Abstract
Infections are frequently experienced complications for patients undergoing haematopoietic cell transplant (HCT). To assess current infection prevention strategies, an international survey among HCT nurses was conducted by the Nurses Group and IDWP of the EBMT. Nurse representatives from all EBMT transplant centres were invited to complete an online questionnaire on protective environment in adult and paediatric HCT units. A total of 141 complete questionnaires were returned for the isolation section and 26 for the paediatric section, the majority of respondents (89.4%) being nurses. A small number of centres (7.1%) reported not allowing visitors, the rest have rules for entering patient rooms. Most HCT units (99.3%) indicated that nurses play a critical role in infection prevention and measures differed between bacterial infections and viral infections. Many of the paediatric units (57.7%) had a play area, applying rules of entry. To our knowledge, this is the first survey on protective environment directed at nurses within HCT centres. Despite having different practices, most HCT units tend to decrease isolation procedures and the use of PPE for multi-drug resistant organisms. This must concur with an increase of hand hygiene compliance, for which our data show that there is still room for improvement.
Similar content being viewed by others
Introduction
One of the most frequently experienced complication for patients undergoing haematopoietic cell transplant (HCT) are infections [1,2,3]. General guidelines for preventing healthcare-associated infections published by Centres for Disease Control and Prevention are valid for all HCTs, with the most important related to hand hygiene [4,5,6]. A systematic review and meta-analysis by Schlesinger et al. summarised that infection control interventions, including protective isolation, hand hygiene, low bacterial or sterile diet, barrier isolation (use of gloves, gown and mask) and prophylactic antibiotics, were all associated with a significant decrease of all-cause mortality [7].
Specific international HCT recommendations relating to isolation procedures and infection control issues were published in 2009 [1, 8]. To date, there is no universal standard of practice for infection prevention within the field of HCT and the measures taken to reduce risk are diverse [9]. As nurses are real-life hosts of a transplant ward, their role in ensuring a protective environment is crucial. Through this international survey, the Nurses Group and Infectious Diseases Working Party (IDWP) of the EBMT aim to provide an overview of the infection prevention strategies used among member centres in different countries.
Methods
Study design, sample and setting
In April 2019, 638 principal nurses of European Society for Blood and Marrow Transplantation (EBMT) transplant centres were invited to complete an online SurveyMonkey by July 2019. Three reminders were sent out from EBMT Leiden Data Office, one every three weeks and some centres were contacted per email personally by the study coordinator in order to achieve complete submissions.
The survey
The objective of this survey is to assess current infection prevention strategies in EBMT centres. The content of the survey was devised by an expert panel of nurses and expert physicians of the IDWP. The survey, available only in English, consisted of 87 questions, which were divided into five main sections for a total of 87 questions (Supplementary File 1): (1) general information about the HCT centre, (2) isolation practices, (3) outpatients settings, (4) cleaning procedures, (5) protective measures specific to paediatric units. In the current manuscript, only data relating to modules 1, 2 and 5 have been reported. The choice to include these three sections has been taken on size and similarity of the data. Content relating to management of outpatients and cleaning procedures will be analysed separately.
Definitions
Five moments of hand hygiene as defined by the World Health Organization: moment (1) before touching a patient, moment (2) before doing a clean/aseptic procedure, moment (3) after having had body fluid exposure risk, moment (4) after touching a patient, and moment (5) after touching the patient surroundings [5].
High efficiency particulate air (HEPA) filter: a system of mechanical air filtration that retains small particles whose diameter is ≧ to 0.3 micrometre.
Multidrug-resistant (MDR) bacteria included methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), extended spectrum beta lactamase (ESBL) and carbapenem-resistant Enterobacteriaceae (CRE) [10].
Apron: plastic disposable piece of protective equipment worn to protect healthcare uniforms when there is a moderate risk of contamination by blood, body fluids, excretions or secretions.
Gown: full length body fluid-repellent gown, to be worn when the risk of splashing of body fluids or when the risk of the uniform’s contamination is extensive.
