Abstract
Hypertension is associated with vascular failure, such as increased arterial stiffness, endothelial dysfunction, and vascular smooth muscle dysfunction. The purpose of this study was to investigate the relationship between out-of-office blood pressure and vascular function in patients receiving antihypertensive drugs. We assessed out-of-office blood pressure, including daytime and night-time blood pressure, by home blood pressure monitoring and performed vascular function tests, including brachial-ankle pulse wave velocity (baPWV), flow-mediated vasodilation (FMD), and nitroglycerine-induced vasodilation (NID), in 169 patients receiving antihypertensive drugs, of whom 86 (50.9%) had normotension, 23 (13.6%) had isolated nocturnal hypertension (night-time systolic blood pressure ≥120 mm Hg), 26 (15.4%) had isolated daytime hypertension (daytime systolic blood pressure ≥135 mm Hg), and 34 (20.1%) had sustained hypertension (daytime and nocturnal hypertension). baPWV was significantly higher in patients with sustained hypertension than in those without sustained hypertension (1585 ± 257 cm/s in normotension; 1687 ± 267 cm/s in isolated nocturnal hypertension; 1688 ± 313 cm/s in isolated daytime hypertension; and 1923 ± 399 cm/s in sustained hypertension; P < 0.001). baPWV above the cutoff value of 1858 cm/s, derived from receiver operating characteristic curve analysis to diagnose patients with sustained hypertension, was significantly associated with sustained hypertension after adjustment of other confounding factors (odds ratio, 5.01; 95% confidence interval, 1.94–13.41; P < 0.001). In contrast, there was no significant association of home blood pressure status with FMD or NID in these patients. In patients receiving antihypertensive drugs, baPWV was significantly associated with sustained hypertension, whereas FMD and NID were impaired regardless of the home blood pressure status.
Similar content being viewed by others
Introduction
Hypertension is globally the strongest modifiable risk factor for cardiovascular death and related disability [1]. Although there is strong evidence that blood pressure-lowering therapy is beneficial for the prevention of major cardiovascular events in hypertensive patients [2], recent epidemiological studies have shown that patients receiving antihypertensive drugs still have a higher cardiovascular risk than those not receiving antihypertensive drugs regardless of the achieved clinic blood pressure level and that there were no stepwise increases in cardiovascular risks with an increase in blood pressure level in patients receiving antihypertensive drugs [3,4,5,6]. These findings suggest that a substantial residual cardiovascular risk is still present in patients receiving antihypertensive drugs and that clinic blood pressure may not be a useful marker for the management of hypertension in treated patients with hypertension. Recently, out-of-office blood pressure measurements have been recommended for more accurate confirmation and better management of hypertension [7, 8]. Accumulating evidence has revealed that out-of-office blood pressure is a stronger and more reliable predictor of cardiovascular events than is clinic blood pressure [9, 10]. In addition, among treated patients with hypertension, out-of-office night-time systolic blood pressure but not out-of-office daytime systolic blood pressure has been shown to be independently associated with 10-year risk of cardiovascular events [11], indicating that measurement of out-of-office blood pressure, especially night-time blood pressure, is necessary for further cardiovascular risk assessment in patients receiving antihypertensive drugs.
Vascular function tests have been performed for an understanding of the underlying pathophysiology of cardiovascular disorders and for risk assessment in patients with cardiovascular risk factors or cardiovascular diseases [12,13,14,15]. Although the relationship between out-of-office blood pressure and vascular function has been investigated in previous studies involving antihypertensive drug naïve individuals [16,17,18,19], there is little information on the relationship between out-of-office blood pressure and vascular function in patients receiving antihypertensive drugs. In addition, to our knowledge, there has been no study in which multiple vascular function tests were simultaneously performed in patients treated with hypertension. We therefore measured out-of-office blood pressure using a home blood pressure monitoring device and performed vascular function tests, including brachial-ankle pulse wave velocity (baPWV) as an index of arterial stiffness, flow-mediated vasodilation (FMD) as an index of endothelial function, and nitroglycerine-induced vasodilation (NID) as an index of vascular smooth muscle function, in patients receiving antihypertensive drugs to investigate the relationship between home blood pressure status and vascular function.
