Abstract
Historically, International Space Station (ISS) exercise countermeasures have not fully protected astronauts’ musculoskeletal and cardiorespiratory fitness. Although these losses have been reduced on more recent missions, decreasing the time required to perform in-flight exercise would permit reallocation of that time to other tasks. To evaluate the effectiveness of a new training prescription, ISS crewmembers performed either the high intensity/lower volume integrated Sprint resistance (3 d wk−1) and aerobic (interval and continuous workouts, each 3 d wk−1 in alternating fashion) exercise program (n = 9: 8M/1F, 48 ± 7 y, 178 ± 5 cm, 77.7 ± 12.0 kg) or the standard ISS countermeasure consisting of daily resistance and aerobic exercise (n = 17: 14M/3F, 46 ± 6 y, 176 ± 6 cm, 80.6 ± 10.5 kg) during long-duration spaceflight. Bone mineral density (dual energy X-ray absorptiometry (DXA)), muscle strength (isokinetic dynamometry), muscle function (cone agility test), and cardiorespiratory fitness (VO2peak) were assessed pre- and postflight. Mixed-effects modeling was used to analyze dependent measures with alpha set at P < 0.05. After spaceflight, femoral neck bone mineral density (−1.7%), knee extensor peak torque (−5.8%), cone agility test time (+7.4%), and VO2peak (−6.1%) were decreased in both groups (simple main effects of time, all P < 0.05) with a few group × time interaction effects detected for which Sprint experienced either attenuated or no loss compared to control. Although physiologic outcomes were not appreciably different between the two exercise programs, to conserve time and optimally prepare crewmembers for the performance of physically demanding mission tasks, high intensity/lower volume training should be an indispensable component of spaceflight exercise countermeasure prescriptions.
Similar content being viewed by others
Introduction
Exercise countermeasures are employed during spaceflight to combat the deleterious physiologic effects of long-duration microgravity exposure. Early exercise hardware on the International Space Station (ISS) was limited to low running velocities (treadmill with vibration isolation system, TVIS: ~11.3 km h−1 peak permitted velocity) and low loads (interim resistive exercise device, iRED: 136 kg peak load), making a low intensity/high volume exercise program the default prescription1. Despite the near-daily performance of this program, multisystem deconditioning was evident including decrements in muscle mass, strength, and function2,3,4,5, cardiorespiratory fitness6, and bone mineral density7,8.
The effectiveness of high intensity/low volume training (HIT) has been extensively documented in populations ranging from elite athletes9 to clinical patients10,11. In addition to the time savings of shorter exercise sessions, there is evidence to suggest that HIT may elicit superior physiologic adaptations compared to traditional lower intensity/higher volume training. For instance, over a 6-week period (5 d wk−1), Tabata et al.12 compared 60 min bouts of continuous exercise (70% VO2peak) to 7–8 intervals (20 s at 170% VO2peak/10 s rest). Despite cumulative exercise time of only ~2 h compared to 30 h for the continuous group, the HIT group increased both aerobic and anaerobic capacity whereas the continuous, high volume group only improved aerobic capacity. Somewhat longer-duration intervals of 2–4 min have been shown to maintain or improve aerobic capacity during bed rest unloading13,14 and athletic training9. High intensity training also has been employed in resistance exercise and elicits superior increases in muscle mass15 and strength compared to lower intensities with equivalent volume load15.
To facilitate higher intensity aerobic and resistance exercise, the original suite of ISS exercise hardware was replaced in 2009 with a second-generation treadmill (T2: 19.3 km h−1 peak velocity) and the advanced resistive exercise device (ARED: 272 kg peak load)16. However, power issues initially limited T2’s peak velocity to 14.5 km h−1 17 and although crewmembers could lift heavier loads on ARED (up to 6-repetition maximum loads have been used based on crewmember capability and preference)1, they continued to perform both aerobic and resistance exercise 6 days per week. This approach consumed 9–10 h per week1,5, a significant time commitment that reduced crewmembers’ availability to perform other important mission tasks.
Thus, in light of the potential for similar, if not superior, physiologic protection coupled with meaningful time savings, the purpose of this investigation was to compare physiologic outcomes after ~6 months of long-duration spaceflight in crewmembers who performed exercise countermeasures consisting of either (1) lower intensity/higher volume exercise (6 d wk−1 resistance exercise and 6 d wk−1 aerobic exercise) or (2) high intensity/lower volume exercise (3 d wk−1 resistance exercise and 6 d wk−1 aerobic exercise). The study’s original hypothesis was that the experimental exercise protocol (Sprint) would better mitigate spaceflight-induced musculoskeletal and cardiorespiratory deconditioning compared to standard of care ISS exercise (Control). Over time, the culture surrounding high intensity exercise during spaceflight changed. Early successes with Sprint, lack of adverse effects, improved pre-flight cardiovascular risk screening, and other factors responsibly led to an evolution of the standard of care. This study is an exemplar of how research should transition to operations; this transition was likely accelerated by having operations colleagues on the research team. This rapid operational success story does pose a unique challenge to the scientific interpretation of the data; we readily acknowledge the complexity of this situation and the limitation of the evolving control group.
Results
Exercise training
SPRINT subjects effectively performed the aerobic exercise protocol as mean, peak heart rates for all intervals performed were >90% HRmax (Supplementary Table 1). Compared to CON, in-flight aerobic exercise volume for SPRINT was 29% and 7% lower on the cycle ergometer with vibration isolation system (CEVIS) and T2, respectively; total combined in-flight aerobic exercise volume was 17% lower for SPRINT. Aerobic exercise intensity was similar between CON and SPRINT for select interval and continuous workouts that each group performed. In-flight resistance exercise average loads for squat, heel raise, and deadlift were 6–15% higher in SPRINT while repetitions per week were 41–46% less for SPRINT. Total weekly resistance exercise volume load (sets × repetitions × load) was 34–44% lower for SPRINT (Supplementary Table 2).
Bone mineral density
Bone mineral density of the lumbar spine, pelvis, total hip, trochanter, femoral neck, and calcaneus were reduced after spaceflight (simple main effect for time, P < 0.05; Table 1). No group × time interactions were detected.
