Abstract
Background
Choroidal tuberculoma is possibly the most unequivocal manifestation of ocular infection with Mycobacterium tuberculosis. Here, we investigate the need for adjunctive corticosteroids in the management of this infection. We have compared the efficacy of anti-tubercular therapy (ATT) with or without oral corticosteroids, in management of choroidal tuberculoma.
Methods
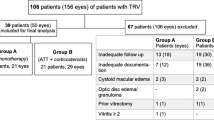
We report a retrospective, observational study of patients treated with ATT for choroidal tuberculoma. Group A patients were treated with standard 6-month ATT alone, and Group B with ATT and oral corticosteroids, with/without intravitreal triamcinolone/ bevacizumab injections. Primary outcome measure was time to complete resolution of lesions. Secondary measures were time to first sign of resolution and change in best corrected visual acuity (BCVA) at final visit.
Results
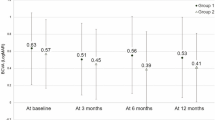
Fourteen patients were included in the study—seven in Group A and seven in Group B. Both groups had similar duration of symptoms and size of lesions but not baseline BCVA (p = 0.02). Perilesional fluid was noted in all eyes in each group. Mean time to complete resolution in group A was 1.89 ± 0.28 (range 1.25–2) months, significantly lesser than group B (5.17 ± 2.64 [range 2–9] months, p = 0.005, Mann–Whitney test). Mean time to first sign of resolution (range from 5 days to 10 weeks, p = 0.35) and mean change in BCVA between presentation and final follow up (p = 0.2) were comparable between both groups.
Conclusion
Anti-TB monotherapy alone, may be sufficient for resolution of at least, select cases of choroidal tuberculoma, without the need for adjunctive corticosteroids.
Similar content being viewed by others
Introduction
Ocular tuberculosis (TB) has several clinical manifestations, majority of which continue to have tenuous associations with Mycobacterium tuberculosis (Mtb) infection in the eye [1]. Amongst all the ocular TB manifestations, tubercular choroidal granuloma or choroidal tuberculoma stands out due to its strong association with Mtb infection in the eye. It is commonly found in disseminated systemic TB [2, 3], several histopathological studies have documented granulomatous inflammation and acid-fast bacilli in the choroidal lesions [4,5,6], and guinea pigs infected with aerosolised Mtb develop choroidal granulomas in the eye [7]. Thus, choroidal tuberculoma probably represent the most “direct” manifestation of ocular TB.
Despite such apparently direct associations, the lack of accurate diagnostic tests, variations in clinical presentations, and differences in treatment response, have deterred the development of clear diagnostic and therapeutic protocols for choroidal tuberculoma [8, 9]. Recently, the Collaborative Ocular TB Study (COTS) reported consensus guidelines for initiating anti-TB therapy (ATT) in different clinical presentations of TB choroiditis [10]. These guidelines strongly recommended (96.2% consensus) adjunctive therapy with oral corticosteroids, for treatment of choroidal tuberculoma not associated with systemic TB [10]. While it is understandable that general guidelines cannot be all-inclusive, our own experience and that of others, suggests that patients presenting with select forms of ocular TB can respond to anti-TB monotherapy without any need for adjunctive corticosteroids [11, 12].
Indeed, there is no conclusive evidence yet, of the utility of adjunctive corticosteroids, in different forms of ocular, or even systemic TB. Individual studies as well as systematic meta-analysis, have not been able to demonstrate any beneficial effect of concurrent corticosteroid therapy in ocular TB [13, 14]. Even in TB of other organ systems, the role of adjunctive corticosteroids has been questioned [15, 16]. Thus, the proposed guidelines for treatment of choroidal tuberculoma need a thorough reappraisal. This is significant since our understanding of the exact pathomechanisms in different forms of ocular TB continue to be equivocal [17, 18]. While histopathological studies of human and animal eyes suggest the role of direct mycobacterial infection [2,3,4,5,6,7], cytokine analyses and cell-based studies from intraocular fluids, have also suggested an autoimmune pathology [19, 20]. While direct infection may be treated by ATT alone, the resolution of autoimmunity mediated inflammation would primarily require anti-inflammatory therapy. In the current study, we have reviewed the presenting features of patients with choroidal tuberculoma and compared treatment outcomes of anti-TB monotherapy with combination therapy of ATT and corticosteroids.
