Abstract
Purpose
In the absence of pre-admission testing for colour blindness, many of the currently practicing ophthalmologists are colour blind, accordingly their accuracy of distinguishing fine diabetic retinopathy (DR) changes is still unknown. This study aims to assess the accuracy of diagnosing and staging diabetic retinopathy and macular oedema among protonopic, deutronopic and tritanopic ophthalmologists.
Methods
Cross-sectional assessment of fundus images that were prepared to simulate the appearance in cases of colour blindness. We assessed the accuracy of staging diabetic retinopathy and macular oedema by a retina specialist on colour-blind simulated images. We used randomiser.org to randomly select images to be simulated by the previously validated Vischeck colour blindness simulator.
Results
A total of 150 simulated images were reviewed, 50 images for each of simulated protanopia, deuteranopia and tritanopia. We found that the accuracy for staging DR and macular oedema for protanope grader were 50% and 60%, respectively. Accuracy within one stage difference for DR and macular oedema were 88% and 90%, respectively. For deuteranopes, 56% and 64% accuracy for DR and macular oedema, respectively. Accuracy within one stage difference for DR and macular oedema were 86% and 90%, respectively. For Tritanope, 62% and 84% accuracy for DR and macular oedema, respectively.
Conclusion
Colour vision is important for distinguishing fine details during retina assessment in diabetic retinopathy patients. Colour blindness is associated with low accuracy in staging diabetic retinopathy and macular oedema, particularly among protonopic graders, and to a lesser extent in tritanopic graders.
Similar content being viewed by others
Introduction
It has been reported that the prevalence of colour blindness (CB) among medical practitioners is similar to that of general population, reaching around 8% among males [1, 2]. Previous surveys showed that many of the physicians are unaware about their CB until it is incidentally discovered later during their career [3]. Ophthalmologists and optometrists are among the medical practitioners with high rate of problems related to colour blindness [4]. This observation was based on doctor’s confessions rather than actually testing ophthalmologists. The aim of this study was to assess the accuracy of diagnosing and staging diabetic retinopathy and macular oedema among protonopic (red-blind), deutronopic (green-blind), and tritanopic (blue-blind) ophthalmologists using high-quality fundus imaging, and with the aid of a validated colour-blindness-simulating software. The added value of simulating instead of real-time examining a colour blind ophthalmologist is to eliminate inter-rater variability by asking one retina specialist to read them.
Methods
We recruited high-quality funds images from Indian Diabetic Retinopathy Image Dataset (IDRiD) [5], an open access database for funds images for diabetic retinopathy patients. Retinal fundus images in IDRiD database were acquired from an Eye Clinic located in Nanded, (M.S.), India. Retinal images of humans affected by diabetes were captured with 39 mm distance between lenses and examined eye using non-invasive fundus camera having xenon flash lamp. All the subjects in the dataset had undergone mydriasis using one drop of tropicamide 0.5%. Images were acquired using a Kowa VX-10α digital fundus camera with 50ْ field of view. The images have resolution of 4288 × 2848 pixels and are stored in jpg file format. The size of each image is about 800 KB.
The dataset consists of 516 images done over the period 2009–2017. Experts verified that all images are of adequate quality, clinically relevant, that no image is duplicated and that a reasonable mixture of disease stratification representative of diabetic retinopathy (DR) and diabetic macular oedema is present. The original images stored at the IDRid database were classified by experienced ophthalmologists into separate groups ranging from 0 (No apparent DR) to 4 (Severe DR) according to the International Clinical Diabetic Retinopathy Scale. The risk of macular oedema was based on the presence of exudates [6].
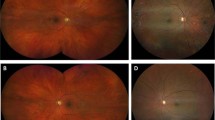
Using randomiser.org, we randomly selected 50 images to be simulated as if were seen by a protanope ophthalmologist, 50 images to be simulated as if were seen by a deuteranope ophthalmologist and 50 images to be simulated as if were seen by a tritanope ophthalmologist. To transform funds images into what a protanope, deuteranope and tritanope ophthalmologist can see, we used Vischeck colour blindness simulator in Fiji software [7], which has been proved to be highly accurate in simulating colour blind images [8]. Figure 1 demonstrates a retinal view as seen by a non-colour blind ophthalmologist (a), and its simulation in case of protanopia (b), deuteranopia (c) and tritanopia (d). The images were reviewed by a single masked certified retina specialist who was asked to grade diabetic retinopathy and the risk of maculopathy on an RGB colour MacBook Pro screen. The nature of the study was explained to the grader and her approval obtained to participate in this study. The grader was blinded for the simulation used for each image. The risk of macular oedema was based on the presence of exudates according to International Clinical Diabetic Retinopathy Scale [6]. We then compared the accuracy of the classification provided by our retina specialist with that of the original images annotated by the IDRiD ophthalmologists.