Methods
Study design
This study was conducted in patients from the Hiroshima Registry for Evaluation and Treatment of Nocturnal and Early Morning Hypertension (Hiroshima NOCTURNE). The Hiroshima NOCTURN is a prospective multicenter study to investigate whether elevated night-time blood pressure assessed by a home blood pressure monitoring device can be normalized by aggressive antihypertensive therapy and to evaluate the effect of reduction of night-time blood pressure on future cardiovascular events in patients with hypertension receiving antihypertensive drugs. Patients aged 20 years or more who had been treated with antihypertensive drug for more than 3 months with a diagnosis of hypertension defined in the Japanese Society of Hypertension Guidelines for the Management of Hypertension were enrolled [7]. Patients with severe valvular heart disease, moderate to severe heart failure (NYHA class III or IV), lethal arrhythmia with an implantable cardioverter defibrillator, end-stage renal disease receiving dialysis, malignant disease, hepatic cirrhosis, corticosteroid therapy, or immunosuppressive therapy, possible pregnant women, women with pregnancy, and lactating women were excluded. A total of 169 Japanese adults (104 men and 65 women; mean age, 69.5 ± 9.2 years; age range, 36–87 years) with agreement for measurements of vascular function at enrollment were recruited from the Hiroshima NOCTURN. The ethical committees of our institutions approved the study protocol. The study was executed in accordance with the Helsinki Declaration of 1975. Written informed consent for participation in the study was obtained from all participants. The protocol was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000019173). Additional details are available in the online-only Data Supplement.
Measurement of blood pressure
Home blood pressure monitoring was performed using a cuff oscillometric device (HEM-7252G-HP or HEM7080IC; Omron Healthcare Co., Kyoto, Japan) that could be set to measure blood pressure automatically during sleep (night-time blood pressure). All data, including blood pressure, heart rate, and measurement time, obtained using HEM-7252G were transmitted automatically to the Medical LINK program, a cloud-based remote monitoring system, provided by Omron Healthcare. All data obtained using HEM7080IC were stored in its memory. Patients were instructed to measure their morning blood pressure twice within 1 h after waking, evening blood pressure twice before bedtime, and night-time blood pressure during sleep for 7 consecutive days. Night-time blood pressure was measured automatically at 2:00, 3:00, 4:00, and 5:00 AM (4 points). In patients who got up before 5:00 AM, night-time blood pressure was measured at 1:00, 2:00, 3:00, and 4:00 AM. Nocturnal hypertension was defined as the average of all night-time systolic blood pressure measurements ≥120 mm Hg, and daytime hypertension was defined as the average of all morning systolic blood pressure measurements ≥135 mm Hg and/or the average of all evening systolic blood pressure measurements ≥135 mm Hg [7]. In accordance with these definitions, we divided patients into four groups: patients with normotension (normotensive group); patients with isolated nocturnal hypertension (isolated nocturnal hypertension group); patients with isolated daytime hypertension (isolated daytime hypertension group); and patients with nocturnal and daytime hypertension (sustained hypertension group).
Study protocol
Subjects fasted the previous night and abstained from alcohol, smoking, caffeine, and antioxidant vitamins on the day of the vascular function tests. The subjects were kept in the supine position in a quiet, dark, and air-conditioned room (constant temperature of 23–26 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. Vascular function tests, including baPWV, FMD, and NID, were performed at least 20 min after maintaining the supine position. The observers were blind to the form of examination.
Measurement of baPWV
baPWV was measured using a volume-plethysmographic apparatus (Form PWV/ABI, Omron Health Care Co., Kyoto, Japan). Detailed information on the study protocol and measurement of baPWV is provided in the online-only Data Supplement.