Muscle mass
Leg lean mass was unchanged after spaceflight (simple main effect for time, P = 0.40; Table 1) and there was no group × time interaction (P = 0.88; Table 1). Leg fat mass was decreased after spaceflight (simple main effect for time, P = 0.001; Table 1) but there was no group × time interaction.
Muscle strength
At the first post-flight test (R + 5), all tested isokinetic peak torque and total work variables were decreased (simple main effect for time, P < 0.05; Table 2). On R + 14, this reduction persisted for all variables (simple main effect for time, P < 0.05; Table 2) except eccentric ankle plantar flexor peak torque (P = 0.06; Table 2). At R + 30 testing, only knee extensor and flexor peak torque and knee flexor total work still differed significantly from preflight baseline (simple main effect for time, P < 0.05; Table 2). Group × time interaction effects were present for knee flexor peak torque (R + 5, R + 14, and R + 30, each P < 0.05; Table 2) and trunk extensor peak torque (R + 14, P = 0.01; Table 2); for these interactions, reductions in strength were absent or attenuated in SPRINT.
Muscle function
Leg press 1RM was unchanged after spaceflight (R + 7, simple main effect for time, P > 0.05; Table 3); at R + 30, strength was significantly greater than preflight baseline (simple main effect for time, P = 0.04; Table 3). Bench press 1RM was increased from preflight at both R + 7 and R + 30 (simple main effects for time, P < 0.05; Table 3). No interaction effects were detected for either 1RM test. Flexibility was decreased at R + 7 (simple main effect for time, P < 0.01; Table 3); a group × time interaction effect was also present with CON losing flexibility to a greater extent than SPRINT (P = 0.01; Table 3). Time to complete the cone test was increased at R + 7 (simple main effect for time, P < 0.01; Table 3); a trend for a group × time interaction effect was also present with CON tending to increase time to completion more than SPRINT (P = 0.07; Table 3).
Cardiorespiratory fitness
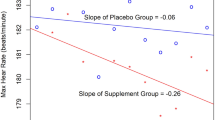
Absolute and relative VO2peak were decreased on R + 1/R + 3 (simple main effect for time, both P < 0.05; Table 4). Similarly, ventilatory threshold and peak workload were reduced immediately postflight (R + 1/R + 3, simple main effect for time, both P < 0.01; Table 4). HRpeak was unchanged after spaceflight. No group × time interaction effects were detected for any cardiorespiratory outcomes.
Discussion
We evaluated the protective effects of a high intensity/lower volume integrated aerobic and resistance exercise countermeasure to the multisystem deconditioning of long-duration spaceflight aboard the ISS; we compared these results to those of the somewhat lower intensity/higher volume regimen that is the standard exercise protocol for ISS crewmembers1. Overall, we found significant decrements in bone mineral density, muscle strength and endurance, and cardiorespiratory performance after long-duration spaceflight; these changes were mostly independent of the exercise countermeasure that was performed (Fig. 1).
Individual (open symbols) and mean (solid marks) percent losses from last preflight to first postflight test for control (open circles; hyphens) and Sprint subjects (open squares; tildes) for selected bone mineral density, muscle mass, muscle strength, muscle function, and cardiorespiratory fitness parameters. KneeExtIsok knee extension isokinetic peak torque at 60°s−1, AnkleExtIsok ankle extension isokinetic peak torque at 30°s−1, TrunkExtIsok trunk extension isokinetic peak torque at 60°s−1, LLM lean leg mass, BMD bone mineral density, VentThreshold ventilatory threshold, LP1RM leg press 1-repetition maximum. *Observations were excluded if not in the model, or missing pre or post.
In these results are a few noteworthy findings that have important application for astronauts’ mission critical task performance (e.g., extravehicular activity). First, the relative change in ventilatory threshold was approximately double that of VO2peak; this is similar to previous findings in bed rest18. Ventilatory threshold and other defined submaximal work levels (e.g., lactate threshold) have been shown to be more predictive of athletic performance than VO2peak19,20; this raises the interesting possibility that ventilatory threshold may be a better parameter for monitoring aerobic fitness in astronauts because it is more sensitive to change, is more aligned with the submaximal nature of occupational work, and may be a better indicator of fitness for duty (i.e., performance). Second, trunk extension strength (Table 2) was notably improved in Sprint subjects which may be related to the higher resistance exercise training intensity. Preservation of lumbar muscle strength may be helpful for prevention of spaceflight-induced back pain or disc herniation21,22.
High intensity training, while novel to spaceflight when this study was first implemented, is not a new phenomenon. It has been studied extensively in clinical23,24, community-dwelling25, and athletic populations9; these populations range in age from young children26,27 to older adults28,29. We and others have evaluated HIT in bed rest14,30, a ground-based analog of spaceflight, where it is largely effective to prevent multisystem physiologic deconditioning31. The appeal of HIT hinges on two potential benefits: (1) superior physiologic adaptations compared to traditional, longer-duration steady state/lower intensity training and (2) shorter/less frequent training sessions that offer different and distinct advantages for each of the aforementioned populations.
Analysis of exercise training logs revealed that aerobic exercise volume was slightly greater in CON while aerobic intensity—at least for a subset of common interval workouts—was similar between the Sprint and control groups; both groups performed aerobic exercise 6 days per week using a combination of interval and continuous workouts. Before and during the earliest part of this study (2011), aerobic interval exercise was employed rarely in the ISS standard care exercise prescription (CON) due to hardware limitations, but by the end of the project (2017) it had become an integral and regular component of the standard aerobic exercise regimen. Although this complicates the research design, it is increasingly important, especially in complex interdisciplinary research that spans many years, to develop methods of accepting and interpreting data when “standard of care” may change over the course of an investigation. In aggregate, our findings show similarity between the current individualized standard care exercise countermeasure and the high intensity/lower volume Sprint protocol with regards to spaceflight-induced changes in bone mineral density, muscle mass, muscle strength and function, and cardiorespiratory fitness. Based on these metrics alone, one would reasonably argue that the two programs are interchangeable. This can be viewed positively as providing flexibility for exercise programming: while some crewmembers may enjoy higher intensity/lower volume exercise such as the Sprint prescription, others may prefer the somewhat lower intensity/higher volume program.