Contact precautions: measures undertaken in addition to transmission-based precautions; key elements are single room, hand hygiene, personal protective equipment (PPE) as disposable aprons and gloves, dedicated equipment (personal stethoscope, blood pressure cuff, oximeter, thermometer, torch, weighing scale), information to visitors, cohorting of patients if single room is not available and cohorting of staff.
Enhanced contact precautions: the use of gown is recommended in addition to other measures of contact precautions.
Droplet precautions: measures undertaken to prevent the spread of pathogens through respiratory or mucous membrane contact. Recommended PPE are surgical masks or respirators, single room, dedicated equipment, spatial separation of more than one metre [11].
Statistical analysis
Data were analysed using frequency tables of the multiple-choice questions, and listings of the open-ended questions. The frequency of each multiple-choice answer is presented as a proportion of all non-missing answers. All analyses were done using the open source statistical software R, version 3.6.2.
Results
Characteristics of respondents
Of the 638 centres contacted, 141 complete questionnaires were returned for the isolation section and 26 for the paediatric section, leading to a response rate of 22.1%. These 141 centres were located in 30 countries (median number of responding centres per country: Europe (n = 23), Africa (n = 2), Canada (n = 1), Asia (n = 4)). Characteristics of respondents are presented in Table 1, each single HCT centre is defined as respondent.
Visitors policy
With respect to age of allowed visitors, 35% of centres do not apply a limit; 7.1% of centres do not allow any visitors, and in 51.9% of HCT units age limits are used. In 25% of centres visitors only above 12 years of age are allowed, in 7.9% the age limit is 14 years and in 9.3% of HCT units it is of 18 years. Other requirements are specific for single units, as for one paediatric centre, the parents are asked to provide a list of six persons who are allowed to visit the patient. The majority of centres (89%) forbid entry of visitors with signs or symptoms of infections and some centres have vaccination requirements for visitors (Table 2).
In 44% of centres, visitors have to change into hospital clothes before entering the patient’s room and wear PPE. The most frequently used PPE was a facemask, followed by gowns, gloves and aprons (Table 2).
Room’s air filtration and ventilation
HEPA filtration are employed at 91.3% and positive air pressure relative to the corridor are present in 85.2% of the centres. Twelve air changes/hour are in place in 73.2% of HCT units and directed room airflow in 54.2%. A rate of 79.1% of centres stated that they do not have regular rooms without any air filtration. According to Centers for Disease Control and Prevention (CDC) the air quality for HCT units is improved by a combination of controls, which include also prohibiting dried and fresh flowers to enter the room: this is in place in 96.3% of centres and having strategies to minimise dust is observed by 92.6% of HCT units.
Nurses practices
Respondents indicated that the education on infection control measures of visitors is important, where nursing staff play a significant role in education provision (in 99.3% of centres this education is performed by nurses vs. doctors in 0.7% centres) providing face-to-face instructions (97.1% face-to-face meeting vs. 2.9% brochure/leaflets/poster).
In preparation for a shift on the HCT unit involving direct patient care, we asked if nurses remove jewellery as an infection control practice. The majority replied that rings (93.5%), followed by watches (86%) and bandages/dressings/plasters (80.1%), wedding ring (66.4%) and earrings (25.8%) are removed. In almost half of the centres (43.7%), nurses take off all jewellery.
Almost all HCT units state that hand washing with soap and water is standard practice at the beginning (86.1%) and end of the shift (81.8%) and additionally performed when dirty (99·3%), soiled with body fluids (96·4%) or the patient is infected with Clostridium difficile (87.6%). Besides hand washing, the use of alcohol gel was evaluated according to the five moments for hand hygiene promoted by the WHO:[5] moment 1 and moment 4 were most frequently followed, while moment 3 has the lowest percentage of compliance (Fig. 1).
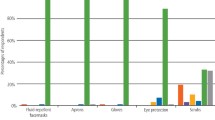
In case patients need to be isolated on contact-, enhanced contact- or droplet isolation, the PPE used for the different types of isolation are gloves, surgical mask and gown (Fig. 2). Further applied PPE are apron, shoe covers, cuff and eye protection. Facial protector type N95 (FFP2) is worn mostly in case of droplet isolation (47.4%), followed by enhanced contact isolation (32.1%) and contact precautions (9.8%).
