Abstract
Study design
A narrative review describing various components of sexual dysfunction in men with spinal cord injury (SCI), as well as addressing potential therapeutic approaches.
Objectives
Restoration of sexual function is considered one of the most important health priorities for individuals with SCI. The purpose of this review is to provide information regarding the factors that are less appreciated when considering changes to sexual function in men with SCI. We also propose therapeutic approaches, with a focus on lifestyle modifications, which have been shown to improve sexual function.
Methods
A literature search was performed and limited evidence for therapeutic approaches in individuals with SCI was supplemented by consistent findings from the able-bodied population.
Results
We evaluated the less addressed factors known to contribute to sexual dysfunction in men with SCI, including hormonal influences (i.e., testosterone deficiency, thyroid hormone, and cortisol), psychological factors (i.e., pain, fatigue, depression, and body image), and secondary SCI complications (i.e., urinary tract infection, pressure sores, and autonomic dysreflexia). To address these factors beyond standard medical treatments for sexual dysfunction, options include physical activity/exercise, diet, and specific medications for symptom relief (i.e., testosterone replacement therapy and selective serotonin reuptake inhibitors for depression).
Conclusions
Physical activity’s potential application, efficacy across multiple aspects of sexuality, and the lack of side effects, suggests that long-term exercise is a viable solution to directly or indirectly improve sexual function in males with SCI. Diet and supplemental medications may further promote body composition changes, which more broadly affect sexuality.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a devastating condition that can lead to pervasive medical complications. A systematic review of 24 studies, revealed sexual dysfunction (SD) to be a major functional priority for individuals with SCI, irrespective of the neurological level and completeness of injury [1]. Seminal survey data from over a decade ago highlighted sexual function as a top priority for persons with paraplegia above walking, bladder and bowel function, and pain, and the second top priority behind hand and arm function for quadriplegics [2]. Such sentiments are closely echoed in the recent North American Spinal Cord Injury Consortium Report from the SCI 2020 Panel and Consumer Survey, with the majority of survey respondents agreeing that restoring sexual function is important to them [3]. Worryingly, sexual function was found to be the area of greatest unmet need for persons with SCI [4].
There is often a focus on the neurological injury itself as the predominant factor for SD in men following SCI. However, SD can also be due to a combination of diverse factors such as hormonal abnormalities, psychological issues, and secondary SCI complications. Furthermore, the “accelerated aging” effect observed in individuals following SCI [5] contributes toward SD. The purpose of this review is to highlight these aforementioned components of SD in men with SCI, with a particular emphasis on relevant factors for sexuality which are less considered or appreciated by health care professionals. Possible treatment strategies (i.e., lifestyle factors and medications) to improve sexual function are suggested, drawing upon evidence from able-bodied individuals where relevant.
Overview of neurological SD in males with SCI
Erectile dysfunction (ED; defined as issues with sustaining and maintaining a reliable erection), impaired ejaculation, and the lack of orgasmic ability, which are predominately secondary to altered somatic and autonomic control, are the most common sexual complaints in men following SCI. The severity of these SDs reflect the level and completeness of the lesion [6]. SD also leads to sexual distress and even complications with fertility [6]. Different treatment options are available for men with SCI to address certain dysfunctions: for example, ED can be pharmacologically managed with a phosphodiesterase type V inhibitor (PDE5i), such as sildenafil [7, 8] and ejaculation can be promoted by the sympathomimetic midodrine [9] and/or penile vibrostimulation (PVS) [10]. PVS, along with electroejaculation (EEJ) are two sperm retrieval options used to pursue the potential of biological fatherhood following SCI [6]. However, the intense stimulus of PVS and EEJ can invoke autonomic dysreflexia, especially in men with cervical injuries [11]. Since the role of neurological impairment in sexual function in men with SCI has been previously described in detail elsewhere [6], this review will focus on less appreciated components that negatively impact sexual function following SCI.
Other components of sexuality
Hormonal changes in men with SCI
Testosterone
The hypothalamic pituitary gonadal (HPG) axis is the main regulator of the male sexual and reproductive system. Specifically, testosterone is a principle male sex hormone that is involved in bone and muscle growth [12], metabolism [13], visceral fat control [14], and sexual function [15, 16]. Hypogonadism is variously defined as a total serum testosterone level of <8–10 nmol/L [17] (~equivalent to <300 ng/dL) with sexual, psychological, and somatic symptoms that typically respond to exogenous testosterone replacement [18]. However, there is controversy regarding this definition of hypogonadism and some testosterone guidelines indicate a trial of testosterone therapy may be indicated for those with levels between 8 and 12 nmol/L in the presence of substantial symptoms [17]. The sexual symptoms of low testosterone levels include decreased libido and reduced nocturnal erections and ejaculate volume [19], and delayed ejaculation in the able-bodied population [20]. Low testosterone is also associated with depressive symptoms [21], which can influence sexual function in men (see below “Psychological issues and body self-image” section). Testosterone therapy may also modulate depressive symptoms in men with concomitant hypogonadism and depression [22].
In able-bodied individuals, the prevalence of hypogonadism increases with age, from 2.3% (in 20–29 age group) to 24.9% (in 70+ age group) [23]. In comparison, the majority of studies found low testosterone levels to be substantially more common in males with SCI than able-bodied controls [24,25,26,27,28]. Low testosterone levels are seen more frequently and at a younger age in men with SCI as compared with their able-bodied counterparts [24]. Younger men with SCI (18–45 years of age) have a 25% prevalence compared with 6.7% in similarly aged men without SCI [29]. Furthermore, the prevalence rises to 32.6% in men with SCI who also experience ED [29]. However, in the SCI population, it is challenging to determine if these clinical features (especially low sex drive, low mood, and fatigue) are due to the effect of the neurological injury itself or low testosterone levels, or an additive effect of both. One study demonstrated that low sexual desire was an independent predictor of low testosterone levels in men with chronic SCI [30].