Despite similar physiologic outcomes, the two programs differ in their requirements for one particularly valuable and limited resource: time. Of the current 2.5 h scheduled for the performance of 6 d wk−1 exercise countermeasures, ~60 min (45–75 min) is allocated to resistance exercise and ~30–45 min devoted to aerobic exercise for a total daily exercise duration of 1.5–2.0 h1,5. The low end of this range (1.5 h × 6 d wk−1) equates to a weekly exercise total of 9 h. In contrast, Sprint consumes at least 33% less time than the standard exercise program: three 60-min resistance exercise sessions, three 30-min continuous sessions, plus 3 aerobic interval sessions totaling <90 min equals ~6 h31. For future exploration missions with compressed timelines, small cabin spaces, and likely a single exercise device on which to perform both aerobic and resistance exercise for an entire crew, brief high intensity exercise prescriptions will be an extremely attractive programming option due to their efficacy and efficiency. Our bed rest studies have demonstrated that the Sprint exercise prescription is similarly effective over a range of exercise modalities and equipment including traditional ISS-like exercise equipment with or without testosterone supplementation and using only a single compact single exercise device that combines rowing and resistance exercise31.
Resistance exercise differed most markedly between the groups on its frequency. Sprint subjects performed about half of the number of repetitions on ARED, which is important both from a time and equipment usage/maintenance perspective. If equipment availability were to change in the future, or there was concern about wear and tear on exercise equipment, 3 days per week of resistance exercise, if intensity is maintained at a high level, should offer sufficient protection as evidenced by the mostly similar musculoskeletal outcomes we observed in the two groups despite markedly different total volume loads (sets × repetitions × load).
It is extremely important to note that physiologic outcomes across systems in both study groups (pooled) were substantially better than those previously reported in ISS crewmembers. The most modest differences were observed for muscle strength variables. For example, declines in isokinetic strength about the knee (−6%), ankle (−10%), and trunk (−5%) for the present study were notably better than previous crewmembers who exercised with iRED (knee: −14%, ankle: −14%, trunk: −7%) and moderately better compared to the losses of early ARED users (knee: −7%, ankle: −13%, trunk: −5%)2. Although leg press 1RM losses (−3%) were comparable to previously reported ISS values (−3%), the more functional cone test time (+7%) was better preserved than in previous crewmembers (+11%)32.
The greatest improvements were observed in bone health and cardiovascular fitness. Bone mineral density losses from the Russian Mir station, which lacked a resistance exercise capability, were 1.06%/month (lumbar spine) and 1.15%/month (femoral neck)33. When extrapolated to multi-month missions, such losses were alarming. Incremental improvements were made with the addition of iRED resistance exercise on the ISS (−3.7% lumbar spine; −6.1% femoral neck over ~6-month missions)34. Further improvement was observed after the installation of ARED (−2.6% lumbar spine; −4.1% femoral neck)34. The data reported in this paper of −1.7% (lumbar spine) and −1.7% (femoral neck) over multi-month missions represent another improvement. Such losses are within the precision error of the DXA measurement and can be considered negligible. It remains possible that changes in bone architecture (not evaluated in this report) could still exist, but bone density is now reasonably maintained.
A similar success story is observed for cardiorespiratory fitness. For the cardiorespiratory system, we measured a 6% decrease in VO2peak from preflight to postflight while our previous study of ISS crewmembers found a ~15% decrement in aerobic capacity postflight35. Together, these data suggest that current ISS exercise countermeasures (both standard of care and Sprint) provide considerably better protection of musculoskeletal and cardiorespiratory outcomes during long-duration spaceflight than did previous hardware and training protocols. These excellent outcomes allow us to consider, for the first time, whether the exercise countermeasures are sufficient or whether additional optimization is necessary. This raises interesting questions: Do we need to completely mitigate in-flight loss? If not, how much loss is acceptable? Does the amount of loss that would be accepted depend, at least in part, on the initial starting point for that individual or the mission tasks or landing scenarios that individual will be asked to perform? It is now time to shift the paradigm to consider these individual details and view astronauts as a tactical population akin to the military, police, and firefighters36. These operational professions have evolved from endeavoring to simply maintain an arbitrary fitness threshold to testing and preparing personnel to ensure that they are physiologically capable of meeting the demands of their job. In the last 5 years, both the Canadian Armed Forces and the US Army have completely overhauled their fitness for duty standards; both retired test batteries that largely featured tests of muscle and aerobic endurance and in their place adopted standards that inclusively evaluate aerobic fitness, anaerobic fitness, and muscle strength/power37,38. These changes were motivated by the inability of the previous fitness tests to predict performance in the field. In this new perspective that tightly links and subordinates testing and training to job performance, it is easy to envision a primary role for HIT in the preparation and training of soldiers and astronauts alike. Indeed, the developers of these new military fitness standards highlight the direct applicability of high intensity/low volume interval training (in contrast to legacy training that centered on low intensity/high volume exercise) to enhanced health and performance in military personnel39.
To fully extend this paradigm to astronauts and long-duration spaceflight, we must consider the key functions of exercise countermeasures that are essentially threefold: (1) to prevent long-term negative health consequences, (2) to ensure safe return to Earth, and (3) to facilitate optimal performance and the achievement of critical mission objectives. The two latter purposes are particularly salient to the “tactical population” view and the role of high intensity interval and strength training in astronaut fitness for duty. Return to Earth from the ISS is currently accomplished via the Russian Soyuz capsule in a well-supported terrestrial landing operation that requires relatively little physiologic effort of returning crews (e.g., they are physically extracted from the capsule). Upcoming flights aboard new commercial and NASA spacecraft will splashdown in the ocean with vehicle recovery and crew extraction nominally performed by the U.S. Navy and Air Force. However, in a contingency situation (e.g., an off target splashdown and/or a cabin emergency necessitating immediate evacuation), crewmembers will be required to egress the capsule unaided into a small, tethered life raft. Not surprisingly, preliminary testing with suited human subjects indicates that the physiologic demand of this relatively brief, off-nominal operation is moderate to high (unpublished data). Although unlikely, this operation represents a potential scenario for which crewmembers must be physiologically prepared upon return to Earth’s 1g environment. Much more certain—if not further into the future—are terrestrial exploration missions that will include unaided egress and a host of demanding surface operations (e.g., hill climbs and descents, habitat construction, materials transfer, and geologic equipment operation); potential off-nominal tasks include incapacitated crewmate rescue40,41. The functional relevance and metabolic specificity of high intensity resistance and aerobic interval exercise to the performance of critical mission tasks suggest that HIT should be a key component of astronaut exercise training and countermeasures.