Personal protective equipment in case of specific bacterial infections
In the majority (90%) of centres, patients infected with MDR bacteria or Clostridium difficile are hospitalised in single room isolation, information to visitors is provided and dedicated equipment is present in the room for each single patient (Fig. 3). Enhanced contact precautions are more common in case of ESBL and carbapenem-resistant Gram-negative organisms (79%), followed by MRSA and VRE (78.8%) and Clostridium difficile toxin positive patients (77.2%).
Personal protective equipment for patients with viral and Pneumocystiis jirovecii diseases
For community respiratory viruses, the majority of respondents indicated single room isolation (91.7%), followed by droplet precautions (83.2%), surgical mask (72.9%), contact precautions (70.0%), N95 facial protector (47.1%) and enhanced contact precautions (45.4%) in HCT units. Measures applied for patients with Norovirus, Adenovirus and Pneumocystiis jirovecii included single room isolation (used in >80.0% of centres for all three organisms), followed by wearing a surgical mask, contact precautions and droplet isolation (Fig. 4).
Paediatric setting
Twenty-six EBMT centres from 12 European countries and one Asian country replied to this part of the survey. The majority of respondents were nurses in various positions (84.5% registered nurse, research nurse, clinical nurse specialist, clinical nurse manager, HCT coordinator and advanced nurse practitioner), followed by quality managers (11.5%) and physicians (3.8%).
Different from the adult setting, some questions dealt with the patient possibility to exit the room and join a play area. In order to join the play area safely, rules were applied as to when paediatric patients can enter the play area: A percentage of 26.9 of centres allow patients only during the conditioning period, the same percentage at any time with a mask, and in 30.8% of centres patients with neutropenia can go in the play area. In isolation rooms, less than half of the centres allow entry of teaching personnel, fur toys, exclusively new toys, and bath toys (Table 3).
Discussion
To our knowledge, this is the first survey on protective environment and isolation practices directed predominantly to nurses who work in HCT. Historically, to minimise the risk of infection during neutropaenia, the goal was to achieve a “germ-free” environment for a “germ-free” patient. Attention was focused on external factors such as sterile food and gowns for all healthcare personnel who had contact with the patient. The “germ-free” patient was not realistic; working in an isolator (plastic tent with sleeves) was difficult for staff and unpleasant for the patient. Fenelon proposed that endogenous sources of infection (e.g. the gastrointestinal tract) were considered a more significant source of pathogens than exogenous ones. These findings ushered in a “post-isolation” period, when the use of protective isolation and gowns was limited and restrictions on visitors relaxed unless they were ill and could be a source of infection [12]. Allowing visitors to the HCT unit is fundamental [13] for the patient’s psychological wellbeing, helping to avoid feelings of loneliness, and experience a sense of being cut out from the external world during prolonged hospitalisations accompanying transplantation [14]. On the other hand, visitors can contribute to organism transmission which can be minimised by forbidding visits to sick patients, vaccination practices and following certain precautions. Our results suggest only a small number of units do not allow any visitors. The majority, however, applies a visitor’s policy. The Society for Healthcare Epidemiology of America (SHEA) guidelines [15] recommend that visitors of immunocompromised patients wear gloves, gown, surgical masks or N95 facial protector. Our survey demonstrates that nearly half of HCT centres require visitors to change into different clothes before entering the hospital room and wear protective equipment. SHEA guidelines point out on the importance of visitors’ education on hand hygiene and different types of precautions provided by nurses. We demonstrate that nurses play a critical role in the education of visitors, family members and patients. Although a bias is possible, as mainly nurses responded to the survey, still in the nurse’s opinion, delivering continuous face-to-face education should be their task.
