energy metabolism. Metab. Open 7, 100053 (2020).
Lin, W., Zhang, T., Zhou, Y., Zheng, J. & Lin, Z. Advances in biological functions and clinical studies of FGF21. Diabetes Metab. Syndr. Obes. 14, 3281–3290 (2021).
Lee, S. J. & McPherron, A. C. Regulation of myostatin activity and muscle growth. Proc. Natl Acad. Sci. USA 98, 9306–9311 (2001).
Kleinert, M. et al. Exercise increases circulating GDF15 in humans. Mol. Metab. 9, 187–191 (2018).
Andersson, H. et al. Differences in the inflammatory plasma cytokine response following two elite female soccer games separated by a 72-h recovery. Scand. J. Med. Sci. Sports 20, 740–747 (2010).
Irving, B. A. et al. Combined training enhances skeletal muscle mitochondrial oxidative capacity independent of age. J. Clin. Endocrinol. Metab. 100, 1654–1663 (2015).
Bae, J. Y. Aerobic exercise increases meteorin-like protein in muscle and adipose tissue of chronic high-fat diet-induced obese mice. Biomed. Res. Int. 2018, 6283932 (2018).
Pourranjbar, M., Arabnejad, N., Naderipour, K. & Rafie, F. Effects of aerobic exercises on serum levels of myonectin and insulin resistance in obese and overweight women. J. Med. Life 11, 381–386 (2018).
Nishizawa, H. et al. Musclin, a novel skeletal muscle-derived secretory factor. J. Biol. Chem. 279, 19391–19395 (2004).
Hjorth, M. et al. The effect of acute and long-term physical activity on extracellular matrix and serglycin in human skeletal muscle. Physiol. Rep. 3, e12473 (2015).
Gopal, S. Syndecans in Inflammation at a glance. Front. Immunol. 11, 227 (2020).
Breen, E. C. et al. Angiogenic growth factor mRNA responses in muscle to a single bout of exercise. J. Appl. Physiol. 81, 355–361 (1996). This paper demonstrated that a single bout of exercise can increase VEGF1 and TGFβ1 expression in muscle to promote the angiogenic response to exercise.
Smith, J. K., Dykes, R., Douglas, J. E., Krishnaswamy, G. & Berk, S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA 281, 1722–1727 (1999).
Klein, A. B. et al. Pharmacological but not physiological GDF15 suppresses feeding and the motivation to exercise. Nat. Commun. 12, 1041 (2021).
Boulé, N. G., Haddad, E., Kenny, G. P., Wells, G. A. & Sigal, R. J. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 286, 1218–1227 (2001).
Pandey, A. et al. Metabolic effects of exercise training among fitness-nonresponsive patients with type 2 diabetes: the HART-D study. Diabetes Care 38, 1494–1501 (2015).
Acknowledgements
The authors thank A. Honkala (Stanford University) and N. C. Oldenburg (University of Minnesota) for their assistance with the manuscript. The workshop that set the foundation for this Review article was supported by the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health (NIH). The listed authors acknowledge the support of the following grants. L.S.C.: NIH grant R01DK098203; B.H.G.: NIH grant U01AR071133; A.L.: Spanish Ministry of Economy and Competitiveness and Fondos FEDER (PI18/00139); C.M.: European Federation of the Study of Diabetes/MSD, Occitanie Region/FEDER funds (DIABKINES, MP0021755 and Enterosys); B.K.P.: TrygFonden for the Centre for PA Research (CFAS); A.P.: Texas Health Resources Clinical Scholarship, Gilead Sciences Research Scholar Program, NIH National Institute of Aging GEMSSTAR grant (1R03AG067960-01), and Applied Therapeutics; J.M.R.: NIH grant HL150327-01A1; H.v.P.: NIH National Institute on Aging (NIA)/NIH IRP and the FDOH Ed and Ethel Moore Alzheimer’s Disease Research program; K.I.S.: NIH grants R01-HL138738 and R01-AG060542; A.E.T.: National Institute for Health Research (NIHR) Leicester Biomedical Research Centre; J.M.T.: NIH grant 1R01HL142879; S.T.: NIH grants U01AR071133; J.R.Z.: Swedish Research Council for Sport Science (P2018-0097), Swedish Research Council (Vetenskapsrådet) (2015-00165), and Novo Nordisk Foundation Center for Basic Metabolic Research at the University of Copenhagen (NNF18CC0034900); M.P.S.: NIH grants U24DK112348 and U54DK102556. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
L.S.C. has received a Dexcom investigator initiated grant (product only). C.J.L. is a consultant for PAIhealth on their Personalized Activity Intelligence applications. A.P. is on the advisory board of Roche Diagnostics. M.P.S. is a cofounder and scientific advisory board member of Personalis, SensOmics, Qbio, January, Filtricine, Protos, NiMo, Mirvie, and an advisor for Genapsys. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks P. Atherton who co-reviewed the manuscript with D. Wilkinson, M. Fukui and E. Ziemann for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Molecular Transducers of Physical Activity Consortium: https://www.motrpac.org/
Resilience: https://ods.od.nih.gov/Research/resilience.aspx#defining
Supplementary information
Glossary
- Resilience
-
Resilience is the ability of the body to resist, adapt to, recover or grow in response to stressors.
- High-intensity interval training
-
High-intensity interval training is a form of exercise training characterized by bursts of high-intensity activity followed by less intense recovery periods.
- Exerkines
-
Exerkines encompass a broad variety of signalling moieties that are released in response to acute and/or chronic exercise that exert their effects through endocrine, paracrine and/or autocrine pathways.
- Acute exercise
-
Acute exercise is typically considered a single episode of exercise (often resistant or aerobic exercise) that is completed during one visit.
- Chronic exercise
-
Chronic exercise is typically described as multiple exercise episodes (often resistant or aerobic exercise) performed over the course of weeks to months.
- MicroRNA
-
MicroRNAs are non-protein-coding RNA molecules that are regulated in a transcriptional or post-transcriptional fashion to affect mRNA transcription and/or degradation.
- Exosomes
-
Exosomes are a type of extracellular vesicle released by parent cells, which contain RNAs, proteins and lipids, to facilitate crosstalk between tissues.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chow, L.S., Gerszten, R.E., Taylor, J.M. et al. Exerkines in health, resilience and disease. Nat Rev Endocrinol 18, 273–289 (2022). https://doi.org/10.1038/s41574-022-00641-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-022-00641-2
This article is cited by
-
Advances in secondary prevention mechanisms of macrovascular complications in type 2 diabetes mellitus patients: a comprehensive review
European Journal of Medical Research (2024)
-
The effect of physical exercise on anticancer immunity
Nature Reviews Immunology (2024)
-
Exerkines and cardiometabolic benefits of exercise: from bench to clinic
EMBO Molecular Medicine (2024)
-
Cardiometabolic profiles and proteomics associated with obesity phenotypes in a longitudinal cohort of young adults
Scientific Reports (2024)
-
Inter-organ crosstalk during development and progression of type 2 diabetes mellitus
Nature Reviews Endocrinology (2024)