This investigation has several limitations. First, astronauts self-selected into the group of their choosing. This was necessary because of the voluntary nature of spaceflight research studies as well as crewmembers’ reluctance to relinquish control of the fundamental nature of their exercise programs especially early in the study. Second, as with many spaceflight studies, the investigation has a relatively low number of participants, increasing the likelihood of a Type II error. Third, by its very nature, the standard care exercise countermeasure program employed by CON subjects included a degree of individualization and temporal change; this is in contrast to the Sprint protocol which was an inflexible experimental protocol. As previously noted, due to the study’s operational environment, the standard care exercise prescription evolved over the ~6 y study duration to include higher aerobic exercise intensities. Finally, not all post-flight testing was completed at the same time; for instance, although we were able to perform VO2peak tests for experimental subjects (SPRINT) on R + 1, most CON subjects were tested on R + 3, the typical timeframe for returning ISS crewmembers.
In summary, we evaluated the physiologic effects of a high intensity/lower volume experimental exercise countermeasure compared to the standard higher volume program performed by long-duration ISS crewmembers. Both exercise programs provided substantially better physiologic protection than historic exercise programs, and for current ISS missions, either program is an excellent option. The Sprint training program had outcomes that were as good as or, for a few variables, slightly better than control and offers several distinct advantages: (1) Sprint can be performed in a substantially shorter amount of time with less exercise equipment usage and (2) it may provide a more occupationally specific training experience that will better prepare crewmembers to optimally perform critical mission tasks while remaining safe and healthy.
Methods
Overview of research design
All National Aeronautics and Space Administration (NASA), Canadian Space Agency (CSA), European Space Agency (ESA), and Japan Aerospace Exploration Agency (JAXA) astronauts assigned to ISS flight were eligible to participate in this investigation. Subjects self-selected into one of two groups: (1) subjects that performed the experimental Sprint exercise program on the ISS (SPRINT) or (2) subjects that performed the standard individualized exercise program on the ISS (CON); all subjects completed the standard physiologic tests required of ISS crewmembers.
Subjects and facilities
Testing for this study was performed during ISS Increments 26S–50S (April 2011–September 2017). Twenty-six astronauts assigned to long-duration ISS missions participated (Table 5). Subject enrollment in the two groups was proportionally equivalent across the study such that neither group had a high concentration of subjects during a particular time period. The study was approved by the Institutional Review Board at NASA Johnson Space Center (JSC, Houston, TX), the Japan Aerospace Exploration Agency (JAXA) Institutional Review Board, the European Space Agency (ESA) Medical Board, and the Human Research Multilateral Review Board; all subjects provided written informed consent before participating in the study. The research was conducted in accord with the Declaration of Helsinki. All preflight and postflight testing was performed at NASA JSC. Room temperature was controlled between 20–23 °C. Exercise training during flight was conducted in the U.S. Laboratory Module of the ISS with cabin conditions similar to those on the ground with temperatures ranging from 20 to 22 °C and relative humidity of 30–40%. All crewmembers completed standard preflight medical screening and received clearance from their flight surgeon before participating in the study.
Exercise training
Exercise hardware
In-flight aerobic exercise was performed using the second-generation treadmill (T2) and CEVIS; resistance exercise was performed with ARED17. T2 was modified from a commercial Woodway Path treadmill (Woodway, Waukesha, WI) to support walking and running exercise between 2.4 and 19.3 km h−1. The user is loaded through a shoulder and waist harness that is terminally attached via bungee cords and c-clips to the treadmill deck surface. CEVIS operates similarly to a standard cycle ergometer providing workloads between 25 and 350 W at pedal speeds from 30 to 120 revolutions per minute. Crewmembers wore cycling shoes that snapped into the pedals and strapped themselves with a belt to the CEVIS frame or used the frame handles to remain appropriately positioned on the cycle. ARED simulates free weights with a constant load of 11–272 kg provided by vacuum cylinders and an inertial load effected by flywheels placed in the load path; both barbell and cable exercises can be performed16.
Exercise prescription
All subjects were matched with a NASA Astronaut Strength, Conditioning, and Rehabilitation (ASCR) specialist approximately two years in advance of their mission. Each subject’s ASCR developed an individualized exercise program based on their group assignment. Subjects also performed preflight exercise training to familiarize themselves with the inflight exercise devices and protcols and for preflight conditioning; exercise programs were not standardized during the preflight phase.
The Sprint exercise prescription is an evidence-based, integrated training program that consists of high intensity, lower volume exercise 6 d wk−1 (3 days of resistance and 6 days of aerobic)31,42,43. Subjects in this group completed high intensity interval aerobic exercise (3 d wk−1) and continuous aerobic exercise (3 d wk−1) on alternating days (Supplementary Table 3). Specifically, each of the three interval workouts was completed once per week (8 × 30-s intervals; 6 × 2-min intervals; and 4 × 4-min intervals); continuous aerobic exercise consisted of 30-min bouts at 75% VO2peak (Supplementary Table 3). Aerobic intensities were initially established based on heart rate (HR) at a percentage of VO2peak and HR response to exercise during preflight. Exercise prescriptions were adjusted during flight based on in-flight training, crewmember communication with their ASCR, and in-flight VO2peak cycle tests (not reported here). HR was monitored continuously during training sessions.
