Abstract
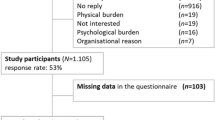
Sexual dysfunction after allogeneic hematopoietic cell transplantation (allo-HCT) is a common long-term complication. We conducted a European multicenter cross-sectional study of adult allo-HCT recipients who had survived >2 years and their partners to investigate sexual functioning after HCT and to evaluate whether discussion about sexual functioning between the transplant team and the survivor and partner was perceived to have taken place. In total, 136 survivors (77 males, 59 females) and 81 partners (34 males, 47 females) participated. Median age was 56 and 54 years in male and female survivors, respectively. Forty-seven percent of male and 65% of female survivors and 57% of male and 59% of female partners reported clinically relevant sexual problems. Sixty-two percent of survivors and 79% of partners reported that sexual functioning had not been discussed with them during transplant. Standardized sexual functioning scores were correlated with self-reported health status in survivors (rho = 0.24, p = 0.009). The high prevalence of sexual dysfunction warrants additional studies focusing on the impact of changes in sexuality for patients as well as their partners. Future studies should also investigate which methods that are effective in preventing or treating sexual problems after allo-HCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data are available upon request from the corresponding author.
References
Majhail NS, Tao L, Bredeson C, Davies S, Dehn J, Gajewski JL, et al. Prevalence of hematopoietic cell transplant survivors in the United States. Biol Blood Marrow Transpl. 2013;19:1498–501.
Burns LJ, Abbetti B, Arnold SD, Bender J, Doughtie S, El-Jawahiri A, et al. Engaging patients in setting a patient-centered outcomes research agenda in hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2018;24:1111–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
Noerskov KH, Schjødt I, Syrjala KL, Jarden M. Sexual function 1-year after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transpl. 2016;51:833–40.
Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111:989–96.
Syrjala KL, Langer SL, Abrams JR, Storer BE, Martin PJ. Late effects of hematopoietic cell transplantation among 10-year adult survivors compared with case-matched controls. J Clin Oncol. 2005;23:6596–606.
Syrjala KL, Roth-Roemer SL, Abrams JR, Scanlan JM, Chapko MK, Visser S, et al. Prevalence and predictors of sexual dysfunction in long-term survivors of marrow transplantation. J Clin Oncol. 1998;16:3148–57.
Syrjala KL, Schoemans H, Yi JC, Langer SL, Mukherjee A, Onstad L, et al. Sexual functioning in long-term survivors of hematopoietic cell transplantation. Transpl Cell Ther. 2021;27:80.e1–80.e12.
Humphreys CT, Tallman B, Altmaier EM, Barnette V. Sexual functioning in patients undergoing bone marrow transplantation: a longitudinal study. Bone Marrow Transpl. 2007;39:491–6.
Wong FL, Francisco L, Togawa K, Kim H, Bosworth A, Atencio L, et al. Longitudinal trajectory of sexual functioning after hematopoietic cell transplantation: impact of chronic graft-versus-host disease and total body irradiation. Blood. 2013;122:3973–81.
Booker R, Walker L, Raffin, Bouchal S. Sexuality after hematopoietic stem cell transplantation: a mixed methods study. Eur J Oncol Nurs. 2019;39:10–20.
Claessens JJ, Beerendonk CC, Schattenberg AV. Quality of life, reproduction and sexuality after stem cell transplantation with partially T-cell-depleted grafts and after conditioning with a regimen including total body irradiation. Bone Marrow Transpl. 2006;37:831–6.
Dyer G, Gilroy N, Bradford J, Brice L, Kabir M, Greenwood M, et al. A survey of fertility and sexual health following allogeneic haematopoietic stem cell transplantation in New South Wales, Australia. Br J Haematol. 2016;172:592–601.
Haavisto A, Mathiesen S, Suominen A, Lähteenmäki P, Sørensen K, Ifversen M, et al. Male sexual function after allogeneic hematopoietic stem cell transplantation in childhood: a multicenter study. Cancers. 2020;12:1786.
Tierney DK, Palesh O, Johnston L. Sexuality, menopausal symptoms, and quality of life in premenopausal women in the first year following hematopoietic cell transplantation. Oncol Nurs Forum. 2015;42:488–97.
Yoo KH, Kang D, Kim IR, Choi EK, Kim JS, Yoon SS, et al. Satisfaction with sexual activity and sexual dysfunction in hematopoietic stem cell transplantation survivors and their partners: a couple study. Bone Marrow Transpl. 2018;53:967–76.
Nørskov KH, Schmidt M, Jarden M. Patients’ experience of sexuality 1-year after allogeneic haematopoietic stem cell transplantation. Eur J Oncol Nurs. 2015;19:419–26.
Zavattaro M, Felicetti F, Faraci D, Scaldaferri M, Dellacasa C, Busca A, et al. Impact of allogeneic stem cell transplantation on testicular and sexual function. Transpl Cell Ther. 2021;27:182.e1–e8.