Duration, level and completeness of injury can all affect testosterone levels after SCI. In acute SCI, the prevalence ranges from 69–83% whereas in chronic SCI, the prevalence ranges from 10–46%, likely reflecting the known gradual recovery of testosterone levels after acute injury or illness [31, 32]. While two studies indicated that males with tetraplegia had a higher prevalence of lower total testosterone levels than males with paraplegia [31, 33], two additional studies showed similar testosterone levels between injury classifications [24, 34]. One study found no significant difference in testosterone levels between incomplete or complete subdivision of each neurological classification [34]. However, the authors suggested a larger sample size may reveal lower testosterone levels for men with incomplete paraplegia, due to the potential alteration of the HPG axis resulting from lower motor neuron injuries [34]. The prevalence of low testosterone in this population is summarized in Table 1.
Although the etiology for low testosterone levels in men with SCI has not been explicitly clarified, the interplay between endocrine and metabolic systems should be considered. Specifically, hypogonadism in able-bodied individuals is often associated with metabolic disorders such as type-2 diabetes mellitus (T2DM) and metabolic syndrome (MetS), both well recognized in the etiology of SD [35]. Furthermore, the prevalence of T2DM in individuals with chronic SCI is 20% (notably three times higher than the general population [36]) and MetS is also elevated in individuals with SCI (~57%) [37]. Lower testosterone has been associated with higher Framingham risk scores, increased percent body fat, lower serum high density lipoprotein cholesterol, higher levels of inflammatory biomarkers (C-reactive protein and interleukin-6), and higher insulin resistance in men with SCI [38]. Therefore, low testosterone may contribute to increased cardiometabolic risk commonly observed in this population. In able-bodied individuals the association between metabolic disorders and hypogonadism is multidirectional; low testosterone levels can contribute to adipose tissue accumulation and insulin resistance [39, 40] and visceral adiposity can lead to low testosterone levels [41, 42]. In males with SCI, Barbonetti et al. reported that body mass index (BMI) was inversely associated with testosterone concentrations, explaining 9% of the variability in testosterone levels [30]. High BMI is a also a risk-factor for metabolic diseases like MetS and T2DM [43]. In summary, low testosterone levels are more prevalent in males with SCI than able-bodied men, with etiology suspected to be of both central and testicular origin, and tightly associated with concurrent metabolic disorders that are prevalent in men with SCI [36].
Other hormones
In the able-bodied population, hypothyroidism is a condition that is confirmed by elevated basal serum thyroid-stimulating hormone (TSH) and reduced triiodothyronine (T3) and thyroxine (T4). Hypothyroidism is associated with decreased sexual desire and an impaired ejaculatory reflex [44], as well as ED [45]. In individuals with chronic SCI, isolated low T3 level has been shown in 23% [46, 47], similar to 24% of individuals with acute heart failure [48]. This condition is called “low T3 syndrome”, and is associated with traumatic stress and critical illness, with the hypothesis that the conservation of energy leads to decreased basal metabolic rate during a time of negative caloric balance. In such patients, T3 usually normalizes after time, but this phenomenon often persists after SCI [46]. It is unknown whether sustained low T3 syndrome specifically would have a similar effect on sexuality as hypothyroidism. Moreover, the majority of men with SCI showed an abnormal response to hypothalamic releasing hormones (thyrotropin-releasing hormone), implicating a possible abnormality in central neurotransmitters after SCI [49]. These findings accentuate the need to clarify the effect of variable levels of T3 on components of sexuality after SCI. Interestingly, one study in men with SCI found that TSH and cortisol did not vary between a low testosterone group and normal testosterone group, suggesting that hypogonadism is not associated with the thyroid nor cortisol hypothalamic pituitary adrenal axis [33]. However, T3 was not measured in this study, therefore its specific association with testosterone remains to be elucidated.
Elevated concentrations of cortisol (hypercortisolemia) are linked with reduced libido in the able-bodied population [50]. The appropriate neuroendocrine response to a stressor such as traumatic SCI would include the dramatic elevation of cortisol and the loss of circadian rhythm, yet markers of cortisol and circadian rhythm typically return to normal levels within 6 months of injury [51]. However, inconsistency exists in the literature regarding cortisol levels in individuals with chronic SCI compared with able-bodied controls. One study found elevated mean plasma cortisol in an SCI group (n = 18) compared with able-bodied controls (n = 18) [52], while a smaller cohort study found no significant difference between mean morning cortisol levels of SCI group (n = 9) and control group (n = 9) [53]. Further research with larger sample sizes is necessary to determine an effect of cortisol on sexual function in men with chronic SCI.
Other factors that affect sexual function
Psychological issues and body self-image
Like in the able-bodied population, psychological issues such as depression, post-traumatic stress disorder [52], performance anxiety [53], and negative body image, can affect sexual function in men with SCI [54]. A bidirectional association often exists between SD (i.e., ED and decreased sexual libido) and depression in able-bodied individuals [55]. Depression is common in the SCI population, with a meta-analysis reporting a 22.2% (data combined across 19 studies) prevalence rate of clinically diagnosed symptomatic depression [56].
SD is reported to be prevalent in able-bodied individuals with chronic pain, which is also predicted by depression and pain duration [57]. Fatigue is a common issue in the SCI population, with a prevalence rate between 25 and 57% [58,59,60,61]. Specifically, fatigue is positively associated with pain and negatively associated with high mood in SCI cohorts [59, 62]. Chronic pain, ranging from nociceptive to neuropathic pain, is also a common secondary complication after SCI with overall pain prevalence estimated to be around 61% (±20%), data pooled from 82 studies [63]. Moreover, in a longitudinal SCI-cohort study, pain and poor mood were found to have a strong relationship [64], further emphasizing pain’s interplay with other psychological outcomes that affect sexual function.
Finally, when negative body image exists in the able-bodied population, the decreased frequency of sexual activity and avoidance of sexual behavior is observed [65]. A distorted and/or negative body image is a frequent presentation in individuals with SCI who experience a drastically altered body composition after the injury [66]. Interestingly, in a longitudinal cohort study conducted during inpatient rehabilitation, body image after SCI was found to explain part of the variance in depression during the program [67]. While outside the scope of this review, it is important for clinicians to also consider premorbid factors, such as personality issues, resiliency, communication skills, prior sexual experiences, and/or SDs and how these influence the capacity to allow for sexual reintegration after injury [68]. In younger men with SCI, it is possible that pre-injury sexual experience and attitudes may be key motivating factors prompting engagement in modifiable lifestyle behaviors.