Measurements of FMD and NID
FMD and NID were measured using UNEXEF18G (UNEX Co., Nagoya, Japan), an ultrasound instrument specialized for FMD and NID measurement equipped with an automated edge detection system for measurement of brachial artery diameter. Detailed information on the study protocol and measurements of FMD and NID is provided in the online-only Data Supplement.
Statistical analysis
Results are presented as means ± SD. All reported probability values were 2-sided, and a probability value of <0.05 was considered statistically significant. Categorical variables were compared by means of the chi-square test. Continuous variables were compared by using ANOVA with Bonferroni’s test for post-hoc comparisons for multiple groups. Univariate linear regression analyses were performed to assess relationships among the variables. Multiple linear regression analysis using forward stepwise selection was performed to identify independent variables associated with baPWV. Multiple logistic regression analysis using forward stepwise selection was performed to identify independent variables associated with sustained hypertension. Receiver operating characteristic (ROC) curve analyses were carried out to assess the sensitivity and specificity and to confirm the optimal cutoff values of baPWV, FMD, and NID to diagnose patients with sustained hypertension. Additional details are available in the online-only Data Supplement. The data were processed using JMP version 11 (SAS institute, Cary, NC).
Results
Baseline clinical characteristics
The baseline clinical characteristics are summarized in Table 1. Of the 169 subjects, 104 (61.5%) were men, 131 (78.0%) had dyslipidemia, 46 (27.4%) had diabetes mellitus, 33 (19.8%) had coronary artery disease, 27 (16.1%) had cerebrovascular disease, and 86 (51.2%) were smokers. All of the subjects were being treated with antihypertensive drugs: 82.6% were on calcium channel blockers, 74.9% were on angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors, 11.4% were on β-blockers, and 22.2% were on diuretics. Mean values of systolic blood pressure were 127.7 ± 14.1 mm Hg for clinic systolic blood pressure, 129.4 ± 11.6 mm Hg for morning systolic blood pressure, 123.5 ± 11.5 mm Hg for evening systolic blood pressure, and 115.4 ± 10.8 mm Hg for night-time systolic blood pressure. Of the 169 subjects, 86 (50.9%) were in the normotensive group, 23 (13.6%) were in the isolated nocturnal hypertension group, 26 (15.4%) were in the isolated daytime hypertension group, and 34 (20.1%) were in the sustained hypertension group.
Relationship between baPWV and home blood pressure
Of the 169 subjects, 164 were included in analysis to investigate the relationship between home blood pressure status and baPWV after excluding patients with ankle-brachial pressure index values less than 0.90 (n = 2) and those without measurement of baPWV (n = 3). The baseline clinical characteristics are summarized in Table 2. The mean value of baPWV was 1683 ± 324 cm/s (median, 1626 cm/s; interquartile range [IQR], 1462 to 1853 cm/s; range, 1167–3220 cm/s). baPWV correlated significantly with morning systolic blood pressure (β = 9.87, r = 0.36, P < 0.001), evening systolic blood pressure (β = 8.93, r = 0.32, P < 0.001), and night-time systolic blood pressure (β = 11.0, r = 0.36, P < 0.001) (online Supplementary Table 1). baPWV was significantly higher in the sustained hypertension group than in the normotensive group, isolated nocturnal hypertension group, or isolated daytime hypertension group (normotensive group, 1585 ± 257 cm/s; isolated nocturnal hypertension group, 1687 ± 267 cm/s; isolated daytime hypertension group, 1688 ± 313 cm/s; sustained hypertension group, 1923 ± 399 cm/s; P < 0.001 in normotensive group vs. sustained hypertension group; P = 0.03 in isolated nocturnal hypertension group vs. sustained hypertension group; P = 0.02 in isolated daytime hypertension group vs. sustained hypertension group; Fig. 1a). After adjustment with mean blood pressure at the measurement of baPWV, baPWV (mean ± s.e.m) was significantly higher in the sustained hypertension group than in the normotensive group and isolated nocturnal hypertension group, although there was no significant difference between the sustained hypertension group and isolated daytime hypertension group (normotensive group, 1598 ± 32 cm/s; isolated nocturnal hypertension group, 1655 ± 62 cm/s; isolated daytime hypertension group, 1704 ± 57 cm/s; sustained hypertension group, 1900 ± 51 cm/s; P < 0.001 in normotensive group vs. sustained hypertension group; P = 0.02 in isolated nocturnal hypertension group vs. sustained hypertension group; P = 0.07 in isolated daytime hypertension group vs. sustained hypertension group; online Supplementary Figure 1). Multivariate analysis revealed that sustained hypertension was significantly associated with higher baPWV (β = 0.191, P = 0.003) (Table 3).