Forgeard N, Jestin M, Vexiau D, Chevillon F, Ricadat E, Peffault de Latour R, et al. Sexuality- and fertility-related issues in women after allogeneic hematopoietic stem cell transplantation. Transpl Cell Ther. 2021;27:432.e1–e6.
Wingard JR, Curbow B, Baker F, Zabora J, Piantadosi S. Sexual satisfaction in survivors of bone marrow transplantation. Bone Marrow Transpl. 1992;9:185–90.
Molassiotis A, van den Akker OB, Milligan DW, Boughton BJ. Gonadal function and psychosexual adjustment in male long-term survivors of bone marrow transplantation. Bone Marrow Transpl. 1995;16:253–9.
Marks DI, Friedman SH, Delli Carpini L, Nezu CM, Nezu AM. A prospective study of the effects of high-dose chemotherapy and bone marrow transplantation on sexual function in the first year after transplant. Bone Marrow Transpl. 1997;19:819–22.
El-Jawahri A, Fishman SR, Vanderklish J, Dizon DS, Pensak N, Traeger L, et al. Pilot study of a multimodal intervention to enhance sexual function in survivors of hematopoietic stem cell transplantation. Cancer. 2018;124:2438–46.
Majhail NS. Long-term complications after hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2017;10:220–7.
Tierney DK. Sexuality following hematopoietic cell transplantation. Clin J Oncol Nurs. 2004;8:43–47.
Lupinacci L, Lamore K, Seyeux AL, Untas A. Facilitators and obstacles to couples’ intimacy after hematopoietic stem cell transplantation: a qualitative study. J Psychosoc Oncol. 2021. https://doi.org/10.1080/07347332.2021.2004292.
Kim IR, Jang SY, Shin HS, Choi HJ, Jung CW, Yoon SS, et al. Association between sexuality knowledge and sexual dysfunction in hematopoietic stem cell transplantation patients and their partners. Patient Educ Couns. 2020;103:1630–6.
Park ER, Norris RL, Bober SL. Sexual health communication during cancer care: barriers and recommendations. Cancer J. 2009;15:74–7.
Eeltink CM, Witte BI, Stringer J, Liptrott S, Babic A, Greenfield DM, et al. Health-care professionals’ perspective on discussing sexual issues in adult patients after haematopoietic cell transplantation. Bone Marrow Transpl. 2018;53:235–45.
Kornblith AB, Anderson J, Cella DF, Tross S, Zuckerman E, Cherin E, et al. Hodgkin disease survivors at increased risk for problems in psychosocial adaptation. Cancer Leuk Group B Cancer. 1992;70:2214–24.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208.
ter Kuile MM, Brauer M, Laan E. The Female Sexual Function Index (FSFI) and the Female Sexual Distress Scale (FSDS): psychometric properties within a Dutch population. J Sex Marital Ther. 2006;32:289–304.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Acknowledgements
The authors would like to thank Frank Wissing, partner of Andrea Linke, for valuable input to the interpretation and description of the results; the EBMT Patient Advocacy Committee and the EBMT Patient Engagement Taskforce for their collaboration; and the EBMT Nurses Group, the EBMT Transplant Complications Working Party and the EBMT Trainee Committee for their support of the study. This study was funded by the EBMT Nurses Group.
Author information
Authors and Affiliations
Contributions
CE was responsible for designing and setting up the study, collecting and interpreting data, and writing the manuscript. LKG was responsible for interpreting data and writing the first draft of the manuscript. JMo was responsible for analyzing and interpreting data and writing the manuscript. PB was responsible for collecting and linking data. DMG, JS and SL were responsible for designing and setting up the study and reviewing the manuscript. MK, PT, SB, DD, SS, LW and AK were responsible for collecting and interpreting data and reviewing the manuscript. ZP, HS and JMu were responsible for supervising the study, interpreting data and writing the manuscript.
Corresponding author
Ethics declarations
Competing interests
AL reports having received personal fees from Novartis and Bristol-Myers Squibb. HS reports having received personal fees from Incyte, Janssen, Novartis, Jazz Pharmaceuticals, Takeda, and from the Belgian Hematological Society (BHS), as well as research grants from Novartis and the BH, paid to her institution. She has also received non-financial support from Incyte, Novartis, Gilead, the EBMT (European Society for Blood and Marrow Transplantation), and the CIBMTR (Center for International Bone Marrow Transplantation Research). JMu reports honorarium from Therakos, Jazz Pharmaceuticals, Janssen and Gilead/Kite. None of these potential conflicts of interest are relevant to this project. The rest of the authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gjærde, L.K., Eeltink, C., Stringer, J. et al. Sexual function of adult long-term survivors and their partners after allogeneic hematopoietic cell transplantation in Europe (S-FAST): a study from the Transplant Complications Working Party and Nurses Group of the EBMT. Bone Marrow Transplant 58, 195–202 (2023). https://doi.org/10.1038/s41409-022-01869-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01869-2