Secondary complications of SCI and sexual functions
Due to secondary SCI complications, sexual activity can be socially constrained, and is often planned rather than spontaneous, further reducing enjoyment. Men with neurogenic bladder and bowel worry about the chance of bladder and bowel incontinence, this plus various catheter issues and associated odors not only provide physical barriers to sexual activities but also involve social inconvenience and embarrassment. The time required and inconvenience of a bowel protocol can interfere with sexual opportunities [69]. Similarly, pressure sores, restricted mobility and autonomic dysreflexia, can further complicate sexual opportunities and interest.
Pressure sores, produced by constant contact to a surface, are prevalent in 23–33% of the SCI population [70, 71]. They are most commonly seen in the gluteal-sacral region from wheelchair sitting [72], but certain sexual positions that place extensive weight on a particular body part, or skin friction during sexual activity, can increase the risk of pressure sore development. The presence of pressure sores (or other medical issues such as urinary tract infections) may hinder some sexual reflexes, such as ejaculation [6]. Mobility is also compromised after SCI, especially in individuals who do not retain any motor function in their lower extremities and/or have impaired hand function (i.e., higher-level motor-complete injuries). Consequently, men with SCI often have problems with sexual positioning and balance that require either upper extremity strength and/or abdominal or lower extremity motor control.
Sexual activity (including genital arousal, sexual activities, and especially ejaculation and orgasm) can induce an episode of autonomic dysreflexia (AD) in men and women with SCI [73, 74] and severe AD can often prohibit continued sexual activity. Interestingly, mild to moderate AD in some men with SCI correlates with pleasant arousal and can even be interpreted as an orgasmic release [10]. However, severe episodes of AD can result in devastating cerebrovascular consequences (i.e., hemorrhagic stroke) and in some instances can be fatal [75, 76]. This highlights the clinician’s responsibility to identify and inform SCI patients of their individualistic triggers (which includes sexual activity) for AD during rehabilitation.
Medications can also affect sexual function. For example, selective serotonin reuptake inhibitors for depression may cause SD as a side effect [77], intravesicular botulinum toxin can lead to decreased seminal volume (but is beneficial to semen quality by reducing bladder infections) [78], antispasmotics can reduce sexual reflexes, and opioids for chronic pain can lower testosterone levels [79]. Therefore, careful management of comorbid mood disorders, pain management, and pharmaceutical treatment strategies are warranted to further prevent SD in individuals with SCI.
Treatment
Blood pressure control
The prevention and reduction of AD in men during sexual activity can be aided by knowing when AD is accelerating and stopping activity, sitting up, and lowering the legs. A portable blood pressure (BP) cuff during sexual activities can provide valuable information on the extent of BP changes, as symptoms may not correlate with blood pressure elevation (silent AD) [6]. A recent systematic review emphasized the effectiveness of nifedipine to prevent AD during sperm retrieval procedures in males with SCI (10). Conversely, midodrine (often used to treat hypotension and promote ejactulation in men with SCI) has concerns due to its long-term cardiovascular risks in able-bodied population [80] and the fact that it diminishes lactate-induced testosterone release in preclinical models [81].
Testosterone replacement therapy (TRT)
TRT has been shown to improve SD in able-bodied individuals [82, 83], but has been insufficiently studied in men with SCI. Different types of testosterone administration include intramuscular injections, oral pills, pellets implanted subcutaneously, topical transdermal gels, patches, and nasal gel applications [84]. TRT has previously been advocated as a viable strategy to improve lean body mass and reduce fat mass in men with SCI [85]. However, exogenous testosterone supplementation is known to decrease sperm production in the able-bodied population due to the suppression of gonadotropin release [86]. Promising initial data with a nasal application of TRT (i.e., Natesto) demonstrated that gonadotropins remained in the normal range and had a minimal impact on semen parameters in able-bodied men [87]. This represents a promising alternative to other forms of TRT delivery (often with supra-physiological doses) for men with SCI that want to become fathers. However, this needs to be investigated further in the SCI population, especially since semen quality is negatively affected by SCI per se (6). While a recent literature review in able-bodied men suggested that cardiovascular risk and prostate cancer risk with TRT was shown to be minimal in properly screened patients [88], there is insufficient research on the efficacy and safety of TRT in men with SCI-specifically. In summary, TRT along with proper monitoring is a viable option to potentiate libido and sexual function, with the potential to preserve lean body mass in hypogonadal males with SCI.
Lifestyle modification
While lifestyle factors such as physical activity (PA)/exercise and an improved diet have been linked with better sexual function in able-bodied individuals [89, 90], to date no studies have longitudinally assessed the impact of these lifestyle modifications on sexual function specifically in an SCI-cohort. Therefore, this review primarily uses evidence in able-bodied individuals complimented with short-term limited data from SCI cohorts.
Diet and body composition
Diet can modulate body composition as well as promote an overall feeling of wellness and sexual attractiveness. There is insufficient information available on how diet can impact sexual function specifically in an SCI-cohort. In an obese able-bodied population, a low-energy diet with significant weight loss improved plasma testosterone levels, erectile function, and sexual desire [90]. It is important to ensure that any caloric deficit is sustainable long-term and that adequate protein intake is maintained (2.4 g per kg of body weight) to prevent the loss of lean mass [91]. In T2DM able-bodied men, both low-fat, high-protein, reduced-carbohydrate (HP) diet, and a low-calorie diet improved sexual desire, SHBG levels, and ED. The HP diet also reduced systemic inflammation leading to sustained beneficial effects at 1 year [92]. This suggests that although calorie restriction can improve sexual function, a high-protein and reduced-carbohydrate diet will most likely result in sustained effects. A recent randomised controlled trial (RCT) in able-bodied individuals with concomitant obesity and depression resulted in significant improvements in BMI and depressive symptoms [93]. As men with SCI often present with elevated visceral obesity [94] and symptoms of depression [56], this trial highlights the potential integration of diet into treating these two concomitant conditions.