Resistance training for Sprint followed an undulating periodized model and was performed on the same day as the continuous aerobic exercise. Most days and when possible, continuous aerobic exercise was performed second, 4–6 h after the resistance exercise session to optimize adaptations. For the typical 6-month mission, resistance training was comprised of a single 24-week mesocycle. After an initial 2-week acclimatization period, load and repetitions were varied on a daily basis (high volume = 4 sets of 12 repetitions, moderate volume = 4 sets of 8 repetitions, low volume = 4 sets of 6 repetitions). Loads were prescribed such that the fourth set of each exercise was performed at near maximal to maximal intensity for the prescribed number of repetitions. Further, subjects were instructed to perform the fourth set of each exercise at each workout to muscle failure with loads for subsequent sessions adjusted accordingly. Thus, all sessions were defined as high intensity with the volume and load varying throughout the week. Subjects rotated among three routines throughout a mission (Supplementary Table 4). Sprint subjects performed upper body resistance exercise similar to that of control subjects (described below) 3 d wk−1. Time to perform the Sprint program was approximately 6 h per week (1.5 h continuous, <1.5 h intervals, and 3 h resistance exercise).
Control subjects participated in the standard care exercise countermeasure protocol. The program typically consisted of 1.5–2.0 h per day total of aerobic and resistance exercise, each performed 6 days per week. Although 2.5 h were scheduled for daily exercise on the ISS1, typically, exercise time was divided into 30–45 min of aerobic training and 60–75 min of resistance training with hardware configuration and postexercise hygiene comprising the remainder of total allotted time. Aerobic training consisted of interval or continuous steady-state exercise on either CEVIS or T2. The CEVIS protocols were developed using the preflight VO2peak test with prescribed work rates (W) between 70 and 100% VO2peak. The ASCRs adjusted the protocols during the mission based on individual performance during training sessions and crew feedback. The T2 protocols were based on pre-flight training and prescribed at 70–100% HRmax. For most crewmembers, external (harness/bungee) loading began at 60% bodyweight (static load measured when standing stationary on the treadmill belt) and increased to ~75–80% bodyweight as tolerated throughout the mission1. Resistance training followed a 9-day periodized program with linear progression of loads and undulating volume across two 12-week mesocycles (Supplementary Table 5). After a 2-week acclimatization period, loads were set at 70% of the repetition-maximum (RM) prescribed for that session (e.g., for a 4 × 6-repetition session, loads in Week 3 were 70% of 6RM) with loading intensity increasing 5% each week. Strength increases over the first mesocycle allowed most crewmembers to reach intensities of 110–120% of their early mission RMs by week 12. For the second mesocycle, loads were reduced to 70% of the crewmember’s new RM (determined from recent training session loads) and the progression of the first mesocycle was repeated. Thus, resistance exercise loading intensity and progression were lower and more conservative, respectively, compared to the Sprint protocol; this was compensated for with twice the workout frequency (6 d wk−1 vs. 3 d wk−1). A variation of squat, deadlift, and heel raises were each prescribed daily for CON subjects followed by rotating exercises focusing on upper body and stability musculature. Heel raises were prescribed as 4 sets × 20 repetitions. Time to perform the CON program was approximately 9–10 h per week (3–4 h continuous and interval aerobic exercise and 6–7 h resistance exercise).
Outcome measures
Exercise training
Aerobic and resistance exercise training variables were recorded and are presented descriptively. Aerobic exercise outcomes were CEVIS and T2 normalized volume (total min/mission duration in weeks) and average peak HR (b min−1 and % maximum) for 30-s, 2-min, and 4-min intervals and 30-min continuous sessions. For resistance exercise, average load (kg) and average repetitions per week were calculated for squat, heel raise, and deadlift and their variations (“squat”: back squat, single leg squat, sumo squat; “heel raise”: heel raise and single leg heel raise; “deadlift”: deadlift, Romanian deadlift, and sumo deadlift). Total volume load (sets × repetitions × load) for each subject’s mission was also calculated and normalized to mission duration (total volume/mission duration in weeks).
Bone densitometry and muscle mass
DXA scans were obtained using a single densitometer (Hologic Discovery; Hologic Inc., Waltham, MA, USA). Two bone densitometry technologists, certified by the International Society for Clinical Densitometry (ISCD), performed and analyzed the scans. For a given crewmember, a single technologist performed both the preflight and postflight scans. Scans were performed at approximately 90 days preflight (L-90) and again 1–2 weeks after landing (R + 7). At each test session, the following fan-beam DXA scans were performed: left and right hip, lumbar spine, whole body, and left heel. Scans were performed and analyzed according to standard procedures recommended by the manufacturer, with the exception of hip and heel scans. The global region of interest box for the hip was positioned manually, with the lateral margin placed adjacent to the lateral cortex of the greater trochanter and the distal border placed a set number of lines from the lesser trochanter’s distal margin44,45. Heel scans were obtained using the forearm scan mode, with the subject seated on the scanner and the foot restrained in a lateral position within a custom jig. In addition to areal bone mineral density (BMD, g cm2) obtained from the scans listed above, whole body and regional lean mass (fat-free, bone-free mass) and fat mass were determined from the whole body scans using standard Hologic analysis software. The BMD precision values (% coefficient of variation, % CV) for the scanning laboratory were as follows: left and right total hip, 0.7% and 0.9%; left and right trochanter, 1.1% and 1.1%; left and right femur neck, 1.2% and 1.5%; lumbar spine, 0.5%; heel, 1.0%; and whole body, 1.0%. Precision of soft tissue values from the whole body scans were: whole body lean mass, 0.9% and whole body fat mass, 2.1%. Calibration of the Hologic densitometer was verified by regular scanning of a calibration phantom (at least weekly as well as on the day of subject testing) with scans analyzed using the manufacturer’s automated software.
