Abstract
Purpose
To compare botulinum neurotoxin (BNT) injections to surgery as first-line therapy in large-angle essential infantile esotropia (IE).
Patients and methods
Children between the ages 6 months and 6 years with IE of ≥40 prism dioptres (PD) were randomised to either a maximum of three BNT injections or surgical intervention of bimedial rectus muscle recession for angles ≤60 PD and augmented with BNT injection in angles >60 PD. Time taken for each procedure was documented. Orthophoria or misalignment of ≤10 PD was regarded as a complete response (CR). Follow-up visits were done at 3, 6, 12 and 24 weeks.
Results
Mean (SD) age and baseline angle of esotropia were 26.9 (14.5) months and 61.9 PD (12.8), respectively, for the overall cohort. The proportion of children who achieved CR was significantly higher in the surgery arm compared to the BNT injection arm (OR = 4.01, 95% CI 1.74–9.22) but the time taken was six times longer (p < 0.0001). In the BNT arm, 55.2% of children aged ≤24 months and 16% of children >24 months achieved CR. In children with esotropia ≤60 PD, CR was achieved in 50% while those with esotropia >60 PD CR was achieved in 25%.
Conclusion
Surgery remains the gold standard for treatment of esotropia but BNT injection is a safe and effective alternative in children ≤24 m and with smaller angles of esotropia ≤60 PD in resource-limited centres.
Similar content being viewed by others
Introduction
Essential infantile esotropia (IE), also referred to as congenital esotropia, has an early onset of approximately 6 months of age. It is characterised by a large angle of deviation and accounts for 8.4% of esotropia cases [1]. Surgical correction is the preferred standard management and is associated with reported success rates between 64 and 80% [2,3,4]. Ing has shown that early surgical intervention and correction of the misalignment may result in the development of stereopsis [5]. In his study, children surgically aligned before 12 months of age developed some degree of stereopsis in 73% and those aligned after 18 months developed stereopsis in 58%. Others have shown that children aligned after 24 months of age did not develop stereopsis [6, 7].
In developing countries like South Africa, IE is reported to be the most common type of strabismus, accounting for 74% of esotropia in childhood [8]. Timeous intervention presents a major challenge in resource-constrained settings such as the public health sector in our country.
Following the introduction by Scott [9] of botulinum neurotoxin injection therapy (BNT) in the treatment of various strabismic conditions, BNT has gained popularity as an alternative treatment option for IE. Results, however, have been mixed. Success rates have varied from 36 to 78% and are related to the degree of strabismus and the age of intervention [10, 11].
The current waiting time for strabismus surgery at our tertiary centre is more than a year from the time of initial presentation and a delay in surgery is known to compromise various aspects of a child’s visual development with regard to fusion and stereopsis [5,6,7] as well as to cause long-term psychosocial issues [12]. A randomised controlled study was undertaken to compare BNT injection to surgical correction as a first-line treatment for large-angle IE. In a Cochrane review, Rowe and Noonan identified six RCT associated with BNT use in strabismus, two in IE and no RCT comparing BNT to surgery in large-angle esotropia [13].
Study methods
A prospective, randomised unblinded study comparing BNT to surgery in IE was conducted from January 2015 to January 2018, in a large tertiary hospital. The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand (Approval no. M140225) and conducted in accordance with the tenets of the Declaration of Helsinki.
Inclusion criteria
Children with onset of esotropia before 6 months of age; with large-angle IE, defined as esotropia of ≥40 prism dioptres (PD), between the ages of 6 months and 6 years at baseline; informed written parental consent.
Exclusion criteria
Children with significant pattern deviation, neurological impairment and hyperopia of >+5.00 dioptres.
Children underwent a full examination including a cycloplegic refraction, fundus examination and orthoptic assessment. Those with a refractive error ≥+2.50 DS were initially given their prescription and if there was no change or minimal change in their esotropic angle, patients were classified as IE and enrolled in the study.
Children were stratified according to two age categories; those ≤24 months and those >24 months. Stratification based on 24 months rather than 12 months was necessary in view of the low enrolment number in the very-young age group and based on previous findings of the potential of developing fusion before and after 24 months [7]. Within each age category, participants were randomised by an independent study assistant and assigned to either the BNT (odd numbers) or surgery (even numbers) arms. Figure 1 shows the schematic randomisation and follow-up.
In the BNT arm, BNT (BotoxTM Allergan) was injected in each medial rectus muscle, administered sub-conjunctively after the muscle was grasped using forceps as described by Benabent et al. [14]. All children received an initial dose of 5 units (U) that was repeated, for a maximum of three injections if the esotropia was >10 PD at visits at 3, 6, 12 or 24 weeks following the last injection. The dosage at subsequent visits depended on the degree of esotropia, 5U for deviations ≥40 PD and 3U for deviations <40 PD.