There is inadequate evidence that any specific type of macronutrient, herb, or vitamin will modulate testosterone or impact sexual function. Persons with SCI are at risk for developing an unfavorable body composition such as visceral obesity [94] and lower-extremity skeletal muscle atrophy [95]. Given that such changes in body composition are associated with low testosterone [96, 97] and potentially negative body image, it may indirectly contribute to impaired sexual satisfaction. In the able-bodied population, higher volumes of exercise, which leads to greater energy expenditure and superior body composition changes, are required to impact testosterone levels [91]. It can be difficult to modulate body composition through exercise alone for persons with SCI, who are primarily limited to upper-body modalities for volitional exercise. These forms of exercise only elicit around 60–70% of energy expenditure compared with whole-body or leg exercise [98]. Further research is needed to determine if body composition (and thus testosterone levels and body image) is more effectively modulated via a combination of exercise and diet in order to have a beneficial impact on sexual satisfaction in men with SCI.
PA and exercise
In the SCI population, Barbonetti et al. demonstrated that weekly leisure time PA presented the most significant independent association with level of serum testosterone, explaining 54.2% of the variability in testosterone levels [30]. Of note, the majority of individuals with SCI are inactive [99], which potentially predisposes them to lower levels of testosterone. To date, the effects of long-term aerobic exercise on both testosterone and the interplay with sexual function have not been investigated in an SCI-cohort. In a small RCT (n = 17), 12 weeks of moderate-intensity arm-crank exercise improved reproductive hormone profile by increasing testosterone levels in men with chronic SCI, relative to a control group. [100]. While encouraging, these results are yet to be replicated in a larger SCI-cohort with concurrent assessments of sexual functioning. A Longitudinal RCT in able-bodied obese males (n = 75) reported that a considerable volume of moderate-intensity aerobic exercise (200–300 min per week) resulted in a greater improvement in testosterone levels and sexual function than low volume moderate-intensity exercise (90–150 min per week) [89]. This low volume of exercise is similar to the recently proposed SCI-specific exercise guidelines [101], which therefore may be inadequate. However, given the numerous psychosocial barriers to engage in exercise [102], it may be unrealistic for men with SCI to achieve the higher volume of moderate-intensity aerobic exercise (300 min per week) in order to see any impact on sexual function.
Preliminary preclinical evidence is emerging regarding the impact of high-intensity exercise on testosterone levels. Lactate, a by-product of intense anaerobic exercise (i.e., swimming for 10 min), has been shown to increase testosterone in a luteinizing hormone (LH)-independent manner in rats [81]. In addition, isolated rat Leydig cells that were incubated in the presence of lactate resulted in an increased production of basal testosterone [103]. These preclinical studies suggest that higher-intensity exercise may possibly mediate additional-HPG axis mechanisms of increasing testosterone. Promising data from male quadriplegic athletes demonstrated that an acute high-intensity exercise condition (i.e., maximal incremental exercise and a simulated 7.5 km race) resulted in a rise in testosterone similar to able-bodied men [104].
A recent systematic review highlighted that short-term (>4 weeks) resistance training in able-bodied older men (≥60 years of age) did not significantly influence basal testosterone whereas short-term (>4 weeks) aerobic and interval training resulted in small, yet significant rise in testosterone [105]. Conversely, another able-bodied study (not included in the aforementioned systematic review) revealed that twice-weekly resistance training for eight weeks, in comparison to control (nontrained participants), increased resting levels of serum testosterone [106]. The authors also reported a significant association between the percentage of type IIa skeletal muscle fibers and serum testosterone levels. Given the predominant shift in muscle fibers of paralysed lower extremities toward a fast glycolytic IIb phenotype after SCI [107], it is perhaps pertinent to consider different exercise modalities (i.e., aerobic and resistance training combined with certain lower extremity electrical stimulation paradigms) to modulate testosterone levels. An acute functional electrical stimulation (FES) assisted resistance training session, of various workloads, increased serum testosterone levels significantly in men with SCI, with no significant change in hematocrit or SHBG [108]. Furthermore, a recent RCT has also highlighted the possibility of combining resistance training with low-dose TRT in men with SCI, demonstrating an increase in total body lean mass in comparison to a TRT only group [109]. It is apparent that exercise-associated increase in testosterone levels can differ due to the modality, intensity, and duration of the activity. In order to fill the current knowledge gap, there is a pressing requirement for future studies to investigate the long-term effects of PA/exercise on testosterone levels, as well as other relevant hormonal changes in an already compromised population. Exercise is also shown to impact the pituitary-thyroid axis [110], but further research is needed to investigate the type of exercise that would enhance low T3 levels observed in individuals with SCI.
PA level is an important lifestyle factor that has been linked to improvements in various aforementioned psychological issues (i.e., fatigue, perceived body image, and mood disorders) [111,112,113], which affect male sexual function. A recent RCT with 180 min per week of home-based moderate-intensity exercise in individuals with SCI reported significantly lower fatigue levels and higher perceived physical functioning compared with the control group [111]. Other RCT studies in the SCI population have demonstrated improvements in pain, stress, and depression after combined aerobic and resistance training and higher satisfaction with physical function, level of perceived health, and overall quality of life [112, 114]. Martin-Ginis et al, [92] also reported better physical self-concept (i.e., perceived body image) with exercise. In addition, a recent cross-sectional study demonstrated that athletes with paraplegia had significantly higher sexual adjustment and higher body and sexual esteem than non-athletes with paraplegia [115]. A recent overview of systematic reviews confirmed that aerobic exercise and resistance training improves cardiorespiratory fitness and strength, respectively following SCI [115]. Such improvements in fitness and strength, along with reduced fatigue, and improved mood, may help improve endurance and mobility options during sexual activity, improving sexual motivation and enjoyment.
Pertinent considerations
There are several advantages of the aforementioned lifestyle modifications compared with medications to improve sexual function. Medications may have side effects that are unpleasant and sometimes hard to manage. Potential drug interactions can also influence SD. On the other hand, exercise is comparatively low-risk and is capable of alleviating multiple psychological morbidities. Due to its effects on diverse components of sexual function (i.e., mobility, psychological benefits, and testosterone levels), exercise is therefore a practical option that could be further advocated to improve sexual function in this population, in addition to achieving substantial benefits in other health outcomes.
