Abstract
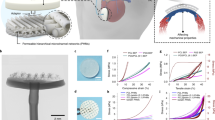
Acellular epicardial patches that treat myocardial infarction by increasing the mechanical integrity of damaged left ventricular tissues exhibit widely scattered therapeutic efficacy. Here, we introduce a viscoelastic adhesive patch, made of an ionically crosslinked transparent hydrogel, that accommodates the cyclic deformation of the myocardium and outperforms most existing acellular epicardial patches in reversing left ventricular remodelling and restoring heart function after both acute and subacute myocardial infarction in rats. The superior performance of the patch results from its relatively low dynamic modulus, designed at the so-called ‘gel point’ via finite-element simulations of left ventricular remodelling so as to balance the fluid and solid properties of the material.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information files. Source data for the figures are available from the corresponding authors upon reasonable request. The RNA sequence data have been deposited in the National Center for Biotechnology Information Sequence Read Archive, with accession code SRP187341.
Code availability
The FEBio code is available upon reasonable request.
References
Rane, A. A. & Christman, K. L. Biomaterials for the treatment of myocardial infarction: a 5-year update. J. Am. Coll. Cardiol. 58, 2615–2629 (2011).
Laflamme, M. A. & Murry, C. E. Heart regeneration. Nature 473, 326–335 (2011).
Wei, K. et al. Epicardial FSTL1 reconstitution regenerates the adult mammalian heart. Nature 525, 479–485 (2015).
Shadrin, I. Y. et al. Cardiopatch platform enables maturation and scale-up of human pluripotent stem cell-derived engineered heart tissues. Nat. Commun. 8, 1825 (2017).
Fujimoto, K. L. et al. An elastic, biodegradable cardiac patch induces contractile smooth muscle and improves cardiac remodeling and function in subacute myocardial infarction. J. Am. Coll. Cardiol. 49, 2292–2300 (2007).
Didie, M. et al. Parthenogenetic stem cells for tissue-engineered heart repair. J. Clin. Invest. 123, 1285–1298 (2013).
Liao, S.-Y. et al. Attenuation of left ventricular adverse remodeling with epicardial patching after myocardial infarction. J. Card. Fail. 16, 590–598 (2010).
Stuckey, D. J. et al. Magnetic resonance imaging evaluation of remodeling by cardiac elastomeric tissue scaffold biomaterials in a rat model of myocardial infarction. Tissue Eng. Part A 16, 3395–3402 (2010).
Fujimoto, K. L. et al. Placement of an elastic biodegradable cardiac patch on a subacute infarcted heart leads to cellularization with early developmental cardiomyocyte characteristics. J. Card. Fail. 18, 585–595 (2012).
Chi, N.-H., Yang, M.-C., Chung, T.-W., Chou, N.-K. & Wang, S.-S. Cardiac repair using chitosan-hyaluronan/silk fibroin patches in a rat heart model with myocardial infarction. Carbohydr. Polym. 92, 591–597 (2013).
Serpooshan, V. et al. The effect of bioengineered acellular collagen patch on cardiac remodeling and ventricular function post myocardial infarction. Biomaterials 34, 9048–9055 (2013).
Vilaeti, A. D. et al. Short-term ventricular restraint attenuates post-infarction remodeling in rats. Int. J. Cardiol. 165, 278–284 (2013).
D’Amore, A. et al. Bi-layered polyurethane—extracellular matrix cardiac patch improves ischemic ventricular wall remodeling in a rat model. Biomaterials 107, 1–14 (2016).
Moainie, S. L. et al. Infarct restraint attenuates remodeling and reduces chronic ischemic mitral regurgitation after postero-lateral infarction. Ann. Thorac. Surg. 74, 444–449 (2002).
Fomovsky, G. M., Clark, S. A., Parker, K. M., Ailawadi, G. & Holmes, J. W. Anisotropic reinforcement of acute anteroapical infarcts improves pump function. Circ. Heart Fail. 5, 515–522 (2012).
Enomoto, Y. et al. Early ventricular restraint after myocardial infarction: extent of the wrap determines the outcome of remodeling. Ann. Thorac. Surg. 79, 881–887 (2005).