Methods
We retrospectively reviewed electronic medical records of consecutive patients diagnosed as choroidal tuberculoma between January 2014 to June 2019, at LV Prasad Eye Institute, Bhubaneswar, a tertiary eye care centre in eastern India. The following diagnostic keywords were used: choroiditis, tuberculosis, tuberculoma, and choroidal granuloma. The study was approved by the institutional review board (IRB) and adhered to the guidelines of the Declaration of Helsinki. Since this was a retrospective observational study, the need for an informed consent was waived by the IRB. We divided cases into two groups: Group A comprising of patients treated with ATT monotherapy; and Group B, where ATT was combined with oral steroids ± local corticosteroid/anti-VEGF therapy. Only patients with complete ocular examination including best-corrected visual acuity (BCVA), slit lamp examination, intraocular pressures, and fundus photography (seven-fields montage images) on all visits, were included in the study. The diagnosis of choroidal tuberculoma was made on basis of clinical recognition of a choroidal granuloma ≥1 disc diameter (DD); ancillary tests for systemic TB infection such as tuberculin skin test (TST) and/or QuantiFERON TB Gold test (QFT); radiological signs of healed or active pulmonary TB (PTB); and exclusion of non-TB entities. We did not combine the results of TST and QFT, which has been reported to have superior diagnostic accuracy for ocular TB than testing them in isolation [21]. All patients were specifically enquired about history of recent contact with PTB and received a thorough physician evaluation for any evidence of pulmonary or extrapulmonary TB (EPTB).
The clinical recognition of choroidal tuberculoma was based on the presence of elevated, sub-retinal, yellowish white mass lesion with perilesional subretinal fluid (SRF), with or without exudative retinal detachment (RD) (Fig. 1). Ocular imaging with B-scan ultrasonography, fundus fluorescence angiography (FFA), indocyanine green angiography (ICGA) and optical coherence tomography (OCT) was considered, either to rule out a differential diagnosis or to document additional inflammatory signs such as exudative RD or cystoid macular oedema (CMO). The ATT regimen used in either group consisted of isoniazid, rifampicin, pyrazinamide and ethambutol (HRZE) in induction phase of 2 months followed by maintenance phase of 4 months with isoniazid and rifampicin (HR). ATT therapy was monitored by an internist with periodic complete blood count and liver function test over 6 months. Supplemental oral vitamin B-complex was administered for pyridoxine supplementation. Oral prednisolone, when considered, were started at a dose of 1 mg/kg/day with a maximum daily dose of 60 mg. The tapering schedule for corticosteroids was as per earlier guidelines [22]. Intravitreal injections of triamcinolone acetonide (2 mg/0.05 cc) and/or bevacizumab (1.25 mg/0.05 cc) were given in eyes with clinically inadequate response to three weeks of full dose corticosteroids.
A Colour fundus photograph of the right eye of patient #1, group A (Table 1), showing two large, yellowish white subretinal lesions, with overlying exudative retinal detachment. Disc hyperaemia is also seen. B Fluorescein angiogram (arteriovenous phase) of the same eye showing intra-lesional hyperfluorescence and peri- and intra-lesional hypofluorescence (arrowheads)corresponding to the two lesions. C Optical coherence tomography vertical line scan running through both lesions, showing dome-shaped elevation of the choroid with sub-retinal hyper-reflective material (‘contact sign’, arrow) and perilesional fluid. D Two weeks following initiation of anti-TB monotherapy, showing significant reduction in size of lesion (E) Five weeks after treatment, near total resolution of both lesions, along with overlying exudation.