Future directions
Sexuality after SCI is a complex interaction of hormonal, psychological, and other medical and neurological factors. Emerging therapies intended to help with other secondary complications of SCI can potentially aid or harm sexual function in men after SCI. Cannabis can potentially reduce pain in individuals with SCI [116]. However, in able-bodied men, tetrahydrocannabinol is associated with a decline in testosterone levels but with inconsistent subjective effects on sexual function [117]. Furthermore, while able-bodied men report increased sexual pleasure and satisfaction after cannabis use [118], men who use cannabis daily have also reported ED [119]. As the majority of these studies were conducted 40–50 years ago, these effects on men with SCI should be studied further in the context of contemporary cannabis products, particularly considering the evolving landscape with cannabis legalisation globally.
Neuromodulation is a novel therapy that has displayed promising improvements in crucial autonomic functions for individuals with SCI. Although demonstrated only in one female SCI participant, the ability to restore the capacity for orgasm was recently reported with epidural spinal cord stimulation [120]. Whether neuromodulation has the capacity to restore the neural control of erection, ejaculation, or orgasm in men with SCI represents an exciting avenue for future research.
Conclusion
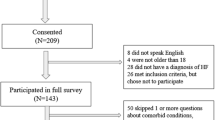
Sexual activity is recognized as essential to living a fulfilled life and should be available to everyone, irrespective of disability. The etiology of SD is multifactorial in this population: neurological impairment, low testosterone level, heightened psychological morbidity, and significant SCI-specific secondary consequences interfering with sexual function and activity (Fig. 1). Some medications and medical modifications that address specific components of sexual, bladder, and bowel dysfunction after SCI can be associated with detrimental side effects. Using established evidence from the able-bodied literature, various lifestyle behaviors (diet, PA, and exercise) that may directly or indirectly improve sexual function in men with SCI have been highlighted in this review. A combination of aerobic exercise and resistance training for a period of at least 4 weeks to improve sexual function would be advocated. We acknowledge that future research is required to elucidate the specific mechanisms whereby PA/exercise improves sexual function and quality of sexual activity, and to identify the most integral characteristics of these behaviors (i.e., intensity, volume, and type). Currently, evidence exists that PA is an effective, low-risk lifestyle behavior to modulate important quality of life components, fitness, mobility, and sex hormone concentrations that may facilitate improved sexual function in males with SCI. In addition, dietary modifications (i.e., altered macronutrient intake or caloric restriction), along with exercise, may be a promising avenue to modulate testosterone levels and indirectly benefit sexual function in men with SCI.
The solid lines represents the direct impact of secondary complications of spinal cord injury on sexual functioning and other components. Lifestyle factors, health-related quality of life, and hormone levels also mediate sexual function (dashed lines). In some instances, these links are bidirectional. Furthermore, there is interplay between lifestyle factors, hormone levels, and health-related quality of life outcomes (dotted lines).
References
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL. Team SCIRESR. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Consortium NASCI. NASCIC Report of SCI 2020 panel and consumer survey. Consortium NASCI; Cleveland, OH; 2020.
Kennedy P, Lude P, Taylor N. Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord. 2006;44:95–105.
Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M, et al. Spinal cord injury and aging: challenges and recommendations for future research. Am J Phys Med Rehabil. 2012;91:80–93.
Elliott S. Sexual dysfunction and infertility in individuals with spinal cord disorders. In: Kirshblum S, Lin VW, editors. Spinal cord medicine. Springer Publishing Company; New York, NY; 2018. p. 411–35.
Burns AS, Rivas DA, Ditunno JF. The management of neurogenic bladder and sexual dysfunction after spinal cord injury. Spine (Philos Pa 1976). 2001;26 Suppl 24 :S129–36.
Schmid DM, Schurch B, Hauri D. Sildenafil in the treatment of sexual dysfunction in spinal cord-injured male patients. Eur Urol. 2000;38:184–93.
Soler JM, Previnaire JG, Plante P, Denys P, Chartier-Kastler E. Midodrine improves ejaculation in spinal cord injured men. J Urol. 2007;178:2082–6.
Courtois F, Rodrigue X, Côté I, Boulet M, Vézina JG, Charvier K, et al. Sexual function and autonomic dysreflexia in men with spinal cord injuries: how should we treat? Spinal Cord. 2012;50:869–77.
Sheel AW, Krassioukov AV, Inglis JT, Elliott SL. Autonomic dysreflexia during sperm retrieval in spinal cord injury: influence of lesion level and sildenafil citrate. J Appl Physiol (1985). 2005;99:53–8.
van den Beld AW, de Jong FH, Grobbee DE, Pols HA, Lamberts SW. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J Clin Endocrinol Metab. 2000;85:3276–82.
Vermeulen A, Rubens R, Verdonck L. Testosterone secretion and metabolism in male senescence. J Clin Endocrinol Metab. 1972;34:730–5.
Tsai EC, Boyko EJ, Leonetti DL, Fujimoto WY. Low serum testosterone level as a predictor of increased visceral fat in Japanese-American men. Int J Obes Relat Metab Disord. 2000;24:485–91.
Corona G, Maggi M. The role of testosterone in erectile dysfunction. Nat Rev Urol. 2010;7:46–56.
Podlasek CA, Mulhall J, Davies K, Wingard CJ, Hannan JL, Bivalacqua TJ, et al. Translational perspective on the role of testosterone in sexual function and dysfunction. J Sex Med. 2016;13:1183–98.
Hackett GI. Controversies in the diagnosis and management of testosterone deficiency syndrome. CMAJ. 2015;187:1342–4.
Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N. Engl J Med. 2010;363:123–35.
Bhasin S, Enzlin P, Coviello A, Basson R. Sexual dysfunction in men and women with endocrine disorders. Lancet. 2007;369:597–611.
Corona G, Jannini EA, Mannucci E, Fisher AD, Lotti F, Petrone L, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–8.
Seidman SN, Weiser M. Testosterone and mood in aging men. Psychiatr Clin North Am. 2013;36:177–82.
Zarrouf FA, Artz S, Griffith J, Sirbu C, Kommor M. Testosterone and depression: systematic review and meta-analysis. J Psychiatr Pr. 2009;15:289–305.
Rohrmann S, Platz EA, Selvin E, Shiels MS, Joshu CE, Menke A, et al. The prevalence of low sex steroid hormone concentrations in men in the Third National Health and Nutrition Examination Survey (NHANES III). Clin Endocrinol (Oxf). 2011;75:232–9.