To assess the reliability of diabetic retinopathy and macular oedema staging by the grader, we repeated the same experiment under the same conditions and using the same sets of simulated images 6 months after the initial assessment. We used SPSS version 21.0 (Chicago, USA), where we performed Spearman correlation to analyse the correlation between initial assessment and the 6 months repeat. We adopted a p value of 0.05 as a significant threshold. To ensure the accuracy of staging diabetic retinopathy and macular oedema by the grader using fundus photographs under the described conditions, we randomly selected another set of 50 images to be used as controls, where no simulation was applied.
Results
A total of 150 simulated images were reviewed, 50 images for each of protanopia, deuteranopia and tritanopia. The median DR stage for the included images was moderate NPDR (stage 2) and for macular oedema was low risk (stage 1).
The accuracy for staging DR and macular oedema for protanope-simulated images were 50% and 60%, respectively, and the accuracy within one stage difference of DR and macular oedema were 88% and 90%, respectively. For deuteranope-simulated images, 56% and 64% accuracy for DR and macular oedema, respectively with an accuracy within one stage difference for DR and macular oedema of 86% and 90%, respectively. For tritanope-simulated images, 62% and 84% accuracy for DR and macular oedema, respectively, with an accuracy within one stage difference for DR and macular oedema of 84% and 90%, respectively. Table 1 details the frequency and percentages for the answers provided by our retina specialist compared to the original key answers for protanopia, deuteranopia and tritanopia images. Two out of four (50%) proliferative diabetic retinopathy in protanope-simulated images were missed and were staged as severe NPDR. Two out of five (40%) proliferative diabetic retinopathy in deuteranope-simulated images were missed, while also three out of six (50%) proliferative diabetic retinopathy of the tritanope-simulated images were missed.
34%, 30%, and 24% of the images were staged less than the actual stages for protanopia, deuteranopia and tritanopia, compared to 18%, 14%, and 14% that were staged greater than the actual stages, respectively.
Regarding test–retest reliability, we found significant association for the protanopia, deuteranopia, and tritanopia simulated images (p < 0.001), with a strong correlation coefficient of 0.765, 0.921, 0.871 for diabetic retinopathy staging, and 0.620, 0.908, 0.803 for macular oedema staging, respectively. The accuracy of the grader for the control images were 90% for both diabetic retinopathy and macular oedema staging, where the falsely graded images where all between stage 2 and 3 for diabetic retinopathy, and between low and high risk for macular oedema.
Discussion
Most medical schools do not require colour vision testing upon admission, neither do admission to ophthalmology programs [4]. This might lead to practicing ophthalmologists that can have colour blindness [9], even without knowing that they have it. We simulated the accuracy of diagnosing and staging diabetic retinopathy and macular oedema in cases of protanopia, deuteranopia, and tritanopia by retina specialist. We found that the overall accuracy for all types of colour blindness is low, with the lowest accuracy is for protanopia and the highest is for tritanopia. The difference between staging the simulated colour blind retina and the correct stage was only one stage difference in almost 90% of cases.
A previous study done on colour blind medical students to assess the accuracy and confidence in diagnosing several signs, the students reported difficulty in the assessment and a low confidence during fundus related signs [1, 10]. One of the main difficulties that may be faced by colour-blind ophthalmologists upon retinal examination is distinguishing artifacts (e.g. melanin pigment) from other retinopathy manifestations as these may have similar appearance [4], which might explain the percentage of images staged higher than the actual stage. Another potential difficulty is distinguishing retinal haemorrhages and other manifestations in patients with chorioretinal degeneration, where the background retina is darker than normal [11]. This is an important barrier during simulated image assessment as confessed by the retina specialist who assessed the simulated images, considering that most patients presenting with diabetic retinopathy are generally old.
