Abstract
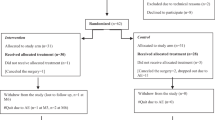
Endobarrier® is a minimally invasive, reversible endoscopic treatment for obesity. It provokes malabsorption along 60 cm of the small intestine, which can contribute to the development of vitamin deficiencies and to changes in bone mineral density (BMD). To determine the prevalence of nutrient deficiencies, changes in body composition and BMD during the first year after Endobarrier® placement. Twenty-one patients with type 2 diabetes met inclusion criteria. Levels of vitamins, micro and macronutrients were assessed prior and at 1, 3 and 12 months post-operatively. DEXA was performed before and 12 months after implant. Nineteen patients completed the 12 months follow-up. Vitamin D deficiency was the most prevalent finding before Endobarrier® implant. The percentage of patients with severe deficiency decreased from 19 to 5% at 12 months after supplementation. Microcytic anaemia was initially present in 9.5% of patients and increased to 26.3% at 12 months. Low ferritin and vitamin B12 levels were observed in 14.2 and 4.8% of patients before the implant and worsened to 42 and 10.5%. Low concentrations of magnesium and phosphorus were also common but improved along the study. A significant but not clinically relevant decrease in BMD of 4.14 ± 4.0% at the femoral neck was observed at 12 months without changes in osteocalcin levels. Vitamin deficiencies are common after Endobarrier® implant. It is therefore important to screen patients prior to and at regular intervals after the implant, and to encourage adherence to diet counselling and supplementation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Schouten R, Rijs CS, Bouvy ND, Hameeteman W, Koek GH, Janssen IM, et al. A multicenter, randomized efficacy study of the EndoBarrier Gastrointestinal Liner for presurgical weight loss prior to bariatric surgery. Ann Surg. 2010;251:236–43.
Vilarrasa N, de Gordejuela AG, Casajoana A, Duran X, Toro S, Espinet E, et al. Endobarrier® in grade i obese patients with long-standing type 2 diabetes: role of gastrointestinal hormones in glucose metabolism. Obes Surg. 2017;27:569–77.
Rohde U, Hedbäck N, Gluud LL, Vilsbøll T, Knop FK. Effect of the EndoBarrier Gastrointestinal Liner on obesity and type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2016;18:300–5.
American Diabetes Association. Standards of medical care in diabetes 2017. Diabetes Care. 2017;40:S57–63.
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon MM, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21:S1–27.
McColl KE. Effect of proton pump inhibitors on vitamins and iron. Am J Gastroenterol. 2009;104:S5–9.
Earthman CP, Beckman LM, Masodkar K, Sibley SD. The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. Int J Obes. 2012;36:387–96.
Kurstjens S, de Baaij JH, Bouras H, Bindels RJ, Tack CJ, Hoenderop JG. Determinants of hypomagnesemia in patients with type 2 diabetes mellitus. Eur J Endocrinol. 2017;176:11–9.
Haglin L, Lindblad Å, Bygren LO, Hypophosphataemia in the metabolic syndrome. Gender differences in body weight and blood glucose. Eur J Clin Nutr. 2001;55:493
Kim HJ, Koo HS, Kim YS, Kim MJ, Kim KM, Joo NS, et al. The association of testosterone, sex hormone-binding globulin, and insulin-like growth factor-1 with bone parameters in Korean men aged 50 years or older. J Bone Miner Metab. 2016;1:1–7.
Acknowledgements
The authors thank Dr. Kenneth McCreath for helpful discussions on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. Nuria Vilarrasa is the recipient of grants “Ajuts per a projectes de recerca clínica de l’Hospital Universitari de Bellvitge (2011-PR143/11)” and of project “PI11/01960 and PI14/01997” funded by Instituto de Salud Carlos III and co-funded by European Union (ERDF, “A way to build Europe”).
Rights and permissions
About this article
Cite this article
Vilarrasa, N., Fabregat, A., Toro, S. et al. Nutritional deficiencies and bone metabolism after endobarrier in obese type 2 patients with diabetes. Eur J Clin Nutr 72, 1447–1450 (2018). https://doi.org/10.1038/s41430-017-0074-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-017-0074-x