Clarke, S. A., Ghanta, R. K., Ailawadi, G. & Holmes, J. W. in Cardiovascular and Cardiac Therapeutic Devices (ed. Franz, T.) 169–206 (Springer Berlin Heidelberg, 2014).
Clarke, S. A., Goodman, N. C., Ailawadi, G. & Holmes, J. W. Effect of scar compaction on the therapeutic efficacy of anisotropic reinforcement following myocardial infarction in the dog. J. Cardiovasc. Transl. Res. 8, 353–361 (2015).
Piao, H. et al. Effects of cardiac patches engineered with bone marrow-derived mononuclear cells and PGCL scaffolds in a rat myocardial infarction model. Biomaterials 28, 641–649 (2007).
Sarig, U. et al. Natural myocardial ECM patch drives cardiac progenitor based restoration even after scarring. Acta Biomater. 44, 209–220 (2016).
Gu, X. et al. Sustained viral gene delivery from a micro-fibrous, elastomeric cardiac patch to the ischemic rat heart. Biomaterials 133, 132–143 (2017).
Mazza, E. & Ehret, A. E. Mechanical biocompatibility of highly deformable biomedical materials. J. Mech. Behav. Biomed. Mater. 48, 100–124 (2015).
Winter, H. H. & Chambon, F. Analysis of linear viscoelasticity of a crosslinking polymer at the gel point. J. Rheol. 30, 367–382 (1986).
Chambon, F. & Winter, H. H. Linear viscoelasticity at the gel point of a crosslinking PDMS with imbalanced stoichiometry. J. Rheol. 31, 683–697 (1987).
Zhang, Y. S. & Khademhosseini, A. Advances in engineering hydrogels. Science 356, eaaf3627 (2017).
Yuk, H., Zhang, T., Lin, S., Parada, G. A. & Zhao, X. Tough bonding of hydrogels to diverse non-porous surfaces. Nat. Mater. 15, 190–196 (2016).
Oz, M. C. et al. Global surgical experience with the acorn cardiac support device. J. Thorac. Cardiov. Sur. 126, 983–991 (2003).
Ghanta, R. K. et al. Adjustable, physiological ventricular restraint improves left ventricular mechanics and reduces dilatation in an ovine model of chronic heart failure. Circulation 115, 1201–1210 (2007).
Ende, N. Amylase activity in body fluids. Cancer 14, 1109–1114 (1961).
Omens, J. H., Mackenna, D. A. & Mcculloch, A. D. Measurement of strain and analysis of stress in resting rat left-ventricular myocardium. J. Biomech. 26, 665–676 (1993).
Lin, Y. D. et al. A nanopatterned cell-seeded cardiac patch prevents electro-uncoupling and improves the therapeutic efficacy of cardiac repair. Biomater. Sci. 2, 567–580 (2014).
Kutschka, I. et al. Collagen matrices enhance survival of transplanted cardiomyoblasts and contribute to functional improvement of ischemic rat hearts. Circulation 114, I167–I173 (2006).
Simpson, D., Liu, H., Fan, T. H., Nerem, R. & Dudley, S. C. Jr. A tissue engineering approach to progenitor cell delivery results in significant cell engraftment and improved myocardial remodeling. Stem Cells 25, 2350–2357 (2007).
Liang, S. et al. Paintable and rapidly bondable conductive hydrogels as therapeutic cardiac patches. Adv. Mater. 30, e1704235 (2018).
Efraim, Y. et al. Biohybrid cardiac ECM-based hydrogels improve long term cardiac function post myocardial infarction. Acta Biomater. 50, 220–233 (2017).
Ravi, S. et al. Effect of bone marrow-derived extracellular matrix on cardiac function after ischemic injury. Biomaterials 33, 7736–7745 (2012).
Jin, J. et al. Transplantation of mesenchymal stem cells within a poly(lactide-co-ɛ-caprolactone) scaffold improves cardiac function in a rat myocardial infarction model. Eur. J. Heart Fail. 11, 147–153 (2009).
Giraud, M.-N. et al. Hydrogel-based engineered skeletal muscle grafts normalize heart function early after myocardial infarction. Artif. Organs 32, 692–700 (2008).