We believe that the main limitation of this study is that we only simulated complete colour blindness in terms of protanopia, deuteranopia and tritanopia, which is rarer than partial colour blindness which are termed of protanomaly, deuteranomaly and tritanomaly, respectively. Moreover, grading of maculopathy on fundus photograph has generally poorer pick-up rate compared to retinopathy grading, and generally depend only on assessing the proximity of exudate to fovea. Future studies should focus on simulating other scenarios faced by ophthalmologists in particular, or other medical specialists, as we found a relatively small number of studies in this regard.
Ophthalmology is a specialty that is highly dependent on distinguishing colours, especially upon retinal examination, where subtle details are important. We recommend a colour vision testing upon admission to specialties with high colour demanding (e.g. ophthalmology and pathology), not for discriminating against them during the admission, but for the sake of informing the participant about the limitations they may face. Where this study confirms the importance of colour vision in staging diabetic retinopathy and macular oedema, it also showed that all types of colour blindness are associated with decreased accuracy in staging.
Summary
What was known before
-
Colour blindness is frequent among medical doctors, but they are unaware about it.
-
Ophthalmology is among the medical specialty who reported high problems related to colour blindness.
What this study adds
-
The overall accuracy for all types of colour blindness in staging diabetic retinopathy and macular oedema is low.
-
The accuracy of staging diabetic retinopathy and macular oedema is lowest for protanopia and highest for tritanopia.
Data availability
We also would like to thank the Indian Diabetic Retinopathy research group for providing their database as open access at https://doi.org/10.21227/H25W98 [12].
References
Campbell JL, Spalding AJ, Mir FA, Birch J. Doctors and the assessment of clinical photographs-does colour blindness matter? Br J Gen Pract. 1999;49:459–61.
Balasundaram R, Reddy SC. Prevalence of colour vision deficiency among medical students and health personnel. Malays Fam Physician. 2006;1:52–53.
Anonymous. International Research Group on Colour Vision Deficiencies. In Proc of Symposium—People and organisations—Trove. https://trove.nla.gov.au/people/1263010?c=people. Accessed 29 Oct 2019.
Spalding JAB, Cole BL, Mir FA. Advice for medical students and practitioners with colour vision deficiency: a website resource. Clin Exp Optom. 2010;93:39–41.
Porwal P, Pachade S, Kokare M, Deshmukh G, Son J, Bae W, et al. IDRiD: diabetic retinopathy—segmentation and grading challenge. Med Image Anal. 2020;59:101561.
Wilkinson CP, Ferris FL, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–82.
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, et al. Fiji - an Open Source platform for biological image analysis. Nat Methods. 2012;9:676–82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3855844/. Accessed 29 Oct 2019.
Lillo J, Alvaro L, Moreira H. An experimental method for the assessment of color simulation tools. J Vis. 2014;14:15.
Arden GB, Hall MJ. Does occupational exposure to argon laser radiation decrease colour contrast sensitivity in UK ophthalmologists? Eye. 1995;9:686–96.
Goh SSM, Chan VXB, Tan NC. Colour vision deficiency: is it a handicap? A narrative review of its impact on medical & dental education and practice. Proc Singp Healthcare 2014;23:149–57.
Ouyang Y, Heussen FM, Keane PA, Sadda SR, Walsh AC. The Retinal Disease Screening Study: prospective comparison of nonmydriatic fundus photography and optical coherence tomography for detection of retinal irregularities. Investig Ophthalmol Vis Sci. 2013;54:1460–8.
Porwal P, Pachade S, Kamble R, Kokare M, Deshmukh G, Sahasrabuddhe V, et al. Indian Diabetic Retinopathy Image Dataset (IDRiD). IEEE Dataport. 2018. https://doi.org/10.21227/H25W98. Accessed 25 Oct 2019.
Acknowledgements
The authors would like to thank Dr. Muna Al-Saad, MBBS, Certificate of Higher Specialisation in Ophthalmology, CJB Ophthalmology, FRCS(Ophth) Glasgow, for staging diabetic retinopathy and macular oedema in simulated colour-blind fundus images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript has not been published and is not under consideration for publication elsewhere.
Rights and permissions
About this article
Cite this article
AlRyalat, S.A., Muhtaseb, R. & Alshammari, T. Simulating a colour-blind ophthalmologist for diagnosing and staging diabetic retinopathy. Eye 35, 2229–2232 (2021). https://doi.org/10.1038/s41433-020-01232-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01232-z