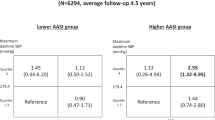
ROC curve analysis to determine the discriminative power of baPWV to diagnose patients with sustained hypertension revealed that the optimal cutoff value of baPWV to diagnose patients with sustained hypertension was 1858 cm/s with an AUC value of 0.74, sensitivity of 0.55, and specificity of 0.83 (Fig. 2a). Multivariate analysis revealed that baPWV above the cutoff value of 1858 cm/s was significantly associated with sustained hypertension in treated hypertensives (odds ratio, 5.01; 95% confidence interval, 1.94–13.41; P < 0.001) (Table 4).
Relationships between FMD, NID, and home blood pressure
Of the 169 subjects, 151 were included in analysis to investigate associations of home blood pressure status with FMD and NID after excluding patients who had received nitrate treatment (n = 10) and those without measurement of FMD (n = 8). The baseline clinical characteristics are summarized in online Supplementary Table 2. The mean value of FMD was 2.0 ± 2.5% (median, 1.3%; IQR, 0.6 to 2.7%; range, −2.5–15.6%) and that of NID was 10.3 ± 5.2% (median, 10.2%; IQR, 6.3–14.1%; range, 0.2–27.0%). FMD did not correlate significantly with morning systolic blood pressure (β = 0.005, r = −0.02, P = 0.79), evening systolic blood pressure (β = 0.001, r = 0.007, P = 0.93), or night-time systolic blood pressure (β = −0.003, r = −0.01, P = 0.88) (online Supplementary Table 1). There was no significant difference in FMD among the four groups stratified according to daytime and night-time systolic blood pressures (normotensive group, 2.1 ± 2.7%; isolated nocturnal hypertension group, 1.5 ± 1.7%; isolated daytime hypertension group, 1.9 ± 1.9%; sustained hypertension group, 2.3 ± 2.7%; P = 0.69; Fig. 1b). NID correlated significantly with morning systolic blood pressure (β = −0.084, r = −0.19, P = 0.02) and night-time systolic blood pressure (β = −0.091, r = −0.19, P = 0.02) but not with evening systolic blood pressure (β = −0.048, r = −0.11, P = 0.19) (online Supplementary Table 1). There was no significant difference in NID among the four groups (normotensive group, 11.2 ± 5.2%; isolated nocturnal hypertension group, 9.3 ± 5.0%; isolated daytime hypertension group, 9.8 ± 5.0%; sustained hypertension group, 9.1 ± 5.4%; P = 0.22; Fig. 1c).
ROC curve analyses to determine the discriminative power of FMD and NID to diagnose patients with sustained hypertension revealed that the optimal cutoff value of FMD to diagnose patients with sustained hypertension was 6.8% with an AUC value of 0.51 (Fig. 2b) and that of NID was 8.9% with an AUC value of 0.58 (Fig. 2c).