Stoll et al. undertook a study in which an intervention group of neutropaenic patients were nursed on a ward where rooms were equipped with protective environment; the control group were admitted to any other ward. The authors observed a decrease in fungal infections within the interventional group. These results were explained as being due to a high adherence to hand hygiene and better air filtration systems (including HEPA filters, positive air pressure and rooms with good sealing) in the protective environment ward [16]. Based on our survey results, although the respondents knew exactly the minimal air changes per hour in their unit, from a nursing point of view, rules on prohibiting the entrance of dried and fresh flowers and strategies to minimise the dust are more rooted than paying attention to the characteristics of air filtration systems. HEPA filtration and positive air pressure showed a presence of 91.3% and 85.2%, respectively. Compared to a previous survey performed by the IDWP among EBMT centres in 2012, respondents stated that 99.4% of the rooms were equipped with HEPA filters [17]. Although both studies did not have the same respondents, this difference can imply that nurses concentrate on practical issues rather than the structural facilities and types of ventilation at their unit.
Hand hygiene is the most important measure to prevent infections in HCT patients. Mank et al. demonstrated no increase in infection rate or mortality following the change of strategy, when strict protective isolation was abandoned but intensive campaign on hand hygiene was performed [18].
Our results suggest that HCT nurses perform hand hygiene more often after leaving the healthcare zone (moments 4 and 5 in 93.5%) compared to patient zone (moments 1, 2, 3 in 90.6%). This is different from the literature, where moment three is generally the most adhered to in practice in critical patients [19]. Additionally, our survey responses imply higher rates of hand hygiene as compared to another study carried out in high-risk settings as an intensive care unit [20]. The compliance rate reported by direct observation is lower for hand hygiene [21]. This difference might be explained by the chosen mode of questionnaire administration (self-administration), however, direct observation can lead to overestimation due to the Hawthorne effect [22].
According to WHO guidelines on hand hygiene published in 2009 [5], the consensus recommendation is to strongly discourage the wearing of rings or other jewellery during health care. If religious or cultural influences strongly condition the healthcare-worker’s attitude, the wearing of a simple wedding ring (band) during routine care may be acceptable, but in high-risk settings, all rings or other jewellery should be removed [5]. In compliance to this consensus recommendation, HCT units are considered high-risk settings; therefore, it would be advisable to remove wedding rings. In our survey, however, in less than half centres, nurses take off all jewellery; specifically wedding ring and earrings are removed in 66.4% and 25.8% of centres, respectively. Education is needed to improve the compliance with these recommendations for healthcare-workers working in HCT.
Finally, nurses have an essential role in protecting patients from specific contagious pathogens by the correct application of isolation types and surveillance of application by others. Wearing the appropriate PPE is imperative to minimise spread of these organisms. The heterogeneity of wards in the number of centres is huge and the recommendations in literature is various, particularly on specific single bacteria in non-critical wards [23, 24]. Our results indicate that measures including contact precautions, enhanced contact precautions, single room isolation, dedicated equipment and information for visitors were most often applied in caring for patients with resistant bacterial infections, with rates which vary from 70 to 97%. Single room isolation, droplet isolation together with contact isolation, and the usage of surgical mask are most often applied in caring for patients with viral or fungal infections (45–91%). Our data point out that although the usage of surgical masks is implied in the type of droplet isolation for respiratory viruses, the rates of the application of contact precautions for this type of isolation is related to the use of surgical masks and equal, a lower percentage of enhanced contact precautions is similar to that of facial protector. We did not find any specific literature that indicates which kind of PPE is recommended for HCT patients, but from our findings, with regards to respiratory viruses, there are two main attitudes: contact precautions with surgical mask and enhanced contact precautions with facial protector N95 (FFP2). Previous study did not demonstrate any difference in the rate of laboratory-confirmed influenza in healthcare personnel working in outpatient setting when surgical masks versus N95 facial protector were used [25].
Current guidelines [1] recommend that in paediatric settings, play areas are allowed to be attended by patients undergoing conditioning regimen, when at least daily cleaning and disinfection can be provided. More than half of the paediatric HCT units in our survey had a play area, and different rules were applied to join it safely, among them wearing masks in certain settings. Regarding toys, books and other playthings (washed and cleaned before entry), compliance with the current guidelines was reported in only 70% of centres and merits attention.