The first signs of resolution of lesion were defined presence of one of the following signs: clinical reduction in size or thickness of lesion, rounding of lesion margins, decrease in exudative RD; OCT features of decrease in SRF, resolution of intraretinal fluid. Complete resolution of tuberculoma was defined as resolution of the choroidal lesions, and subretinal fluid, accompanied by choroidal atrophy, pigmentation and/or fibrosis. Primary outcome measure was the time to complete resolution of tuberculoma in each group. Secondary outcome measures were time to first sign of resolution and mean change in BCVA at final follow up.
Statistical analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected, a non-parametric test was used. Statistical tests were applied as follows:
-
1.
Quantitative variables were compared using independent t-test or Mann-Whitney Test (when the data sets were not normally distributed) between the two groups.
-
2.
Qualitative variables were compared using Fisher’s Exact test.
-
3.
Kaplan–Meier survival analysis curve was used for time of resolution and log rank test was used for comparison between two groups.
A p value of <0.05 was considered statistically significant. The data was entered in MS Excel spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
We retrieved data of 18 patients, who were diagnosed as choroidal tuberculoma during the study period. Three patients were excluded due absence of any evidence of systemic TB. One patient was excluded due to inadequate follow up. Finally, 14 patients (14 eyes) were included into the study. Group A (n = 7) was treated with ATT monotherapy, and group B (n = 7) with ATT and oral corticosteroid combination therapy. The summary data of baseline demographic features, clinical presentations and treatment outcomes is listed in Table 1.
The mean age, gender and duration of symptoms, were comparable between both groups. Thirteen patients (92.6%) were investigated with contrast-enhanced computerised tomography (CECT) of thorax, which revealed active PTB in three patients (two in group A and one in group B) and healed PTB in four. The remaining six (46.2%) patients had normal scans. One received a chest X-ray, which were normal. One patient had been diagnosed with pulmonary TB (PTB) prior to presentation to our clinic (group A, #4). Majority of tuberculomas (n = 5) in group A were located at the posterior pole, while in group B, three were located at the posterior pole and four at the periphery. One eye in each group had two tuberculomas (Fig. 1); all other eyes in both groups had solitary lesions. The tuberculoma involved the optic disc in two eyes in group A and three in group B. All eyes with disc involvement had peripapillary splinter haemorrhages. One eye in group A, also had deep retinal haemorrhages overlying the tuberculoma. All eyes in both groups showed presence of perilesional fluid, either clinically or on OCT (Fig. 1C). However, dense vitritis (≥grade 2) was seen in three group B eyes, but none in group A (p = 0.21).
We noted additional inflammatory lesions, in the study or fellow eye, apart from the primary lesion. Among the study eyes, two (one in each group) showed active multifocal yellowish-white lesions (<1 DD size), which healed without pigmentation during resolution of the primary lesion. Old, pigmented chorioretinal scars were also seen in two study eyes. Amongst the fellow eyes, one patient (#3, group B) had active choroiditis (<1 DD size) lesions. Healed chorioretinal scars were noted in four fellow eyes – non-pigmented in three and pigmented in one eye.
B-scan ultrasonography was done in four eyes (two in each group) and consistently showed dome shaped elevations, with medium surface reflectivity and low to medium internal reflectivity. FFA was performed in five eyes at baseline – four in group A and one in group B. In all eyes, patchy choroidal hypofluorescence was noted in choroidal to arterial phase, which changed to intralesional hyperfluorescence and perilesional hypofluorescence in the arteriovenous phase (Fig. 1B). Pooling of dye into the sub-retinal space was seen in the late phase. The perilesional hypofluorescence surrounded the intralesional hyperfluorescence and persisted till the end of the angiogram. ICGA was performed in two patients—one in each group. Both eyes showed early phase hypofluorescence corresponding to the lesion, which persisted in the mid- and late phases. Fellow eye of one patient revealed small hypofluorescent choroidal lesions on ICGA, which were not apparent on clinical examination. None of the angiograms showed any evidence of retinochoroidal anastomosis, either on FFA or ICGA. OCT was performed in 10 eyes (7 in group A and 3 in group B). All showed presence of sub-retinal hyperreflective material (SHRM) with a surrounding cuff of sub-retinal fluid (Fig. 1C). This OCT appearance has been termed as “contact sign” in earlier studies [23]. Intra-retinal cystic spaces were found in all scans except three in group A. Thickening of the RPE with distortion of ellipsoid layer overlying the tuberculoma, was also noted in all eyes.