Discussion
In the present study, we demonstrated that baPWV was significantly higher in treated patients with sustained hypertension than in those without sustained hypertension, whereas there were no significant differences in FMD and NID between treated patients with and without sustained hypertension. baPWV above the cutoff value of 1858 cm/s, derived from ROC curve analysis, was significantly associated with sustained hypertension even after adjustment for other cardiovascular risk factors and confounding factors. To our knowledge, this is the first report in which the associations of home blood pressure assessed by home blood pressure monitoring with results of multiple vascular function tests were assessed and the first study showing a significant association between sustained hypertension and baPWV, an index of arterial stiffness, in patients receiving antihypertensive drugs. Although the relationship between out-of-office blood pressure and vascular function has been investigated in a general population [16], in patients with essential hypertension including those not receiving antihypertensive drugs [17], in patients with type 2 diabetes [18], and in patients with one or more cardiovascular risk factors [19], there is little information on the relationship between out-of-office blood pressure and vascular function in patients receiving antihypertensive drugs.
baPWV has been shown to correlate closely with directly measured aortic PWV and carotid-femoral PWV (cfPWV), the gold standard for a non-invasive approach for the assessment of central arterial stiffness [20, 21]. Recent meta-analyses have shown that the hazard risk for the development of cardiovascular disease increases linearly with an increase in baPWV independently from traditional cardiovascular risk factors, indicating that baPWV is not only an index of arterial stiffness but also an independent predictor for cardiovascular events [15, 22]. In the present study, baPWV was significantly higher in treated patients with sustained hypertension than in those without sustained hypertension. In addition, multivariate analysis revealed that sustained hypertension was significantly associated with baPWV even after adjustment for other cardiovascular risks factors and confounding factors of baPWV, including age, brachial systolic blood pressure at baPWV measurement, heart rate, and body mass index [23, 24]. Although, to our knowledge, there has been no study on the relationship between out-of-office blood pressure status stratified according to daytime and night-time blood pressures and risk for the development of cardiovascular disease in patients receiving antihypertensive drugs, these findings suggest that patients with sustained hypertension may have higher rates of cardiovascular morbidity and mortality than those without sustained hypertension in treated patients with hypertension.
In the present study, ROC curve analysis revealed that the optimal cutoff value of baPWV to diagnose patients with sustained hypertension was 1858 cm/s (AUC value, 0.74). In addition, baPWV above the cutoff value of 1858 cm/s was significantly associated with sustained hypertension in treated patients with hypertension even after adjustment for other confounding factors. Recent studies have shown that increased baPWV is a significant predictor of new onset of hypertension in subjects without hypertension [25]. Although the cross-sectional design of the present study did not allow us to investigate a causal relationship between baPWV and sustained hypertension, these findings suggest that increased arterial stiffness is associated not only with the development of hypertension but also with maintenance of an elevated blood pressure condition in treated patients with hypertension.
The results of ROC curve analysis also demonstrated the potential usefulness of baPWV measurement for selecting candidates for whom assessment of night-time blood pressure should be performed. Home blood pressure monitoring for the assessment of night-time blood pressure is still often burdensome because of sleep disturbances caused by cuff occlusion during sleep [26]. Therefore, it is practically difficult to perform measurement of out-of-office night-time blood pressure in all patients receiving antihypertensive drugs. Assessment of night-time blood pressure should be recommended for treated hypertensives with baPWV above 1858 cm/s in order to identify patients with sustained hypertension for further cardiovascular risk assessment in patients receiving antihypertensive drugs.
FMD of the brachial artery has been widely used for assessment of endothelial function in humans [27, 28]. Measurement of NID of the brachial artery is usually performed for assessment of endothelium-independent vasodilation as a control test for FMD. Recent studies have shown that NID per se is impaired in patients with multiple cardiovascular risk factors or established cardiovascular disease, suggesting that not only FMD but also NID could be used as a vascular biomarker [29, 30]. Although measurements of FMD and NID were performed in patients with hypertension in previous studies, there is little information on the associations of home blood pressure status with FMD and NID in patients receiving antihypertensive drugs [31,32,33]. The present study showed that there was no significant association between out-of-office systolic blood pressure and FMD, the mean value of which was 2.0%. Considering the results of a cross-sectional study conducted in 4533 Japanese subjects showing that normal reference values of FMD were 6.5% in men and 7.4% in women [34], these findings suggest that FMD is impaired regardless of the achieved clinic systolic blood pressure and out-of-office systolic blood pressure in treated patients with hypertension.