Bauman WA, La Fountaine MF, Spungen AM. Age-related prevalence of low testosterone in men with spinal cord injury. J Spinal Cord Med. 2014;37:32–9.
Durga A, Sepahpanah F, Regozzi M, Hastings J, Crane DA. Prevalence of testosterone deficiency after spinal cord injury. PM R. 2011;3:929–32.
Wang YH, Huang TS, Lien IN. Hormone changes in men with spinal cord injuries. Am J Phys Med Rehabil. 1992;71:328–32.
Safarinejad MR. Level of injury and hormone profiles in spinal cord-injured men. Urology. 2001;58:671–6.
Ibrahim E, Aballa TC, Roudebush WE, Lynne CM, Brackett NL. Inhibin B is lower and anti-Mullerian hormone is similar in serum of men with spinal cord injuries compared to controls. Syst Biol Reprod Med. 2015;61:72–7.
Behnaz M, Majd Z, Radfar M, Ajami H, Qorbani M, Kokab A. Prevalence of androgen deficiency in chronic spinal cord injury patients suffering from erectile dysfunction. Spinal Cord. 2017;55:1061–5.
Barbonetti A, Vassallo MR, Pacca F, Cavallo F, Costanzo M, Felzani G, et al. Correlates of low testosterone in men with chronic spinal cord injury. Andrology. 2014;2:721–8.
Schopp LH, Clark M, Mazurek MO, Hagglund KJ, Acuff ME, Sherman AK, et al. Testosterone levels among men with spinal cord injury admitted to inpatient rehabilitation. Am J Phys Med Rehabil. 2006;85:678–84. quiz 85–7.
Gaspar AP, Brandao CM, Lazaretti-Castro M. Bone mass and hormone analysis in patients with spinal cord injury: evidence for a gonadal axis disruption. J Clin Endocrinol Metab. 2014;99:4649–55.
Sullivan SD, Nash MS, Tefera E, Tinsley E, Blackman MR, Groah S. Prevalence and etiology of hypogonadism in young men with chronic spinal cord injury: a cross-sectional analysis from two university-based rehabilitation centers. PM R. 2017;9:751–60.
Clark MJ, Schopp LH, Mazurek MO, Zaniletti I, Lammy AB, Martin TA, et al. Testosterone levels among men with spinal cord injury: relationship between time since injury and laboratory values. Am J Phys Med Rehabil. 2008;87:758–67.
Corona G, Rastrelli G, Maggi M. Diagnosis and treatment of late-onset hypogonadism: systematic review and meta-analysis of TRT outcomes. Best Pr Res Clin Endocrinol Metab. 2013;27:557–79.
Lavela SL, Weaver FM, Goldstein B, Chen K, Miskevics S, Rajan S, et al. Diabetes mellitus in individuals with spinal cord injury or disorder. J Spinal Cord Med. 2006;29:387–95.
Gater DR Jr., Farkas GJ, Berg AS, Castillo C. Prevalence of metabolic syndrome in veterans with spinal cord injury. J Spinal Cord Med. 2019;42:86–93.
Sullivan SD, Nash MS, Tefara E, Tinsley E, Groah S. Relationship Between Gonadal Function and Cardiometabolic Risk in Young Men With Chronic Spinal Cord Injury. PM R. 2018;10:373–81.
Traish AM, Saad F, Guay A. The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J Androl. 2009;30:23–32.
Kapoor D, Goodwin E, Channer KS, Jones TH. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol. 2006;154:899–906.
Corona G, Mannucci E, Fisher AD, Lotti F, Petrone L, Balercia G, et al. Low levels of androgens in men with erectile dysfunction and obesity. J Sex Med. 2008;5:2454–63.
Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, et al. Hypothalamic-pituitarytesticular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008;93:2737–45.
World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO consultation. WHO technical report series; 894. World Health Organization; 2000.
Maggi M, Buvat J, Corona G, Guay A, Torres LO. Hormonal causes of male sexual dysfunctions and their management (hyperprolactinemia, thyroid disorders, GH disorders, and DHEA). J Sex Med. 2013;10:661–77.
Gabrielson AT, Sartor RA, Hellstrom WJG. The impact of thyroid disease on sexual dysfunction in men and women. Sex Med Rev. 2019;7:57–70.
Cheville AL, Kirshblum SC. Thyroid hormone changes in chronic spinal cord injury. J Spinal Cord Med. 1995;18:227–32.
Prakash V, Lin MS, Song CH, Perkash I. Thyroid hypofunction in spinal cord injury patients. Paraplegia. 1980;18:56–63.
Wang B, Liu S, Li L, Yao Q, Song R, Shao X, et al. Non-thyroidal illness syndrome in patients with cardiovascular diseases: a systematic review and meta-analysis. Int J Cardiol. 2017;226:1–10.
Huang TS, Wang YH, Chiang HS, Lien YN. Pituitary-testicular and pituitary-thyroid axes in spinal cord-injured males. Metabolism. 1993;42:516–21.
Valassi E, Santos A, Yaneva M, Toth M, Strasburger CJ, Chanson P, et al. The European Registry on Cushing's syndrome: 2-year experience. Baseline demographic and clinical characteristics. Eur J Endocrinol. 2011;165:383–92.
Cruse JM, Lewis RE Jr., Bishop GR, Kliesch WF, Gaitan E, Britt R. Decreased immune reactivity and neuroendocrine alterations related to chronic stress in spinal cord injury and stroke patients. Pathobiology. 1993;61:183–92.
Campagnolo DI, Bartlett JA, Chatterton R Jr., Keller SE. Adrenal and pituitary hormone patterns after spinal cord injury. Am J Phys Med Rehabil. 1999;78:361–6.
Culpepper-Morgan JA, Twist DJ, Petrillo CR, Soda KM, Kreek MJ. beta-Endorphin and cortisol abnormalities in spinal cord-injured individuals. Metabolism. 1992;41:578–81.
Barlow DH. Causes of sexual dysfunction: the role of anxiety and cognitive interference. J Consult Clin Psychol. 1986;54:140–8.
Atlantis E, Sullivan T. Bidirectional association between depression and sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2012;9:1497–507.
Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil. 2015;96:133–40.
Kwan KS, Roberts LJ, Swalm DM. Sexual dysfunction and chronic pain: the role of psychological variables and impact on quality of life. Eur J Pain. 2005;9:643–52.