Muscle strength
Isokinetic strength data were acquired for the knee, ankle, and trunk via a Biodex System 4 dynamometer (Biodex Medical Systems, Shirley, NY) using NASA’s Medical Volume B 5.3 Isokinetic Testing protocol2. Subjects were tested twice prelaunch (L-9 months and L-50 d) with the latter test used as the preflight baseline and three times after return (R + 5 d, R + 14 d, and R + 30 d). Trunk testing was not performed at the R + 5 postflight test as specified in the Medical Volume B 5.3 Isokinetic Testing protocol due to concerns about post-flight low back pain. The right leg was used for all testing unless previous injury indicated use of the contralateral limb.
Specifically, subjects wore laboratory-provided athletic shoes to maintain standardized footwear and completed a 5-min warm up on a cycle ergometer (Lode, Groningen, Netherlands) at 50 W before all test sessions. Calibration was performed before each test session per manufacturer instructions. At the first preflight session, the dynamometer was fit to each subject, and position settings were recorded so that they could be replicated for future test sessions. An anatomic reference (knee = 90°, ankle = 0°, trunk = 0°) was measured with a hand-held goniometer during subject set-up for each joint tested. Knee testing was conducted in the seated position over a range of 95° (flexion) to 20° (extension). Ankle testing was performed prone over a subject’s maximal active range of motion rounded down to the nearest 5°. For example, if a subject could attain −18° of ankle flexion and 37° of ankle extension, range of motion was set at −15° (dorsiflexion) to 35° (plantarflexion). Trunk testing was conducted in the seated position from 0° (extension) to 90° (flexion). Testing was always performed in the order described below.
After cycle ergometer warm up, subjects performed five warm-up repetitions of knee extension/flexion (60°s−1, concentric/concentric) at 50% of their perceived maximum effort followed by two repetitions at 75–90% of maximum effort. After a 1- to 2-min rest, subjects performed three maximal knee extension/flexion repetitions. Subsequently, subjects performed three warmup repetitions of knee extension/flexion (180° s−1, concentric/concentric) at 50% of their perceived maximum effort followed by a 2-min rest. Then they completed 20 consecutive maximal repetitions (180° s−1, concentric/concentric) of knee extension/flexion. Ankle testing was performed in a similar manner. After an initial warm up (five repetitions at 50% of perceived maximum, two repetitions at 75–90% of maximum effort), subjects completed three maximal repetitions (30° s−1, concentric/concentric) of ankle extension (plantarflexion)/flexion (dorsiflexion). The final ankle tests were also ankle extension/flexion (30° s−1), but these tests were completed eccentrically with subjects maximally resisting the movement of the dynamometer. After one warm-up repetition at 50% of perceived maximal effort, subjects completed five maximal repetitions of discrete ankle plantarflexion followed by a set of five maximal repetitions of discrete ankle dorsiflexion. Last, subjects performed five warm-up repetitions of trunk flexion/extension (60° s−1, concentric/concentric) at 50% of their perceived maximum followed by two repetitions at 75–90% of maximum effort. After a 1- to 2-min rest, subjects performed three maximal trunk flexion/extension repetitions.
Subjects were instructed not to eat a large meal for at least 2 h before testing but could eat a light snack up to 1 h before testing. No nicotine or alcohol was allowed for 8 h before testing; caffeine was restricted to one cup of coffee or its caffeine equivalent which was permitted up to 1 h before testing. In addition, subjects could not perform a neutral buoyancy dive (training for extravehicular activity) for 72 h before testing, maximal exercise for 24 h before a scheduled evaluation, or any exercise 8 h before testing.
Muscle function
The functional fitness test (FFT) battery evaluates functional muscular strength, flexibility, and agility. The FFT was performed 60–90 days before flight; postflight testing was conducted 5–7 days after landing32. The following four measures were evaluated:
Leg press (1RM)
After a warm up at ~50% load for 10 repetitions on a leg press machine (Cybex International, Medway, MA), the load was increased 15–20% each set with decreasing repetitions until the subject could only complete 1 repetition at which point the load was increased 5–10% until failure. Subjects rested 3–5 min between sets. Leg press 1RM was recorded as the maximum weight successfully lifted.
Bench press (1RM)
After a warm up at ~30% load for 10 repetitions on a smith machine (Cybex International, Medway, MA), the load was increased 10–20% each set with decreasing repetitions until the subject could only complete 1 repetition at which point the load was increased 5–10% until failure. Subjects rested 3–5 min between sets. Bench press 1RM was recorded as the maximum weight successfully lifted.
Sit and reach
Lower back and hamstring flexibility was tested using an Acuflex I sit and reach box (Novel Products, Rockton, IL). Subjects were instructed to remove their shoes and place the feet against the footplate, then slowly reach forward, bending at the lumbar spine with knees in a fully extended position and hands one over the other. Subjects reached forward as far as possible while holding the most distant point momentarily. The score was recorded as the furthest reach of three trials.
Cone agility
Cone agility measured subjects’ ability to move quickly in four directions (forward, backward, left, and right) and to rapidly change directions32. Cones were placed at corners of a 4.57 m square and, starting at the lower left corner of the square, subjects were instructed to: (1) move forward to the upper left corner, (2) shuffle right to the upper right corner, (3) move backwards to the lower right corner, (4) shuffle left to the lower left corner (starting point), (5a) turn 45° to the right and move forward in a diagonal direction to the upper right corner, (5b) turn 135° to the left and move forward to the upper left corner, and (5c) turn 135° to the left and move forward to the lower right corner. The entire circuit was completed as quickly as possible; a hand-held stopwatch quantified the best of three trials.
Cardiorespiratory fitness
Aerobic fitness was evaluated during upright peak cycle ergometry tests (Lode Excalibur Sport; Lode B.V., Groningen, the Netherlands) performed twice before launch (L-180 d and L-50 d with the latter used for pre-flight baseline) and twice after return. Sprint subjects were tested on R + 1 and R + 30; most control subjects were tested on R + 3 and R + 30. The protocol consisted of a 3-min warm up at 50 W, followed by 1-min stepwise increments of 25 W to volitional fatigue. The HR and heart rhythm were monitored continuously (GE CASE, GE Healthcare, Chicago, IL). Ventilation and expired gas fractions (FEO2 and FECO2) were measured continuously using the Portable Pulmonary Function System (PPFS), a metabolic gas analyzer commissioned by the European Space Agency and manufactured by the Danish Aerospace Company (DAC, Odense, DK)35. VO2pk was defined as the highest 30-s average and was confirmed by the attainment of at least two of three criteria: (1) respiratory exchange ratio of > 1.09; (2) HR >90% of age-predicted maximum; (3) a plateau in VO2 (an increase of <150 mL min−1) from the previous stage. Ventilatory threshold was defined as the point at which VCO2 began to increase disproportionate to VO2, and VE/VO2 increased with no comcomitant increase in VE/VCO246.