Unfortunately, it was not possible to compare data from type of HCT performed (autologous and allogeneic) since centres performing only autologous transplants were 7.8% of the total and the rest of the centres undertake both. The small number of respondent paediatric centres (n = 26) over the adult centres (n = 115) prohibited comparison. Another limitation was the inability to geographically compare centres, since the vast majority of responding centres were from South and Western Europe. The survey was addressed to nurses, but 10.6% were physicians; the authors acknowledge this as a further limitation as no subgroup analysis has been undertaken and the answers were not excluded. The survey was conducted in 2019 from April to July, in a time in which COVID-19 pandemic was unforeseen.
Infections and nurses have a common denominator, they are there for the patient 24 h a day, seven days a week and both are fighting to win. Nurses are hosts of transplant wards and are mostly responsible for creating safe conditions and protective environment for patients. The educational role starts from admission of the patient, involves also caregivers, family and visitors and continues until discharge. The main areas of education are on the correct way of wearing PPE and showing good knowledge of which type of personal protective equipment is the safest for the patient and for healthcare personnel. Despite HCT centres having different practices, hand hygiene is extremely important and our data show that there is still room for improvement, for example setting rules on wearing wedding rings. In most centres there is the tendency to decrease the use of PPE in isolation procedures for multi-drug resistant organisms, but this must go hand in hand with an increase of hand hygiene compliance.
HCT patients are a vulnerable category, if nurses adopt poor infection control procedures or are not compliant to the common practices, they contribute to transmission of contagious pathogens to the patients. More attention to appropriate protective environment choosing the right equipment could achieve less possibility for infections for patients.
In conclusion, our results provide an overview of the main common practices among nurses in HCT centres. In order to create recommendations, further research in different and specific areas as stopping infected people visiting HCT patients, more compliance on hand hygiene and wearing of jewellery, allowance to the play area for paediatric HCT patients is needed.
References
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transpl. 2009;15:1143–38.
Girmenia C, Bertania A, Picciocchi A, Perruccio K, Algarotti A, Busca A, et al. Incidence, risk factors and outcome of pre-engraftment gram-negative bacteremia after allogeneic and autologous hematopoietic stem cell transplantation: an Italian prospective multicenter survey. Clin Infect Dis. 2017;65:1884–96.
Mikulska M, Raiola AM, Galaverna F, Balletto E, Borghesi ML, Varaldo R, et al. Pre-engraftment bloodstream infections after allogeneic hematopoietic cell transplantation: impact of T Cell-Replete transplantation from a haploidentical donor. Biol Blood Marrow Transpl. 2018;24:109–18.
Centers for Disease Control and Prevention. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep.. 2002;51:1–48.
WHO. WHO guidelines on hand hygiene in health care. 2009. https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf. Accessed 9 March 2020.
Centers for Disease Control and Prevention, Infectious Disease Society of America & American Society of Blood and Marrow Transplant. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. MMWR Recomnm Rep.2000;49:1–125.
Schlesinger A, Mical P, Gafter-Gvili A, Rubinovitch B, Leibovici L. Infection-control interventions for cancer patients after chemotherapy: a systematic review and meta-analysis. Lancet Infect Dis. 2009;9:97–107.
Yokoe D, Casper C, Dubberke E, Leee G, Muñoz P, Palmore T, et al. Infection prevention and control in health-care facilities in which heamatopoietic cell transplant recipients are treated. Bone Marrow Transpl. 2009;44:495–507.
Rump B, Timen A, Verweij M, Hulscher M. Experiences of carriers of multidrug-resistant organisms: a systematic review. Clin Microbiol Infect. 2019;25:274–79.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
CDC, 2019. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html. Accessed 25 March 2020.
Fenelon LE. Protective isolation: who needs it? J Hosp Infect. 1995;30:218–22.
Biagioli V, Piredda M, Mauroni MR, Alvaro R, De, Marinis MG. The lived experience of patients in protective isolation during their hospital stay for allogeneic haematopoietic stem cell transplantation. Eur J Oncol Nurs. 2016;24:79–86.
