Abstract
Background and aims
The investigation of inflammatory background of hypertension (HTN) concentrates mainly on patients with primary HTN. The aim of the study was to analyze the role of new parameters of inflammation—lymphocyte to monocyte ratio (LMR), neutrophil to lymphocyte ratio (NLR), and platelet to lymphocyte ratio (PLR), in the population of children with primary (pHTN) and secondary renal hypertension (rHTN).
Material and methods
The study group consisted of 70 children with pHTN, 46 patients with rHTN, and 30 age-matched normotensive controls. The retrospective analysis focused on the evaluation of LMR, NLR, and PLR values in relation to blood pressure (BP) parameters from in-office and ambulatory BP monitoring measurements. Twenty-four hours, daytime, and nighttime periods were evaluated. Blood pressure variability (BPV) was defined by standard deviation and coefficient of variation of analyzed values.
Results
LMR and NLR values in HTN patients differed significantly vs. controls. Dippers with pHTN demonstrated significant correlations between LMR, NLR, PLR, and markers of BPV, in 24 h and daytime diastolic BP and mean arterial pressure. In dippers with rHTN such correlations concerned only LMR.
Conclusions
LMR may become a promising marker of BPV, useful in children with primary and secondary hypertension.
Impact
-
Lymphocyte to monocyte ratio is a novel marker of blood pressure variability, connected to target-organ damage, in children with primary and secondary renal hypertension.
-
Our study analyzes for the first time the connections between blood cell count-driven inflammatory markers (lymphocyte to monocyte, neutrophil to lymphocyte, and platelet to lymphocyte ratios) and parameters of blood pressure variability, and compares those ratios in children with primary and secondary hypertension.
-
The increasing incidence of hypertension among children urges the search for simple methods of assessment of its complications. LMR may be of added value in the analysis of the inflammatory background of hypertension.
Similar content being viewed by others
Introduction
The global prevalence of hypertension (HTN) in children is increasing, with a pooled estimate of 4%. Although the contribution of primary HTN (pHTN) follows the growing number of cases of childhood obesity, secondary HTN preponderates in the pediatric population.1 Among its causes, renal pathology is the most prevalent. Many studies have confirmed that HTN developed during childhood is the strongest independent predictor of HTN in adulthood and increases the risk of childhood and future target-organ damage.2,3,4 Introducing ambulatory blood pressure monitoring (ABPM) in children gave a new tool for HTN diagnosis, including observation of nocturnal dipping.5,6 Moreover, ABPM has shown to be more predictive of end-organ damage compared with office measurements.7
Despite diagnostic progress, pathogenesis of HTN still remains unclear. Working hypotheses on this multifactorial disease extend from the essential kidney role in sodium retention, through the paramount impact of peripheral vascular resistance, skin influence on both sodium stores and inflammatory responses, until the autoimmune background.8 Over the last years, subclinical low-grade inflammation has been concerned an important pathogenic factor in the wide spectrum of cardiovascular diseases, including HTN. The direct consequence of this interest was an increasing number of studies analyzing blood cell count (BCC)-derived indices in adults with cardiovascular disease, reviewed by Balta et al., Kurtul and Ornek, or Zamora et al.9,10,11,12 More recent investigation has concentrated on neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) as potential markers of inflammatory activity in hypertensive patients. The data on these parameters indicate the association between increased NLR and PLR in hypertensive adults and their role as predictors of dipper vs. non-dipper status.13,14,15 However, scarce studies on children gave so far contradictory results.16,17,18 Another BCC-derived marker, lymphocyte to monocyte ratio (LMR), has rather been attributed to the prognosis of survival in various types of cancer, including urothelial carcinoma.19,20 To the best of our knowledge, there are no studies evaluating the association between LMR and ABPM values, either in adults or children.
Aim of study
The aim of this study was to analyze the values of BCC-derived inflammatory markers (LMR, NLR, and PLR) in relation to the origin of HTN (primary vs. secondary renal) and established inflammation markers (C-reactive protein [CRP]), as well as to evaluate their correlation with blood pressure measurements in the population of children with HTN.
Methods
Study design and patient characteristics
This was a retrospective single-center study analyzing medical records of 184 children admitted to the Department of Pediatric Nephrology with the suspicion of HTN. HTN was diagnosed according to the European Society of Hypertension guidelines, based on three independent oscillometric office blood pressure measurements showing values over the 95th percentile for age, sex, and height.5 pHTN was diagnosed when all potential secondary causes of HTN (cardiological, endocrine, renal) were excluded. The overall exclusion criteria were age under 5 (due to the lack of ABPM device validation and age-related disparities in peripheral BCC and smear), previous antihypertensive pharmacotherapy, missing laboratory data (lack of complete blood smear), and impaired kidney function (estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2). All patients were hemodynamically stable and normovolemic. None of the patients presented with any signs of infection or exacerbation of the underlying kidney disease, or suffered from diabetes, metabolic syndrome, hyperlipidemia, cardiovascular disease, malignancies, connective tissue disease, vasculitides, or other systemic autoimmune diseases, on admission to the hospital.
One hundred thirty-six patients were divided into three groups. The first group consisted of 70 children with pHTN, the second group contained 46 patients with secondary renal hypertension (rHTN) and normal renal function.The control group consisted of 20 children with normal blood pressure values and normal kidney function, admitted for the diagnostics of nocturnal enuresis.
The causative factors for secondary rHTN were congenital anomalies of the kidney and urinary tract (22 children), polycystic kidney disease (6 patients), primary glomerulopathies (13 cases), secondary glomerulopathies (3 children), and fibromuscular dysplasia (2 patients). At the time point of data analysis, patients received no antihypertensive treatment. Basic clinical data are presented in Table 1.