Response to therapy
All eyes in group A, and all but one in group B, showed complete resolution of the lesion, before the end of the follow up period (Fig. 1). The only exception in group B was one eye that had persistent exudative RD at final follow-up (6 months) even though the primary lesion healed. The mean time to first sign of resolution (range from 5 days to 10 weeks) was comparable between both groups (p = 0.345). The mean time for complete resolution in group A was 1.89 ± 0.28(1.25–2) months which was significantly less as compared to 5.17 ± 2.64 (2-9) months in group B (p = 0.005, Mann–Whitney test). Kaplan–Meier survival analysis showed that at 2 months post ATT, 100% eyes (n = 7) in group A had complete resolution, compared to 14.29% (n = 1) in group B. The group B value increased to 42.8% at the end of 4 months. The estimated median time to complete resolution was significantly less with group A compared to group B (p = 0.002, log rank test). Finally, the mean increases in BCVA (logMAR) between presentation and final follow up was comparable between group A (0.67) and group B (1.24) (p = 0.196). At resolution, circumscribed RPE atrophy was noted corresponding to the location of the lesion, in all eyes. This was associated with pigmentation in one eye in group A, and five eyes in group B. The types of pigmentation observed in group B eyes included blotchy pigmentation (n = 2), hypertrophic RPE band (n = 2) and pigmentation around central fibrotic scar (n = 1).
Discussion
Our study demonstrates the efficacy of anti-TB monotherapy in resolution of select cases of choroidal tuberculoma. It is possible that in such cases, the resolution with monotherapy can be faster than combination therapy with adjunctive corticosteroids, without compromising the visual outcome in these patients.
The role of corticosteroids in treatment of TB has been studied ever since the introduction of ATT in the 1940s [24]. However, controlled trial evidence for the benefits of corticosteroids is available for only two forms of TB – meningitis and pericarditis [25, 26]. Here too, the benefits have been noted in terms of survival rates, and not necessarily functional outcomes. For other forms of TB, including pulmonary TB, the beneficial effects of corticosteroids, have remained questionable [15, 16]. Even in TB meningitis, adjunctive dexamethasone was not found to have any effect on peripheral monocyte or local T-cell responses, or on radiological appearance of lesions [27, 28]. In the case of ocular TB, a systematic meta-analysis did not show any difference in outcome between those treated with ATT alone or in combination with corticosteroids [14]. The COTS study showed variations in use of combination therapy for ocular TB in different geographical locations, ranging from >80% in Asia and the Middle East, to ~60% in Australia and Western countries [13].
There could be several explanations for such incongruity in the treatment patterns of ocular TB. One reason could be the uncertainty in aetiological diagnosis of TB in majority of cases of ocular TB prompting physicians to add corticosteroids to the treatment regimen. Another factor could be the differences between genetic backgrounds of patients. An example is the polymorphism in a gene that encodes leukotriene A4 hydrolase (LTA4H), an enzyme determines the balance between proinflammatory and anti-inflammatory eicosanoids [29]. Polymorphisms in the LTA4H gene result in hyperinflammatory or hypoinflammatory phenotypes, the former benefitting from adjunctive corticosteroid therapy, at least in TB meningitis [30]. Conversely, in the hypoinflammatory group, the effect of corticosteroids, could be detrimental. Such polymorphisms could be the reason, why treating ophthalmologists have variable experiences with adjunctive corticosteroids in treating ocular TB in different parts of the world [13].