Statistical analysis
Statistical analyses were conducted using Stata, IC software (v15.1) setting two-tailed alpha to reject the null hypothesis at 0.05. Our experimental design was a mixed-factorial with repeated observations collected preflight and postflight in which astronauts either participated in the Sprint intervention or the standard ISS exercise protocol. All outcomes were collected preflight and postflight with repeated postflight observations on some outcomes. We evaluated the effects of the Sprint exercise protocol (relative to standard of care) and spaceflight (preflight vs. each postflight) in separate mixed-effects models per dependent variable, with a priori simple interaction terms comparing each postflight to preflight, and simple interaction effects evaluating the relative change from preflight by group. Each of these models included a random y-intercept to accommodate the within-subjects experimental design, and degrees of freedom calculated per our repeated-measures experimental design. Each statistical test also underwent a rigorous examination of the distribution of model residuals before hypothesis testing and while nearly all of our analyses were satisfactory, it was necessary to use the inverse-cubic transformation for one outcome (cone test performance) to meet model assumptions, and to occasionally eliminate an overly influential observation (standardized residuals >3 and failure of the normality test). The data contained in this study constitute private medical information. As such, they are only available upon request in a deidentified fashion from NASA’s Life Sciences Data Archive (Life Sciences Data Archive).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data from this study may be obtained through a data request in the NASA Life Science Data Archive (https://lsda.jsc.nasa.gov/Request/dataRequest). The study title “Integrated Resistance and Aerobic Training Study—Sprint” should be entered in the “Data Request Description”.
References
Loehr, J. A. et al. Physical training for long-duration spaceflight. Aerosp. Med. Hum. Perform. 86, A14–A23 (2015).
English, K. L., Lee, S. M., Loehr, J. A., Ploutz-Snyder, R. J. & Ploutz-Snyder, L. L. Isokinetic strength changes following long-duration spaceflight on the ISS. Aerosp. Med. Hum. Perform. 86, A68–A77 (2015).
Fitts, R. H. et al. Prolonged space flight-induced alterations in the structure and function of human skeletal muscle fibres. J. Physiol. 588, 3567–3592 (2010).
Gopalakrishnan, R. et al. Muscle volume, strength, endurance, and exercise loads during 6-month missions in space. Aviat. Space Environ. Med. 81, 91–102 (2010).
Trappe, S. et al. Exercise in space: human skeletal muscle after 6 months aboard the International Space Station. J. Appl. Physiol. 106, 1159–1168 (2009).
Moore, A. D., Lynn, P. A. & Feiveson, A. H. The first 10 years of aerobic exercise responses to long-duration ISS flights. Aerosp. Med. Hum. Perform. 86, 78–86 (2015).
Lang, T. et al. Cortical and trabecular bone mineral loss from the spine and hip in long-duration spaceflight. J. Bone Miner. Res. 19, 1006–1012 (2004).
Sibonga, J. D. et al. Adaptation of the skeletal system during long-duration spaceflight. Clin. Rev. Bone Miner. Metab. 5, 249–261 (2008).
Ronnestad, B. R., Askestad, A. & Hansen, J. HIT maintains performance during the transition period and improves next season performance in well-trained cyclists. Eur. J. Appl. Physiol. 114, 1831–1839 (2014).
Wisloff, U. et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115, 3086–3094 (2007).
Terry, L., Sprinz, E. & Ribeiro, J. P. Moderate and high intensity exercise training in HIV-1 seropositive individuals: a randomized trial. Int. J. Sports Med. 20, 142–146 (1999).
Tabata, I. et al. Effects of moderate-intensity endurance and high-intensity intermittent training on anaerobic capacity and VO2max. Med. Sci. Sports Exerc. 28, 1327–1330 (1996).
Greenleaf, J. E., Bernauer, E. M., Ertl, A. C., Trowbridge, T. S. & Wade, C. E. Work capacity during 30 days of bed rest with isotonic and isokinetic exercise training. J. Appl. Physiol. 67, 1820–1826 (1989).
Lee, S. M. et al. LBNP exercise protects aerobic capacity and sprint speed of female twins during 30 days of bed rest. J. Appl. Physiol. 106, 919–928 (2009).
Lasevicius, T. et al. Effects of different intensities of resistance training with equated volume load on muscle strength and hypertrophy. Eur. J. Sport Sci. 18, 772–780 (2018).
Loehr, J. A. et al. Musculoskeletal adaptations to training with the advanced resistive exercise device. Med. Sci. Sports Exerc. 43, 146–156 (2011).
Korth, D. W. Exercise countermeasure hardware evolution on ISS: the first decade. Aerosp. Med. Hum. Perform. 86, A7–13 (2015).
Convertino, V. A., Karst, G. M., Kirby, C. R. & Goldwater, D. J. Effect of simulated weightlessness on exercise-induced anaerobic threshold. Aviat. Space Environ. Med. 57, 325–331 (1986).
Engelbrecht, L. & Terblanche, E. Physiological performance predictors in mountain bike multi-stage races. J. Sports Med. Phys. Fit. 58, 951–956 (2018).
Coyle, E. F., Coggan, A. R., Hopper, M. K. & Walters, T. J. Determinants of endurance in well-trained cyclists. J. Appl. Physiol. 64, 2622–2630 (1988).
Bailey, J. F. et al. From the international space station to the clinic: how prolonged unloading may disrupt lumbar spine stability. Spine J. 18, 7–14 (2018).
Chang, D. G. et al. Lumbar spine paraspinal muscle and intervertebral disc height changes in astronauts after long-duration spaceflight on the International Space Station. Spine 41, 1917–1924 (2016).