In the surgical arm, children underwent standard bilateral medial rectus muscle recession surgery for esotropia ≤60 PD. The medial recti were recessed to a maximum of 7 mm with 3U of BNT given intraoperatively to each recessed muscle in cases >60 PD to augment the recessions. No child had three-muscle surgery for the larger angles as an initial procedure.
Participants in both arms were assessed at 3-, 6-, 12- and 24-week post-procedure (patients in the surgery arm were also seen day 1 post-surgery) for possible complications. Children in the BNT arm who had an unacceptable outcome after three injections were offered surgery after a stable angle measurement on two successive visits, 1 month apart. In the surgical arm, all unacceptable outcomes with residual esotropia, received BNT into the recessed muscles at the 6 weeks post-operative visit and surgery as the third procedure if required, once a stable angle was attained on two consecutive visits.
Outcome measure
Complete response (CR) was defined as orthophoria or residual esotropia of ≤10 PD [15], partial response (PR) as residual esotropia of >10 PD and ≤20 PD and deemed acceptable by the parents, and failures or non-response (NR) as >20 PD.
The total theatre time taken for each arm of the study was also recorded.
Sample size
A sample size of 98 (49 per arm) was calculated using a Pearson Chi-squared test with the proportion of success set at 0.65 for the surgery arm and 0.37 for the BNT arm at a power of 80% and an alpha level of 0.05.
Statistical analysis
Data analysis was restricted to children followed up for at least 24 weeks after the last procedure. The Chi-squared test or two-tailed Fisher’s exact test was used to compare binary variables between groups. Continuous variables were analysed using the Wilcoxon rank sum test. Univariate and multivariate logistic regression models were used to assess the effect of intervention adjusting for age and angle of deviation at baseline on the outcome. A p value < 0.05 was considered significant. Statistical analysis was performed using Stata 15.1 (STATA Corp, Texas) and MedCalc (MedCalc Software, Belgium).
Results
Of the 55 children randomised to each arm initially, 101 children, 54 in the BNT arm and 47 in the surgery arm had adequate follow-up of at least 24 weeks after the last procedure. Of the defaulting children, one was in the BNT arm and eight in surgery arm. The mean (SD) age was 26.9 (14.5) months and median (IQR) baseline angle of esotropia was 60 (55–70) PD for the entire cohort with no significant difference between the two arms (Table 1). Total theatre time was significantly shorter for the BNT arm compared to the surgical arm, mean (SD) 11 (1.5) and 72 (5) minutes, respectively, 95% CI 10.46–11.31 and 69.93–74.32, respectively.
As shown in Table 2, CR was achieved in a significantly higher proportion of children in the surgery arm (70.2%) after single procedure compared to the BNT arm (37%). Of 20 children who achieved CR in the BNT arm, 11 (55%) achieved it with one injection, 5 (25%) after the second injection and 4 (20%) after the third injection.
Univariate analysis of subgroups stratified by age showed that the proportion of patients that achieved CR was not significantly different between the two arms for children ≤24 months, whereas it was significantly better in the surgery arm in children >24 months (OR 11.81, 95% CI: 3.05–45.81, p = 0.002). When comparing subgroups stratified by degree of baseline esotropia, there was no significant difference between the two arms for children with esotropia ≤60 PD, but significantly better in the surgery arm in children with esotropia >60 PD (OR = 8.5, 95% CI: 2.4–30.09, p = 0.0005) (Table 2).
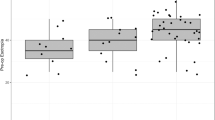
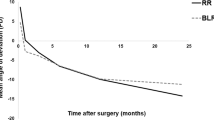
Multivariate logistic regression analysis for the BNT arm showed that age and degree of baseline esotropia were significant independent predictors. Receiver operating characteristic (ROC) curve analysis using univariate predictors, degree of baseline esotropia and age, yielded an area under the curve of 70% and 66%, respectively. The optimal threshold sensitivity/specificity modelled by our data was 50 PD for degree of esotropia (Fig. 2a) and 21 months for age (Fig. 2b).
In the BNT arm, 7 children (13%) had PR and 27 children (50%) had NR. Of the 27 NR children, 21 had subsequent surgery—11 of these achieved CR and 2 PR at 24 weeks post-surgery follow-up. Eight children failed to return for their follow-up visits. Ultimately, CR and PR were achieved in at least 40 (74.1%) of children in the BNT arm within a year of the initial procedure.