Biagioli V, Piredda M, Alvaro R, De Marinis MG. The experiences of protective isolation in patients undergoing bone marrow or hematopoietic stem cell transplantation: systematic review and metasynthesis. Eur J Cancer Care. 2017;26: https://doi.org/10.1111/ecc.12461.
Munoz-Price LS, Banach DB, Bearman G, Gould JM, Leekha S, Morgan DJ, et al. Isolation precautions for visitors. Infect Control Hosp Epidemiol. 2015;36:747–58.
Stoll P, Silla LM, Cola CM, Splitt BI, Moreira LB. Effectiveness of a Protective Environment implementation for cancer patients with chemotherapy-induced neutropaenia on fever and mortality incidence. Am J Infect Control. 2013;41:357–59.
Styczynski J, Tridello G, Donnlly JP, Iacobelli S, Hoek J, Mikulska M, et al. Protective environment for hematopoietic cell transplant (HSCT) reecipients: The Infectious Diseases Working Party EBMT analysis of global recommendations on health-care facilities. Bone Marrow Transpl. 2018;53:1131–38.
Mank A, van der Lelie H. Is there still an indication for nursing patients with prolonged neutropenia in protective isolation? An evidence-based nursing and medical study of 4 years experience for nursing patients with neutropenia without isolation. Eur J Oncol Nurs. 2003;7:17–23.
Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws ML, Moro ML, et al. Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis. 2013;13:843–51.
Anwar MM, Elareed HR. Improvement of hand hygiene compliance among health care workers in intensive care units. J Prev Med Hyg. 2019;60:E31–E35.
Oliveira AC, Gama CS, Paula AO. Multimodal strategy to improve the adherence to hand hygiene and self-assessment of the institution for the promotion and practice of hand hygiene. J Public Health. 2018;40:163–68.
Bruchez SA, Duarte GC, Sadowski RA, da Silva Filho AC, Fahning WE, Belini Nishiyama SA, et al. Assessing the Hawthorne effect on hand hygiene compliance in an intensive care unit. Infect. Prev Pract. 2020:2. https://doi.org/10.1016/j.infpip.2020.100049.
Maechler F, Schwab F, Hansen S, Fankhauser C, Harbarth S, Huttner B, et al. Contact isolation versus standard precautions to decrease acquisition of extended-spectrum ß-lactamase-producing Enterobacterales in non-critical wards: a cluster-randomised crossover trial. Lancet Infect Dis. 2020;20:575–84.
Ford CD, Lopansri BK, Gazdik MA, Webb B, Snow GL, Hoda D, et al. Room contamination, patient colonization pressure, and the risk of vancomycin-resistant Enterococcus colonization on a unit dedicated to the treatment of hematologic malignancies and hematopoietic stem cell transplantation. Am J Infect Control. 2016;44:1110–15.
Radanovich LJ Jr, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, Gaydos CA, et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. JAMA. 2019;322:824–33.
Acknowledgements
We are extremely grateful to all nurses and other colleagues of EBMT centres who filled out the survey. Thanks for the time.
Author information
Authors and Affiliations
Consortia
Contributions
IA, TNB, MC, ECG, JacS, DA, MM, LG, JS, SJL, PVB conceptualised and designed the study. AEK collected the survey responses and KB performed the data analysis. IA, JS, DA, DH, JacS interpreted the results. IA has been the primary person responsible for writing the manuscript. IA, JS, AEK, KB, DA, JacS, DH, MM, TNB, MC, ECG, PVB, LG, SJL, JM, were involved in drafting the work or revising it critically for important intellectual content. All authors approved the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Agreiter, I., Kozijn, A.E., Bakunina, K. et al. Contribution of nurses to protective environment in haematopoietic cell transplant setting: an international survey by the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant 56, 1433–1440 (2021). https://doi.org/10.1038/s41409-020-01194-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01194-6
This article is cited by
-
Infection prevention practices among EBMT hematopoietic cell transplant centers: the EBMT Infectious Disease Working Party survey
Bone Marrow Transplantation (2023)