Conraads, V. M. et al. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int. J. Cardiol. 179, 203–210 (2015).
Moholdt, T. et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: a randomized controlled study. Clin. Rehabil. 26, 33–44 (2012).
Fisher, G. et al. High intensity interval- vs moderate intensity- training for improving cardiometabolic health in overweight or obese males: a randomized controlled trial. PLoS ONE 10, e0138853 (2015).
Cvetkovic, N. et al. Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scand. J. Med. Sci. Sports 28, 18–32 (2018).
Thivel, D. et al. High-intensity interval training in overweight and obese children and adolescents: systematic review and meta-analysis. J. Sports Med. Phys. Fit. 59, 310–324 (2019).
Moro, T. et al. High intensity interval resistance training (HIIRT) in older adults: Effects on body composition, strength, anabolic hormones and blood lipids. Exp. Gerontol. 98, 91–98 (2017).
Hwang, C. L. et al. Novel all-extremity high-intensity interval training improves aerobic fitness, cardiac function and insulin resistance in healthy older adults. Exp. Gerontol. 82, 112–119 (2016).
Ploutz-Snyder, L. L. et al. Integrated resistance and aerobic exercise protects fitness during bed rest. Med. Sci. Sports Exerc. 46, 358–368 (2014).
Ploutz-Snyder, L. L. et al. Exercise training mitigates multisystem deconditioning during bed rest. Med. Sci. Sports Exerc. 50, 1920–1928 (2018).
Laughlin, M. S., Guilliams, M. E., Nieschwitz, B. A. & Hoellen, D. Functional fitness testing results following long-duration ISS missions. Aerosp. Med. Hum. Perform. 86, A87–A91 (2015).
LeBlanc, A. et al. Bone mineral and lean tissue loss after long duration space flight. J. Musculoskelet. Neuronal Interact. 1, 157–160 (2000).
Sibonga, J. D., Spector, E. R., Johnston, S. L. & Tarver, W. J. Evaluating bone loss in ISS astronauts. Aerosp. Med. Hum. Perform. 86, A38–A44 (2015).
Moore, A. D. Jr. et al. Peak exercise oxygen uptake during and following long-duration spaceflight. J. Appl. Physiol. 117, 231–238 (2014).
Hackney, K. J. et al. The astronaut-athlete: optimizing human performance in space. J. Strength Cond. Res. 29, 3531–3545 (2015).
Stockbrugger, B. G., Reilly, T. J., Blacklock, R. E. & Gagnon, P. J. Reliability of the individual components of the Canadian Armed Forces Physical Employment Standard. Appl. Physiol. Nutr. Metab. 43, 663–668 (2018).
Foulis, S. A. et al. U.S. army physical demands study: development of the occupational physical assessment test for combat arms soldiers. J. Sci. Med. Sport 20(Suppl 4), S74–S78 (2017).
Gibala, M. J., Gagnon, P. J. & Nindl, B. C. Military applicability of interval training for health and performance. J. Strength Cond. Res. 29(Suppl 11), S40–S45 (2015).
Ryder, J. W. et al. A novel approach for establishing fitness standards for occupational task performance. Eur. J. Appl. Physiol. 119, 1633–1648 (2019).
Sutterfield, S. L. et al. Prediction of planetary mission task performance for long-duration spaceflight. Med. Sci. Sports. Exerc. 51(8), 1662–1670 (2019).
Kraemer, W. J., Ratamess, N. A. & French, D. N. Resistance training for health and performance. Curr. Sports Med. Rep. 1, 165–171 (2002).
Rhea, M. R., Ball, S. D., Phillips, W. T. & Burkett, L. N. A comparison of linear and daily undulating periodized programs with equated volume and intensity for strength. J. Strength Cond. Res. 16, 250–255 (2002).
Spector, E., LeBlanc, A. & Shackelford, L. Hologic QDR 2000 whole-body scans: a comparison of three combinations of scan modes and analysis software. Osteoporos. Int. 5, 440–445 (1995).
LeBlanc, A. D. et al. Alendronate as an effective countermeasure to disuse induced bone loss. J. Musculoskelet. Neuronal Interact. 2, 335–343 (2002).
Beaver, W. L., Wasserman, K. & Whipp, B. J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 60, 2020–2027 (1986).
Acknowledgements
We thank members of the NASA Exercise Physiology and Countermeasures Laboratory, our Astronaut Strength Conditioning and Rehabilitation (ASCR) colleagues, and the astronaut test subjects who enthusiastically participated in this study. This study was supported by research grants from the NASA Human Research Program and the National Space Biomedical Research Institute.
Author information
Authors and Affiliations
Contributions
L.L.P.-S. developed the study concept. K.L.E., M.D., E.G., R.B., J.W.R., M.G., J.M.S., and L.L.P.-S. collected and reduced the data. K.L.E., M.D., E.G., R.B., J.W.R., R.P.-S., M.G., J.M.S., and L.L.P.-S. analyzed and interpreted the results. K.L.E. wrote the paper together with all co-authors. All authors approved the final work and are accountable for the accuracy and integrity of the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
English, K.L., Downs, M., Goetchius, E. et al. High intensity training during spaceflight: results from the NASA Sprint Study. npj Microgravity 6, 21 (2020). https://doi.org/10.1038/s41526-020-00111-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41526-020-00111-x
This article is cited by
-
Effects of body size and countermeasure exercise on estimates of life support resources during all-female crewed exploration missions
Scientific Reports (2023)
-
Impacts of radiation exposure, hindlimb unloading, and recovery on murine skeletal muscle cell telomere length
npj Microgravity (2023)
-
Genetic diversity modulates the physical and transcriptomic response of skeletal muscle to simulated microgravity in male mice
npj Microgravity (2023)
-
Effects of exercise countermeasures on multisystem function in long duration spaceflight astronauts
npj Microgravity (2023)
-
Effect of Exercise on Energy Expenditure and Body Composition in Astronauts Onboard the International Space Station: Considerations for Interplanetary Travel
Sports Medicine (2022)