An additional confounding factor, in the case of ocular TB, is the wide variation in clinical phenotypes of the disease. Some of these phenotypes (e.g., serpiginous-like choroiditis [SLC]) are more likely to cause breakdown of blood-retinal-barriers (BRBs) than others (e.g. choroiditis). We recently reported the presence of autoreactive T-cells (reactive to retinal antigens) in the vitreous of patients with clinically diagnosed ocular TB [20]. The autoreactive T-cells were not only more pro-inflammatory than Mtb antigen-reactive T-cells, but also were resistant to activation-induced cell death, thereby promoting prolonged inflammatory response. It is likely that conditions that disrupt the BRB, such as SLC or chronic disease would have a higher proportion of autoreactive T-cells, and therefore merit adjunctive corticosteroid therapy. Thus, the treatment response in different clinical phenotypes of ocular TB could be multifactorial and the role of adjunctive corticosteroids needs to be investigated by randomised control trials for each phenotype.
Our study is limited by its retrospective nature and the small number of patients in each group. It is relevant to note here that tuberculoma are relatively rare in ophthalmic practice, and more common in multi-specialty practices. However, there remains a strong possibility of selection bias in our study whereby patients with larger lesions, exudative RD or increased vitritis, were treated with adjunctive corticosteroids. This selection bias may have been masked during statistical comparison between the two groups due to the small sample size of each group (Table 1). All the patients in our study received 6 months of ATT, even though previous studies have supported a longer duration of therapy [31]. However, the duration of ATT was probably irrelevant in our case, as all the tuberculoma healed prior to the completion of ATT. We may have missed some of the variations in choroidal tuberculoma, such as highly vascular tumours, that are known to benefit from local anti-vascular endothelial growth factor therapy [32, 33]. Finally, we cannot discount the inherent anti-inflammatory properties of rifampicin [34], which have found use in dermatological conditions [35]. However, it is unlikely, that these anti-inflammatory properties alone would be sufficient to induce resolution of large choroidal tuberculoma.
In conclusion, our study demonstrates the efficacy of ATT monotherapy, at least in select cases of choroidal tuberculoma. Its significance lies in the relatively linear relationship of this phenotype with ocular Mtb infection. Clear understanding of treatment outcomes in choroidal tuberculoma will greatly facilitate future studies for other phenotypes of ocular TB.
Summary
What was known before
-
Choroidal tuberculoma is caused by Mycobacterium tuberculosis. Choroidal tuberculoma resolves on treatment with anti-TB therapy.
What this study adds
-
Anti-TB monotherapy, without adjunctive corticosteroids, is sufficient for treatment of choroidal tuberculoma. Monotherapy may lead to faster resolution of lesions without compromising visual outcomes
References
Ang M, Chee SP. Controversies in ocular tuberculosis. Br J Ophthalmol. 2017;101:6–9. https://doi.org/10.1136/bjophthalmol-2016-309531.
Sharma PM, Singh RP, Kumar A, Prakash G, Mathur MB, Malik P. Choroidal tuberculoma in miliary tuberculosis. Retina. 2003;23:101–4. https://doi.org/10.1097/00006982-200302000-00018.
Heiden D, Saranchuk P, Keenan JD, Ford N, Lowinger A, Yen M, et al. Eye examination for early diagnosis of disseminated tuberculosis in patients with AIDS. Lancet Infect Dis. 2016;16:493–9. https://doi.org/10.1016/S1473-3099(15)00269-8.
Lyon CE, Grimson BS, Peiffer RL Jr, Merritt JC. Clinicopathological correlation of a solitary choroidal tuberculoma. Ophthalmology. 1985;92:845–50.
Barondes MJ, Sponsel WE, Stevens TS, Plotnik RD. Tuberculous choroiditis diagnosed by chorioretinal endobiopsy. Am J Ophthalmol. 1991;112:460–1. https://doi.org/10.1016/s0002-9394(14)76260-9.
Wroblewski KJ, Hidayat AA, Neafie RC, Rao NA, Zapor M. Ocular tuberculosis: a clinicopathologic and molecular study. Ophthalmology. 2011;118:772–7. https://doi.org/10.1016/j.ophtha.2010.08.011.