Siepe, M. et al. Myoblast-seeded biodegradable scaffolds to prevent post-myocardial infarction evolution toward heart failure. J. Thorac. Cardiovasc. Sur. 132, 124–131 (2006).
Hashizume, R. et al. The effect of polymer degradation time on functional outcomes of temporary elastic patch support in ischemic cardiomyopathy. Biomaterials 34, 7353–7363 (2013).
Mewhort, H. E. M. et al. Bioactive extracellular matrix scaffold promotes adaptive cardiac remodeling and repair. JACC Basic Transl. Sci. 2, 450–464 (2017).
Singelyn, J. M. et al. Catheter-deliverable hydrogel derived from decellularized ventricular extracellular matrix increases endogenous cardiomyocytes and preserves cardiac function post-myocardial infarction. J. Am. Coll. Cardiol. 59, 751–763 (2012).
Dai, W. et al. Intramyocardial injection of heart tissue-derived extracellular matrix improves postinfarction cardiac function in rats. J. Cardiovasc. Pharmacol. Ther. 18, 270–279 (2013).
Hassaballah, A. I., Hassan, M. A., Mardi, A. N. & Hamdi, M. An inverse finite element method for determining the tissue compressibility of human left ventricular wall during the cardiac cycle. PLoS ONE 8, e82703 (2013).
Wang, H. M. et al. Structure-based finite strain modelling of the human left ventricle in diastole. Int. J. Numer. Meth. Bio. 29, 83–103 (2013).
Eriksson, T. S. E., Prassl, A. J., Plank, G. & Holzapfel, G. A. Influence of myocardial fiber/sheet orientations on left ventricular mechanical contraction. Math. Mech. Solids 18, 592–606 (2013).
Gao, H., Carrick, D., Berry, C., Griffith, B. E. & Luo, X. Y. Dynamic finite-strain modelling of the human left ventricle in health and disease using an immersed boundary-finite element method. IMA J. Appl. Math. 79, 978–1010 (2014).
Hall, J. E. Guyton and Hall Textbook of Medical Physiology (Elsevier Health Sciences, 2015).
Mielniczuk, L. M. et al. Left ventricular end-diastolic pressure and risk of subsequent heart failure in patients following an acute myocardial infarction. Congest. Heart Fail. 13, 209–214 (2007).
Holzapfel, G. A. & Ogden, R. W. Constitutive modelling of passive myocardium: a structurally based framework for material characterization. Phil. Trans. R. Soc. A 367, 3445–3475 (2009).
Guccione, J. M. & Mcculloch, A. D. Mechanics of active contraction in cardiac-muscle. 1. Constitutive relations for fiber stress that describe deactivation. J. Biomech. Eng. Trans. ASME 115, 72–81 (1993).
Guccione, J. M., Waldman, L. K. & Mcculloch, A. D. Mechanics of active contraction in cardiac-muscle. 2. Cylindrical models of the systolic left-ventricle. J. Biomech. Eng. Trans. ASME 115, 82–90 (1993).
Rodriguez, E. K., Omens, J. H., Waldman, L. K. & Mcculloch, A. D. Effect of residual stress on transmural sarcomere length distributions in rat left ventricle. Am. J. Physiol. 264, H1048–H1056 (1993).
Walker, J. C. et al. Magnetic resonance imaging-based finite element stress analysis after linear repair of left ventricular aneurysm. J. Thorac. Cardiov. Sur. 135, 1094–1102 (2008).
Goktepe, S., Abilez, O. J. & Kuhl, E. A generic approach towards finite growth with examples of athlete’s heart, cardiac dilation, and cardiac wall thickening. J. Mech. Phys. Solids 58, 1661–1680 (2010).
Himpel, G., Kuhl, E., Menzel, A. & Steinmann, P. Computational modelling of isotropic multiplicative growth. CMES Comp. Model. Eng. Sci. 8, 119–134 (2005).
Genet, M., Lee, L. C., Baillargeon, B., Guccione, J. M. & Kuhl, E. Modeling pathologies of diastolic and systolic heart failure. Ann. Biomed. Eng. 44, 112–127 (2016).