Fawkes-Kirby TM, Wheeler MA, Anton HA, Miller WC, Townson AF, Weeks CA. Clinical correlates of fatigue in spinal cord injury. Spinal Cord. 2008;46:21–5.
Cudeiro-Blanco J, Onate-Figuérez A, Soto-León V, Avendaño-Coy J, Mordillo-Mateos L, Brocalero-Camacho A, et al. Prevalence of fatigue and associated factors in a spinal cord injury population: data from an internet-based and face-to-face surveys. J Neurotrauma. 2017;34:2335–41.
Lidal IB, Jensen AE, Larsen TW, Stanghelle JK. Fatigue in persons who have lived with spinal cord injury for >20 years. Spinal Cord. 2013;51:103–8.
Anton HA, Miller WC, Townson AF, Imam B, Silverberg N, Forwell S. The course of fatigue after acute spinal cord injury. Spinal Cord. 2017;55:94–7.
Hammell KW, Miller WC, Forwell SJ, Forman BE, Jacobsen BA. Fatigue and spinal cord injury: a qualitative analysis. Spinal Cord. 2009;47:44–9.
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015;19:5–14.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Faith MS, Schare ML. The role of body image in sexually avoidant behavior. Arch Sex Behav. 1993;22:345–56.
Fuentes CT, Pazzaglia M, Longo MR, Scivoletto G, Haggard P. Body image distortions following spinal cord injury. J Neurol Neurosurg Psychiatry. 2013;84:201–7.
van Diemen T, van Leeuwen C, van Nes I, Geertzen J, Post M. Body image in patients with spinal cord injury during inpatient rehabilitation. Arch Phys Med Rehabil. 2017;98:1126–31.
Alexander M, Courtois F, Elliott S, Tepper M. Improving sexual satisfaction in persons with spinal cord injuries: collective wisdom. Top Spinal Cord Inj Rehabil. 2017;23:57–70.
Benevento BT, Sipski ML. Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther. 2002;82:601–12.
Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in communityresident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993;74:1172–7.
Raghavan P, Raza WA, Ahmed YS, Chamberlain MA. Prevalence of pressure sores in a community sample of spinal injury patients. Clin Rehabil. 2003;17:879–84.
Richardson RR, Meyer PR. Prevalence and incidence of pressure sores in acute spinal cord injuries. Paraplegia. 1981;19:235–47.
Karlsson AK. Autonomic dysreflexia. Spinal Cord. 1999;37:383–91.
Elliott S, Krassioukov A. Malignant autonomic dysreflexia in spinal cord injured men. Spinal Cord. 2006;44:386–92.
Eltorai I, Kim R, Vulpe M, Kasravi H, Ho W. Fatal cerebral hemorrhage due to autonomic dysreflexia in a tetraplegic patient: case report and review. Paraplegia. 1992;30:355–60.
Pan SL, Wang YH, Lin HL, Chang CW, Wu TY, Hsieh ET. Intracerebral hemorrhage secondary to autonomic dysreflexia in a young person with incomplete C8 tetraplegia: a case report. Arch Phys Med Rehabil. 2005;86:591–3.
Rosen RC, Lane RM, Menza M. Effects of SSRIs on sexual function: a critical review. J Clin Psychopharmacol. 1999;19:67–85.
Caremel R, Courtois F, Charvier K, Ruffion A, Journel NM. Side effects of intradetrusor botulinum toxin injections on ejaculation and fertility in men with spinal cord injury: preliminary findings. BJU Int. 2012;109:1698–702.
Bawor M, Bami H, Dennis BB, Plater C, Worster A, Varenbut M, et al. Testosterone suppression in opioid users: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;149:1–9.
Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996;276:1328–31.
Lu SS, Lau CP, Tung YF, Huang SW, Chen YH, Shih HC, et al. Lactate and the effects of exercise on testosterone secretion: evidence for the involvement of a cAMP-mediated mechanism. Med Sci Sports Exerc. 1997;29:1048–54.
Wang C, Swerdloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G, et al. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab. 2000;85:2839–53.
Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl. 2008;29:102–5.
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone Therapy in Men With Hypogonadism: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2018;103:1715–44.
Nightingale TE, Moore P, Harman J, Khalil R, Gill RS, Castillo T, et al. Body composition changes with testosterone replacement therapy following spinal cord injury and aging. A mini review. J Spinal Cord Med. 2018;41:624–36.
Crosnoe LE, Grober E, Ohl D, Kim ED. Exogenous testosterone: a preventable cause of male infertility. Transl Androl Urol. 2013;2:106–13.
Masterson T, Molina M, Ibrahim E, Ramasamy R. Natesto effects on reproductive hormones and semen parameters: results from an ongoing single-center, investigatorinitiated phase IV clinical trial. Eur Urol Focus. 2018;4:333–5.
Traish AM. Benefits and health implications of testosterone therapy in men with testosterone deficiency. Sex Med Rev. 2018;6:86–105.
Khoo J, Tian HH, Tan B, Chew K, Ng CS, Leong D, et al. Comparing effects of low- and high-volume moderate-intensity exercise on sexual function and testosterone in obese men. J Sex Med. 2013;10:1823–32.
Khoo J, Piantadosi C, Worthley S, Wittert GA. Effects of a low-energy diet on sexual function and lower urinary tract symptoms in obese men. Int J Obes (Lond). 2010;34:1396–403.
Longland TM, Oikawa SY, Mitchell CJ, Devries MC, Phillips SM. Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: a randomized trial. Am J Clin Nutr. 2016;103:738–46.
Khoo J, Piantadosi C, Duncan R, Worthley SG, Jenkins A, Noakes M, et al. Comparing effects of a low-energy diet and a high-protein low-fat diet on sexual and endothelial function, urinary tract symptoms, and inflammation in obese diabetic men. J Sex Med. 2011;8:2868–75.
Ma J, Rosas LG, Lv N, Xiao L, Snowden MB, Venditti EM, et al. Effect of integrated behavioral weight loss treatment and problem-solving therapy on body mass index and depressive symptoms among patients with obesity and depression: the RAINBOW Randomized Clinical Trial. JAMA. 2019;321:869–79.
Edwards LA, Bugaresti JM, Buchholz AC. Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutr. 2008;87:600–7.