Complications in the BNT arm were; partial transient ptosis in 9 children (16.7%), which resolved within 6–8 weeks, transient vertical deviation in 3 children (5.6%) and consecutive exotropia in 13 children (24.1%). Seven of the children with exotropia were associated with CR. There were no cases of globe perforation, infections or chemosis following BNT injections.
In the surgical arm, of the 47 children, 24 had large-angle esotropia and 23 children had very-large-angle esotropia requiring surgery with BNT augmentation. CR was achieved in 17 (70.8%) and 16 (69.6%), respectively, with one procedure. Of the 14 children who failed to achieve CR, 12 had residual esotropia and 2 exotropia. All of the 12 children with esotropia received 3U of BNT as a second procedure and CR was achieved in 8 children while 4 children needed additional surgery.
The two children with exotropia, received BNT to the lateral rectus muscles as initial therapy followed bimedial rectus muscle advancement and had final NR. In total, 45 children (95.7%) had a CR or PR in the surgery arm. There were no major complications of surgery such as slipped or lost muscles, globe perforation or anaesthetic-related issues.
Discussion
In this prospective randomised control study, surgery was superior to BNT in our cohort of children with large-angle esotropia; however, BNT has a definite role as primary treatment option in selected children. Surgery was associated with equally good outcomes irrespective of the age of the child or the degree of esotropia. While previous studies using BNT showed the best outcome in infants [16], our study did not have sufficient numbers to consider the very young separately. Crude analysis of the BNT arm versus the surgery arm, however, did show comparable outcomes to surgery in children ≤24 months of age and with a baseline esotropia ≤60 PD. This association remained valid in the multivariate analysis with non-significant odds ratios between the BNT and surgery arms in patients ≤24 months and ≤60 PD. This is further supported by ROC curve analysis which indicated that children below 21 months of age and those with esotropia below 50 PD are more likely to have complete resolution.
In a systematic review Issaho et al. identified nine papers describing the use of BNT in the management of IE. Most of the studies were non-comparative and success rate varied from 37.5 to 100% [17]. The high-success-rate studies were associated with small to moderate angles of esotropia while studies of large angles reported lower success rates.
The results of this study show a similar trend to that of de Alba Campomannes et al. [11] for large-angle esotropia. In their study, large-angle esotropias of >30 PD treated with BNT were associated with a success rate of 36%. All our study children had angles ≥40 PD with a success rate of 37% but angles ≤60 PD were associated with 50% success. BNT in younger children had a significantly higher success rate (55.2%) than older children (16%). The explanation is probably based on increasing contracture of the medial rectus muscles over time [18]. In our cohort, a better response was seen with one injection and we found lower success rates for second and third injections.
The present study reaffirms the safety of BNT [17] as there were no adverse events associated with BNT injections.
Exotropia after the first injection was a good predictor of success as shown by Campos et al. [16]. In our study 7 of 13 patients with exotropia after the first injection were associated with CR. This represented over a third of all successful cases. In cases where BNT failed to correct the esotropia, alignment with surgery was achieved within a reasonable time interval. On average, it was found that surgery took six to seven times longer than BNT. In resource-constrained settings the short procedure-time for BNT allows many more patients to gain access to treatment at a potentially earlier age.
Our need to recognize cosmetically acceptable small angles (PR) highlights the real problems encountered in developing countries, where functional outcome and potential for fusion may not be a priority. With BNT use, at least 50% of our patients overall achieved CR and PR. Another compelling reason for BNT use is the absence of serious complications and that an exact angle measurement may not be essential. This obviates the need for specialist orthoptic personnel. Orthoptists are few in number and seldom service public sector hospitals in South Africa.
The number of participants achieving a cosmetically acceptable result in the surgical arm was more impressive as only two patients were deemed failures. However, the number of patients that dropped out pre-operatively in this arm may highlight parental reservations concerned with surgery.
The results of this study support the use of BNT in large-angle deviations as augmentation to surgery. Leuder reported a favourable outcome with augmented surgery in 17 out of 23 patients (73%) [19]. Our study showed a similar outcome in patients with augmented surgery. This would eliminate the need for three-muscle surgery and thus allow for shorter theatre-time.
Limitations
The study only followed children for 6 months following the last procedure and late esodrift may still be an issue. The scope of the study addressed only motor response and did not test for fusion in children that were aligned. No attempt was made to establish parental satisfaction or dissatisfaction. We were unable to recruit children younger than 10 months to confirm the reported higher rate of success in this very-young age category [11, 16]. The study also did not compare three-muscle surgery to surgery with augmented BTX which could have added another comparative arm.