In the present study, although NID correlated significantly with morning systolic blood pressure and night-time systolic blood pressure, there was no significant association between home blood pressure status and NID in patients receiving antihypertensive drugs. We previously reported that the mean value of NID in subjects without cardiovascular risk factors was 15.3% [30], suggesting that NID is also impaired regardless of the home blood pressure status in treated patients with hypertension. There is a paucity of data on the relationship between blood pressure and NID in patients with hypertension. Further studies are needed to investigate the role of NID as a vascular biomarker in treated patients with hypertension.
In the present study, baPWV was significantly higher in patients with sustained hypertension than in patients without sustained hypertension, whereas there were no significant associations of home blood pressure status with FMD and NID in patients receiving antihypertensive drugs. Recent epidemiological studies have demonstrated that patients receiving antihypertensive drugs have a higher cardiovascular risk than those not receiving antihypertensive drugs regardless of the achieved clinical blood pressure levels, indicating that patients receiving antihypertensive drugs should be regarded as a high risk group for cardiovascular events with advanced atherosclerosis [3,4,5,6]. Endothelial dysfunction and vascular smooth muscle dysfunction may occur at an early stage of atherosclerosis than arterial stiffening do. Therefore, it is postulated that FMD and NID are already impaired in patients receiving antihypertensive drugs, leading to lower FMD and NID regardless of out-of-office blood pressure status. In addition, we cannot deny the possibility that ability of the brachial artery to dilate in response to shear stress or exogenous nitric oxide is chronically altered by long-term use of vasoactive medications, making FMD and NID of no use for the assessment of vascular function in patients receiving antihypertensive drugs.
Although we did not know the precise reasons for more frequent use of β-blockers in the sustained hypertension group, it may be due to higher prevalence of patients with coronary heart disease in the sustained hypertension group, for whom use of β-blockers is recommended for the secondary prevention [7].
There is a limitation in the present study. baPWV measures velocity over a long arterial path, including peripheral muscular arteries, which may be influenced by sympathetic tone. Therefore, we cannot deny the possibility that baPWV may be confounded by the presence of sympathetic activity, which may also contribute to sustained hypertension. Although data on the index of sympathetic activity, such as power spectrum analysis of heart rate variability, would enable more specific conclusion to be drawn regarding the association between baPWV and sustained hypertension, we have no information on the index of sympathetic activity. Further studies are needed to investigate the associations of sympathetic activity with baPWV and sustained hypertension.
In conclusion, baPWV was significantly higher in patients with sustained hypertension than in those without sustained hypertension, whereas there was no significant difference in FMD or NID between patients with and those without sustained hypertension who were receiving antihypertensive drugs. Increased arterial stiffness may contribute to sustained hypertension in patients receiving antihypertensive drugs. Arterial stiffness may be a potential therapeutic target for sustained hypertension to reduce residual risk in patients receiving antihypertensive drugs. Further studies are needed to determine whether aggressive antihypertensive interventions targeting nocturnal hypertension improve baPWV and lower cardiovascular morbidity and mortality rates in patients receiving antihypertensive drugs.
References
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, et al. The preventable causes of death in the united states: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43.
Psaty BM, Furberg CD, Kuller LH, Cushman M, Savage PJ, Levine D, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–92.
Chambless LE, Folsom AR, Sharrett AR, Sorlie P, Couper D, Szklo M, et al. Coronary heart disease risk prediction in the atherosclerosis risk in communities (aric) study. J Clin Epidemiol. 2003;56:880–90.
D’Agostino RB Sr., Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:743–53.
Asayama K, Satoh M, Murakami Y, Ohkubo T, Nagasawa SY, Tsuji I. et al. Evidence for Cardiovascular Prevention from observational cohorts in Japan Research Group Cardiovascular risk with and without antihypertensive drug treatment in the Japanese general population: participant-level meta-analysis. Hypertension. 2014;63:1189–97.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. Japanese Society of Hypertension Committee for Guidelines for the management of hypertyension(JSH 2014). Hypertens Res. 2014;37:253–390.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in ohasama, Japan. J Hypertens. 1998;16:971–5.
Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M, de la Cruz JJ, et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. New Engl J Med. 2018;378:1509–20.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K. et al.International database on ambulatory blood pressure monitoring in relation to cardiovascular outcomes investigators Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cifkova R, Cosentino F, et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the european society of cardiology working group on peripheral circulation: endorsed by the association for research into arterial structure and physiology (artery) society. Atherosclerosis. 2015;241:507–32.
Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman. A Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4:e002270.
Kajikawa M, Maruhashi T, Hida E, Iwamoto Y, Matsumoto T, Iwamoto A, et al. Combination of flow-mediated vasodilation and nitroglycerine-induced vasodilation is more effective for prediction of cardiovascular events. Hypertension. 2016;67:1045–52.
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y. et al.Collaborative Group for J-BAVEL Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension. 2017;69:1045–52.
Li Y, Staessen JA, Lu L, Li LH, Wang GL, Wang JG. Is isolated nocturnal hypertension a novel clinical entity? Findings from a chinese population study. Hypertension. 2007;50:333–9.
Alioglu E, Turk UO, Bicak F, Tengiz I, Atila D, Barisik V, et al. Vascular endothelial functions, carotid intima-media thickness, and soluble cd40 ligand levels in dipper and nondipper essential hypertensive patients. Clin Res Cardiol. 2008;97:457–62.
Wijkman M, Lanne T, Engvall J, Lindstrom T, Ostgren CJ, Nystrom FH. Masked nocturnal hypertension--a novel marker of risk in type 2 diabetes. Diabetologia. 2009;52:1258–64.
Kario K, Hoshide S, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S. et al.J-HOP study group Sleep blood pressure self-measured at home as a novel determinant of organ damage: Japan morning surge home blood pressure (J-HOP) study. J Clin Hypertens. 2015;17:340–8.
Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA, et al. Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Human Hypertens. 2005;19:401–6.
Tanaka H, Munakata M, Kawano Y, Ohishi M, Shoji T, Sugawara J, et al. Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J Hypertens. 2009;27:2022–7.
Vlachopoulos C, Aznaouridis K, Terentes-Printzios D, Ioakeimidis N, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysis. Hypertension. 2012;60:556–62.
Yamashina A, Tomiyama H, Arai T, Koji Y, Yambe M, Motobe H, et al. Nomogram of the relation of brachial-ankle pulse wave velocity with blood pressure. Hypertens Res. 2003;26:801–6.
Lantelme P, Mestre C, Lievre M, Gressard A, Milon H. Heart rate: an important confounder of pulse wave velocity assessment. Hypertension. 2002;39:1083–7.
Tomiyama H, Komatsu S, Shiina K, Matsumoto C, Kimura K, Fujii M, et al. Effect of wave reflection and arterial stiffness on the risk of development of hypertension in japanese men. J Am Heart Assoc. 2018;7:e008175.
Hosohata K, Kikuya M, Ohkubo T, Metoki H, Asayama K, Inoue R, et al. Reproducibility of nocturnal blood pressure assessed by self-measurement of blood pressure at home. Hypertens Res: Off J Jpn Soc Hypertens. 2007;30:707–12.
Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–5.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8.
Adams MR, Robinson J, McCredie R, Seale JP, Sorensen KE, Deanfield JE, et al. Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol. 1998;32:123–7.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol. 2013;33:1401–8.
Gokce N, Holbrook M, Duffy SJ, Demissie S, Cupples LA, Biegelsen E, et al. Effects of race and hypertension on flow-mediated and nitroglycerin-mediated dilation of the brachial artery. Hypertension. 2001;38:1349–54.