Gorgey AS, Dudley GA. Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord. 2007;45:304–9.
Srinivas-Shankar U, Roberts SA, Connolly MJ, O'Connell MD, Adams JE, Oldham JA, et al. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2010;95:639–50.
Abilmona SM, Sumrell RM, Gill RS, Adler RA, Gorgey AS. Serum testosterone levels may influence body composition and cardiometabolic health in men with spinal cord injury. Spinal Cord. 2018;57:229–39.
Reybrouck T, Heigenhauser GF, Faulkner JA. Limitations to maximum oxygen uptake in arms, leg, and combined arm-leg ergometry. J Appl Physiol. 1975;38:774–9.
Nightingale TE, Williams S, Thompson D, Bilzon JLJ. Energy balance components in persons with paraplegia: daily variation and appropriate measurement duration. Int J Behav Nutr Phys Act. 2017;14:132.
Rosety-Rodriguez M, Rosety I, Fornieles G, Rosety JM, Elosegui S, Rosety MA, et al. A short-term arm-crank exercise program improved testosterone deficiency in adults with chronic spinal cord injury. Int Braz J Urol. 2014;40:367–72.
van der Scheer JW, Ginis KAM, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Williams TL, Smith B, Papathomas A. The barriers, benefits and facilitators of leisure time physical activity among people with spinal cord injury: a meta-synthesis of qualitative findings. Health Psychol Rev. 2014;8:404–25.
Lin H, Wang SW, Wang RY, Wang PS. Stimulatory effect of lactate on testosterone production by rat Leydig cells. J Cell Biochem. 2001;83:147–54.
Wheeler G, Cumming D, Burnham R, Maclean I, Sloley BD, Bhambhani Y, et al. Testosterone, cortisol and catecholamine responses to exercise stress and autonomic dysreflexia in elite quadriplegic athletes. Paraplegia. 1994;32:292–9.
Hayes LD, Elliott BT. Short-term exercise training inconsistently influences basal testosterone in older men: a systematic review and meta-analysis. Front Physiol. 2018;9:1878.
Staron RS, Karapondo DL, Kraemer WJ, Fry AC, Gordon SE, Falkel JE, et al. Skeletal muscle adaptations during early phase of heavy-resistance training in men and women. J Appl Physiol (1985). 1994;76:1247–55.
Biering-Sorensen B, Kristensen IB, Kjaer M, Biering-Sorensen F. Muscle after spinal cord injury. Muscle Nerve. 2009;40:499–519.
Wheeler GD, Ashley EA, Harber V, Laskin JJ, Olenik LM, Sloley D, et al. Hormonal responses to graded-resistance, FES-assisted strength training in spinal cord-injured. Spinal Cord. 1996;34:264–7.
Gorgey AS, Khalil RE, Gill R, Gater DR, Lavis TD, Cardozo CP, et al. Low-dose testosterone and evoked resistance exercise after spinal cord injury on cardio-metabolic risk factors: an open-label randomized clinical trial. J Neurotrauma. 2019;36:2631–45.
Klubo-Gwiedzinska JB, Victor WL. Exercise and thyroid function. In: Constantini NH, Anthony C, editors. Endocrinology of physical activity and sport. New York: Humana Press; 2013.
Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99:1998–2006.e1.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J, et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord. 2003;41:34–43.
Tawashy AE, Eng JJ, Lin KH, Tang PF, Hung C. Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: a correlational study. Spinal Cord. 2009;47:301–6.
Ginis KAM, Latimer AE, McKechnie K, Ditor DS, McCartney N, Hicks AL, et al. Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol. 2003;48:157–64.
Eitivipart A, Oliveira CQ, Arora M, Middleton J, Davis G. Overview of systematic reviews of aerobic fitness and muscle strength training after spinal cord injury. J Neurotrauma. 2019;36:2943–63.
Wilsey B, Marcotte TD, Deutsch R, Zhao H, Prasad H, Phan A. An Exploratory Human Laboratory Experiment Evaluating Vaporized Cannabis in the Treatment of Neuropathic Pain From Spinal Cord Injury and Disease. J Pain. 2016;17:982–1000.
Kolodny RC, Masters WH, Kolodner RM, Toro G. Depression of plasma testosterone levels after chronic intensive marihuana use. N. Engl J Med. 1974;290:872–4.
Halikas J, Weller R, Morse C. Effects of regular marijuana use on sexual performance. J Psychoact Drugs. 1982;14:59–70.
Cohen S. Cannabis and sex: multifaceted paradoxes. J Psychoact Drugs. 1982;14:55–8.
Darrow D, Balser D, Netoff TI, Krassioukov A, Phillips A, Parr A, et al. Epidural spinal cord stimulation facilitates immediate restoration of dormant motor and autonomic supraspinal pathways after chronic neurologically complete spinal cord injury. J Neurotrauma. 2019;36:2325–36.
Funding
CARL was supported via the Summer Student Research Program and Flexible and Enhanced Learning Program within the Faculty of Medicine at the University of British Columbia. TEN is supported by a 2018/2019 Michael Smith Foundation for Health Research & International Collaboration on Repair Discoveries joint award (#17767). SE is a co-investigator on a Craig H. Neilsen Foundation (CNF), Creating Opportunity & Independence Sustainable Impact Project Grant. AVK laboratory is supported by funds from the Canadian Institute for Health Research, Heart and Stroke Foundation, Canadian Foundation for Innovation and the CNF.
Author information
Authors and Affiliations
Contributions
CARL and TEN were responsible for the conception and design of the article, searching the relevant literature, interpreting results, and drafting the manuscript. SE was responsible for the conception and design of the article, interpreting results, and contributed to writing the manuscript. AVK was responsible for oversight of the article, interpretation of the results, and provided feedback on the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This review article includes papers in which human volunteers were studied and assumes that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of the research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, C.A.R., Nightingale, T.E., Elliott, S. et al. Lifestyle modifications and pharmacological approaches to improve sexual function and satisfaction in men with spinal cord injury: a narrative review. Spinal Cord 58, 391–401 (2020). https://doi.org/10.1038/s41393-019-0404-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0404-z
This article is cited by
-
Sexual Dysfunction After Spinal Cord Injury
Current Sexual Health Reports (2020)