Rao NA, Albini TA, Kumaradas M, Pinn ML, Fraig MM, Karakousis PC. Experimental ocular tuberculosis in guinea pigs. Arch Ophthalmol. 2009;127:1162–6.
Ang M, Vasconcelos-Santos DV, Sharma K, Accorinti M, Sharma A, Gupta A, et al. Diagnosis of ocular tuberculosis. Ocul Immunol Inflamm. 2018;26:208–16.
Petrushkin H, Sethi C, Potter J, Martin L, Russell G, White V, et al. Developing a pathway for the diagnosis and management of ocular tuberculosis. The pan-LOndon ocular tuberculosis pathway-LOOP. Eye. 2020;34:805–8.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Kon OM et al. Collaborative Ocular Tuberculosis Study Consensus Guidelines on the Management of Tubercular Uveitis—Report 1. Ophthalmology. 2020;S0161-6420 30013-0. (published ahead of print). https://doi.org/10.1016/j.ophtha.2020.01.008.
Nahon-Esteve S, Martel A, Maschi C, Alketbi M, Baillif S, Tieulie N Uveitis associated with latent tuberculosis: a comparative study of the impact of antitubercular therapy combined or not with systemic corticosteroids. Eur J Ophthalmol. 2020:1120672120962066. https://doi.org/10.1177/1120672120962066. Epub ahead of print.
Zhang M, Zhang J, Liu Y. Clinical presentations and therapeutic effect of presumed choroidal tuberculosis. Retina. 2012;32:805–13. https://doi.org/10.1097/IAE.0b013e3182215b5e.
Agrawal R, Gunasekeran DV, Raje D, Agarwal A, Nguyen QD, Kon OM, et al. Global variations and challenges with tubercular uveitis in the collaborative ocular tuberculosis study. Invest Ophthalmol Vis Sci. 2018;59:4162–71. https://doi.org/10.1167/iovs.18-24102.
Kee AR, Gonzalez-Lopez JJ, Al-Hity A, Gupta B, Lee CS, Gunasekeran DV, et al. Anti-tubercular therapy for intraocular tuberculosis: a systematic review and meta-analysis. Surv Ophthalmol 2016;61:628–53. https://doi.org/10.1016/j.survophthal.2016.03.001.
Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis. 1997;25:872–87. https://doi.org/10.1086/515543.
Thwaites GE. Adjunctive corticosteroids for all forms of tuberculosis? Lancet Infect Dis. 2013;13:186–8. https://doi.org/10.1016/S1473-3099(13)70009-4.
Forrester JV, Kuffova L, Dick AD. Autoimmunity, autoinflammation, and infection in uveitis. Am J Ophthalmol. 2018;189:77–85.
Basu S, Elkington P, Rao N. Pathogenesis of ocular tuberculosis—new observations and future observations. Tuberculosis. 2020;124:101961.
Ang M, Cheung G, Vania M, Chen J, Yang H, Li J, et al. Aqueous cytokine and chemokine analysis in uveitis associated with tuberculosis. Mol Vis. 2012;18:565–73.
Tagirasa R, Parmar S, Barik MR, Devadas S, Basu S. Autoreactive T cells in immunopathogenesis of TB-associated uveitis. Invest Ophthalmol Vis Sci 2017;58:5682–91. https://doi.org/10.1167/iovs.17-22462.
Ang M, Wong WL, Li X, Chee SP. Interferon γ release assay for the diagnosis of uveitis associated with tuberculosis: a Bayesian evaluation in the absence of a gold standard. Br J Ophthalmol. 2013;97:1062–7.
Jabs DA. Immunosuppression for the uveitides. Ophthalmology. 2018;125:193–202. https://doi.org/10.1016/j.ophtha.2017.08.007.
Salman A, Parmar P, Rajamohan M, Vanila CG, Thomas PA, Jesudasan CA. Optical coherence tomography in choroidal tuberculosis. Am J Ophthalmol. 2006;142:170–2. https://doi.org/10.1016/j.ajo.2006.01.071.