Conclusion
Surgery is still the gold standard of managing large-angle IE. However, BNT is a viable primary treatment option for IE. BNT is safe and a short procedure and could be considered as a first-line intervention in developing countries where resources are limited with respect to waiting time for surgery. Further, BNT was found to be more effective in children ≤24 months of age and with baseline angles of ≤60 PD of esotropia.
Summary
What was known before
-
BNT can be used in various types of strabismus.
-
Surgery is the gold standard.
-
In IE, BNT is successful in the management of small angles and very-young patients.
What this study adds
-
BNT can be used in larger angles of deviation <50 PD.
-
Viable option as it takes 5× less time than surgery useful in developing countries with limited resources.
References
Mohney BG. Common forms of childhood strabismus in an incidence cohort. Am J Ophthalmol. 2007;144:465–7.
Kushner BJ, Morton GV. A randomized comparison of surgical procedures for infantile esotropia. Am J Ophthalmol. 1984;98:50–61.
Tolun H, Dikici K, Ozkiris A. Long-term results of bimedial rectus recessions in infantile esotropia. J Pediatr Ophthalmol Strabismus. 1999;36:201–5.
Wan MJ, Chiu H, Shah AS, Hunter DG. Long-term surgical outcomes for large-angle infantile esotropia. Am J Ophthalmol. 2018;189:155–9.
Ing MR. Early surgical alignment for congenital esotropia. J Pediatr Ophthalmol Strabismus. 1983;20:11–8.
Taylor DM. Is congenital esotropia functionally curable? Trans Am Ophthalmol Soc. 1972;70:529–76.
von Noorden GK. A reassessment of infantile esotropia. XLIV Edward Jackson memorial lecture. Am J Ophthalmol. 1988;105:1–10.
Tinley C, Grötte R. Comitant horizontal strabismus in South African black and mixed race children-a clinic-based study. Ophthalmic Epidemiol. 2012;19:89–94.
Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology. 1980;87:1044–9.
McNeer KW, Tucker MG. Comparison of botulinum toxin with surgery as primary treatment for infantile esotropia. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2010;14:558.
de Alba Campomanes AG, Binenbaum G, Campomanes Eguiarte G. Comparison of botulinum toxin with surgery as primary treatment for infantile esotropia. J AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus. 2010;14:111–6.
Pathai S, Cumberland PM, Rahi JS. Prevalence of and early-life influences on childhood strabismus: findings from the Millennium Cohort Study. Arch Pediatr Adolesc Med. 2010;164:250–7.
Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017;3:CD006499.
Benabent EC, García Hermosa P, Arrazola MT, Alió y Sanz JL. Botulinum toxin injection without electromyographic assistance. J Pediatr Ophthalmol Strabismus. 2002;39:231–4.
Von Noorden GK, Isaza A, Parks ME. Surgical treatment of congenital esotropia. Trans Am Acad Ophthalmol Otolaryngol Am Acad Ophthalmol Otolaryngol. 1972;76:1465–78.
Campos EC, Schiavi C, Bellusci C. Critical age of botulinum toxin treatment in essential infantile esotropia. J Pediatr Ophthalmol Strabismus. 2000;37:328–32.
Issaho DC, Carvalho FR, de S, Tabuse MKU, Carrijo-Carvalho LC, de Freitas D. The use of botulinum toxin to treat infantile esotropia: a systematic review with meta-analysis. Invest Ophthalmol Vis Sci. 2017;58:5468–76.
McNeer KW, Tucker MG, Spencer RF. Management of essential infantile esotropia with botulinum toxin A: review and recommendations. J Pediatr Ophthalmol Strabismus. 2000;37:63–7.
Lueder GT, Galli M, Tychsen L, Yildirim C, Pegado V. Long-term results of botulinum toxin-augmented medial rectus recessions for large-angle infantile esotropia. Am J Ophthalmol. 2012;153:560–3.
Acknowledgements
We wish to thank all the patients and parents who were willing to participate in the study, our orthoptist Ms Sarah Young, Ms Adelaide Molopane for coordinating patients visits, the staff of St John assisting with patient care, and the Anglo-American Chairman’s Fund for grant in facilitating additional surgical lists for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mayet, I., Ally, N., Alli, H.D. et al. Botulinum neurotoxin injections in essential infantile esotropia—a comparative study with surgery in large-angle deviations. Eye 35, 3071–3076 (2021). https://doi.org/10.1038/s41433-020-01300-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01300-4
This article is cited by
-
The incidence, clinical features, and management of essential infantile esotropia in the United Kingdom. A British Ophthalmology Surveillance Unit (BOSU) study
Eye (2024)
-
Efficacy of botulinum toxin injection versus bilateral medial rectus recession for comitant esotropia: a meta-analysis
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)