Puso, M. A. & Weiss, J. A. Finite element implementation of anisotropic quasi-linear viscoelasticity using a discrete spectrum approximation. J. Biomech. Eng. Trans. ASME 120, 62–70 (1998).
Maas, S. A., Ellis, B. J., Ateshian, G. A. & Weiss, J. A. FEBio: finite elements for biomechanics. J. Biomech. Eng. Trans. ASME 134, 011005 (2012).
Tsai, J. Z. et al. In-vivo measurement of swine myocardial resistivity. IEEE Trans. Biomed. Eng. 49, 472–483 (2002).
Gabriel, C., Peyman, A. & Grant, E. H. Electrical conductivity of tissue at frequencies below 1 MHz. Phys. Med. Biol. 54, 4863–4878 (2009).
Li, J. et al. Tough adhesives for diverse wet surfaces. Science 357, 378–381 (2017).
Mehdizadeh, M., Weng, H., Gyawali, D., Tang, L. P. & Yang, J. Injectable citrate-based mussel-inspired tissue bioadhesives with high wet strength for sutureless wound closure. Biomaterials 33, 7972–7983 (2012).
Guo, J. S. et al. Click chemistry improved wet adhesion strength of mussel-inspired citrate-based antimicrobial bioadhesives. Biomaterials 112, 275–286 (2017).
Jeon, E. Y. et al. Rapidly light-activated surgical protein glue inspired by mussel adhesion and insect structural crosslinking. Biomaterials 67, 11–19 (2015).
Acknowledgements
We thank Y. Guan, A. J. Clasky and Y. Mao for material fabrication and characterization assistance, G. A. Holzapfel for discussions on the modelling methods, Y. Zhao for artwork, J. Wu for assistance with haemodynamics measurements, and C. Liu and H. Chen for assistance with rat surgery and echocardiology measurements. This work has been supported by the National Natural Science Foundation of China (81622032 and 51672184 to L.Y., 31571527 to N.S. and 81501858 to X.L.), National Science Foundation (CMMI-1562904 to H.G.), Jiangsu Innovation and Entrepreneurship Program (to L.Y.), National Key R&D Program of China (2016YFC1000500 and 2016YFC1305100 to N.S., and 2014CB748600 to L.Y.), Science and Technology Commission of Shanghai Municipality (numbers 17XD1400300 and 17JC1400200 to N.S.) and Priority Academic Program Development of Jiangsu Higher Education Institutions (to L.Y.).
Author information
Authors and Affiliations
Contributions
L.Y., N.S. and H.G. conceived and designed the study, analysed the data and provided funding. X.L., Y.B. and H.Y. carried out preparation and characterization of the GPAP, in vitro evaluation and data analysis. Y.L. performed the simulation work. A.B., H.C., W.J. and X.W. carried out the GPAP experiments for MI in rats, transcriptomic study and data collection. All authors wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary methods, discussion, figures, tables, references and video captions.
Supplementary Video 1
Stretching of GPAP with a tweezer.
Supplementary Video 2
Demonstration of patching GPAP onto a rat heart.
Supplementary Video 3
Injection of GPAP through a syringe needle with an inner diameter of 1.2 mm.
Rights and permissions
About this article
Cite this article
Lin, X., Liu, Y., Bai, A. et al. A viscoelastic adhesive epicardial patch for treating myocardial infarction. Nat Biomed Eng 3, 632–643 (2019). https://doi.org/10.1038/s41551-019-0380-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-019-0380-9
This article is cited by
-
Self-compliant ionic skin by leveraging hierarchical hydrogen bond association
Nature Communications (2024)
-
Nano-frictional mechano-reinforcing porous nanowires scaffolds
Friction (2024)
-
Study on viscoelasticity and damping properties of OSA/PAAM hydrogel
Journal of Polymer Research (2024)
-
Monolithic-to-focal evolving biointerfaces in tissue regeneration and bioelectronics
Nature Chemical Engineering (2024)
-
Chronological adhesive cardiac patch for synchronous mechanophysiological monitoring and electrocoupling therapy
Nature Communications (2023)