Ashby M, Grant H. Tuberculous meningitis treated with cortisone. Lancet. 1955;268:65–6. https://doi.org/10.1016/s0140-6736(55)90003-9.
Thwaites GE, Nguyen DB, Nguyen HD, Hoang TQ, Do TT, Nguyen TC, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004;351:1741–51. https://doi.org/10.1056/NEJMoa040573.
Hakim JG, Ternouth I, Mushangi E, Siziya S, Robertson V, Malin A. Double blind randomised placebo controlled trial of adjunctive prednisolone in the treatment of effusive tuberculous pericarditis in HIV seropositive patients. Heart. 2000;84:183–8. https://doi.org/10.1136/heart.84.2.183.
Simmons CP, Thwaites GE, Quyen NT, Chau TT, Mai PP, Dung NT, et al. The clinical benefit of adjunctive dexamethasone in tuberculous meningitis is not associated with measurable attenuation of peripheral or local immune responses. J Immunol 2005;175:579–90. https://doi.org/10.4049/jimmunol.175.1.579.
Thwaites GE, Macmullen-Price J, Tran TH, Pham PM, Nguyen TD, Simmons CP, et al. Serial MRI to determine the effect of dexamethasone on the cerebral pathology of tuberculous meningitis: an observational study. Lancet Neurol. 2007;6:230–6. https://doi.org/10.1016/S1474-4422(07)70034-0.
Tobin DM, Vary JC Jr, Ray JP, Walsh GS, Dunstan SJ, Bang ND, et al. The lta4h locus modulates susceptibility to mycobacterial infection in zebrafish and humans. Cell. 2010;140:717–30. https://doi.org/10.1016/j.cell.2010.02.013.
Thuong NTT, Heemskerk D, Tram TTB, Thao LTP, Ramakrishnan L, Ha VTN, et al. Leukotriene A4 hydrolase genotype and HIV infection influence intracerebral inflammation and survival from tuberculous meningitis. J Infect Dis. 2017;215:1020–8. https://doi.org/10.1093/infdis/jix050.
Ang M, Hedayatfar A, Wong W, Chee SP. Duration of anti-tubercular therapy in uveitis associated with latent tuberculosis: a case-control study. Br J Ophthalmol. 2012;96:332–6. https://doi.org/10.1136/bjophthalmol-2011-300209.
Babu K, Murthy PR, Murthy KR. Intravitreal bevacizumab as an adjunct in a patient with presumed vascularised choroidal tubercular granuloma. Eye. 2010;24:397–9. https://doi.org/10.1038/eye.2009.83.
Bansal R, Beke N, Sharma A, Gupta A. Intravitreal bevacizumab as an adjunct in the management of a vascular choroidal granuloma. BMJ Case Rep. 2013;2013:bcr2013200255. https://doi.org/10.1136/bcr-2013-200255.
Păunescu E. In vivo and in vitro suppression of humoral and cellular immunological response by rifampicin. Nature. 1970;228:1188–90. https://doi.org/10.1038/2281188a0.
Pradhan S, Madke B, Kabra P, Singh AL. Anti-inflammatory and immunomodulatory effects of antibiotics and their use in dermatology. Indian J Dermatol. 2016;61:469–81. https://doi.org/10.4103/0019-5154.190105.
Funding
Hyderabad Eye Research Foundation. This study was supported by Hyderabad Eye Research Foundation, L V Prasad Eye Institute, Hyderabad.
Author information
Authors and Affiliations
Contributions
AK: Data collection and analysis; revision of manuscript; final approval. AK: Data collection and analysis; revision of manuscript; final approval. SB: Conception of study; analysis; initial draft and revision of manuscript. All authors approved the submission
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khalsa, A., Kelgaonkar, A. & Basu, S. Anti-TB monotherapy for choroidal tuberculoma: an observational study. Eye 36, 612–618 (2022). https://doi.org/10.1038/s41433-021-01505-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01505-1