Iiyama K, Nagano M, Yo Y, Nagano N, Kamide K, Higaki J, et al. Impaired endothelial function with essential hypertension assessed by ultrasonography. Am Heart J. 1996;132:779–82.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Endothelial function is impaired in patients receiving antihypertensive drug treatment regardless of blood pressure level: FMD-J Study (flow-mediated dilation Japan). Hypertension. 2017;70:790–7.
Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, et al. Reliability of measurement of endothelial function across multiple institutions and establishment of reference values in Japanese. Atherosclerosis. 2015;242:433–42.
Acknowledgements
We thank Megumi Wakisaka, Miki Kumiji, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Funding
Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to YH) and a Grant in Aid of Japanese Arteriosclerosis Prevention Fund (to YH).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Appendix
Appendix
Participants and participating centers: Yasuki Kihara, (Hiroshima University), Yoshihiko Kinoshita (Kinoshita Clinic), Ryoji Ozono (Ozono Clinic, Internal Medicine and Cardiology), Mitsuaki Nakamaru (Nakamaru Clinic), Masanori Ninomiya (Ninomiya Clinic), Jiro Oiwa (Oiwa Naika), Kotaro Sumii (Mazda Hospital), Narimasa Miho (Mazda Hospital), Takuji Kawagoe (Kawagoe Clinic of Cardiology), Kousuke Takahari (Shobara City Soryo Clinic), Osamu Yoshida (Yoshida Cardiology Clinic), Yasuhiko Hayashi (Tsuchiya General Hospital), Tomokazu Okimoto (Tsuchiya General Hospital), Yujiro Ono (Higashi-Hiroshima Medical Center), Hikari Jo (Higashi-Hiroshima Medical Center), Hiroshi Tsushima (Higashi-Hiroshima Medical Center), Yasuo Fukunaga (Fukunaga Cardiology Clinic), Nobuo Shiode (Hiroshima City Hiroshima Citizens Hospital), Tadanao Higaki (Hiroshima City Hiroshima Citizens Hospital), Hiroki Mitsuda (Mitsuda Clinic), Toshiyuki Matsumoto (Matsumoto Cardiovascular Medical Clinic), Hiroshi Sugino (National Hospital Organization Kure Medical Center and Chugoku Cancer Center), Hironori Ueda (Hiroshima Prefectural Hospital), Naoya Mitsuba (Hiroshima Prefectural Hospital), Hideo Matsuura (Saiseikai Kure Hospital), Koji Kido (Saiseikai Kure Hospital), Kentaro Ueda (Ueda Hatchobori Clinic), Koji Matsumoto (Saiseikai Hiroshima Hospital), Mitsuaki Watanabe (Saiseikai Hiroshima Hospital), Tatsuya Maruhashi (Hiroshima University), Masato Kajikawa (Hiroshima University), Shinji Kishimoto (Hiroshima University), Shogo Matsui (Hiroshima University), Haruki Hashimoto (Hiroshima University),Yuji Takaekou (Hiroshima University), Yoshiki Aibara (Hiroshima University), Farina Mohamad Yusoff (Hiroshima University), Takayuki Hidaka (Hiroshima University), Kazuaki Chayama (Hiroshima University), Kensuke Noma (Hiroshima University), Ayumu Nakashima (Hiroshima University), Chikara Goto (Hiroshima International University), Masakazu Takahashi (Yamaguchi University), Yukihito Higashi (Hiroshima University).
Rights and permissions
About this article
Cite this article
Maruhashi, T., Kinoshita, Y., Kajikawa, M. et al. Relationship between home blood pressure and vascular function in patients receiving antihypertensive drug treatment. Hypertens Res 42, 1175–1185 (2019). https://doi.org/10.1038/s41440-019-0240-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0240-8
Keywords
This article is cited by
-
Comparison of the usefulness of the cardio-ankle vascular index and augmentation index as an index of arteriosclerosis in patients with essential hypertension
Hypertension Research (2022)
-
Predictive power of home blood pressure measurement for cardiovascular outcomes in patients with type 2 diabetes: KAMOGAWA-HBP study
Hypertension Research (2021)