The study was approved by the Wroclaw Medical University ethics committee. Retrospective informed consent was obtained from all available subjects involved in the study.
ABPM measurements
The 24-h ambulatory blood pressure measurements were performed with the device Oscar (SunTech Medical Inc., Morrisville, NC, USA). The analyzed parameters covered 24-h, daytime (D), and nighttime (N) observations of systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), mean arterial pressure (MAP), and pulse pressure (PP), as well as dipping (10% < dip < 20%) vs. non-dipping (dip < 10%) pattern. The group with pHTN contained 51 dippers and 19 non-dippers. In the rHTN group, there were 36 dippers and 10 non-dippers.
The variability of values of examined parameters was demonstrated with the use of standard deviation (SD) and coefficient of variation (CV).
Blood analysis
Complete BCC and serum chemistry were assessed during planned blood testing. Samples for BCC were collected in the tubes with ethylenediaminetetraacetic acid (EDTA) as an anticoagulant and analyzed within 2 h after sample collection. Complete BCC and manual assessment of peripheral blood smear were performed in all HTN patients and in the control group. Neutrophil, lymphocyte, monocyte, and platelet absolute counts per microliter were assessed and then subsequent ratios were evaluated: NLR, PLR, and LMR.
The serum creatinine was assessed with the modified Jaffé method, eGFR was calculated according to the Schwartz formula.21 High-sensitivity CRP was assessed by immunonephelometry with Siemens CardioPhase hsCRP reagent on the BN II System analyzer.
Statistical analysis
The results are expressed as mean values ± SD. Blood pressure variability (BPV) was defined by SD and CV.22 SD is the square root of the variance of BP readings, whereas CV (%) is the ratio of within-subject SD to the within-subject average BP, multiplied by 100. The latter defines the extent of variability in relation to the mean. The normality of distribution was evaluated by the Shapiro–Wilk test. Thus, the comparisons between normally distributed variables were evaluated by using the Student t-test, and between non-normally distributed by using nonparametric tests (Kruskal–Wallis, Mann–Whitney U). Relations between parameters were defined by Pearson’s correlation coefficient. Statistical analysis was performed using the package Statistica ver. 13.3 (StatSoft Inc., Tulsa, Oklahoma, USA). A p value of <0.05 was considered significant.
Results
LMR, NLR, and PLR values
BCC values, except for neutrophil count in children with rHTN, did not differ significantly between the control group and HTN patients (Table 2). The values of LMR were significantly lower, whereas NLR values were significantly higher, in patients with primary and secondary HTN when compared to the control group (Table 2). None of these parameters could differentiate between pHTN and rHTN or between dippers and non-dippers. In contrast, PLR values were increased only in patients with pHTN vs. controls (Table 2).
ABPM parameters
Patients with pHTN and rHTN demonstrated comparable values of 24 h, D, and N ABPM parameters (SBP, DBP, HR, MAP, PP) (Table 3).
Correlations of BCC parameters with ABPM measurements and CRP
In the group of all children with HTN, mean SBP, HR, and PP correlated with lymphocyte count, whereas mean SBP and PP correlated with platelet count (Table 4). SBP dip% correlated with monocyte count (Table 4). Within the subgroup of pHTN, SBP dip% and DBP dip% correlated with monocyte count. In rHTN patients, lymphocyte count correlated with mean HR, whereas platelet count correlated with mean SBP, MAP, and PP (Table 4). In addition, platelet count correlated with CRP (r = 0.25, p = 0.04) in pHTN patients.
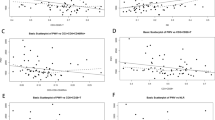
Correlations of LMR, NLR, and PLR with ABPM measurements and CRP
LMR and NLR correlated significantly with 24 h DBP SD and 24 h MAP SD in the group of all patients with pHTN. Within the subgroup of pHTN dippers, all examined parameters (LMR, NLR, and PLR) correlated significantly with 24 h DBP SD, DBP CV, MAP SD, MAP CV (Table 5). NLR and PLR correlated with D DBP SD, DBP CV, MAP SD, MAP CV (Table 5), whereas LMR correlated significantly with 24 h, D, and N mean PP and PP CV (Table 6). When patients with rHTN were analyzed, dippers demonstrated significant correlations of LMR with 24 h SYS and DBP SD and CV, as well as 24 h and N mean HR (Table 6).
PLR correlated with CRP (r = 0.28, p = 0.02) in patients with pHTN.
Discussion
Our investigation revealed variable values of NLR, PLR, and LMR, and their correlations with markers of BPV in children with non-treated primary and secondary rHTN.
Subclinical inflammation forms the background of many chronic diseases, including HTN. Neutrophils, the most abundant leukocytes in circulation, seem to play a major role in this process owing to their pro-inflammatory activity.23 Triggering increased oxidative stress, infiltration of tissues by immune cells, cytokine secretion, and fibrosis, leading to endothelial dysfunction.23 NLR was widely investigated in adults with HTN, and its increased values were found in non-dippers and in patients with resistant HTN.13,24 Consequently, NLR decreased in subjects with well-controlled BP values.25
Pediatric investigation proved the pro-inflammatory phenotype of essential HTN, but the evaluation of NLR gave contradictory results of its either increased or unchanged values in children with essential HTN.16,17,18 In our study group, NLR was higher in hypertensive vs. normotensive children. However, it failed to differentiate between primary and secondary rHTN. This observation suggests that the analyzed BCC-driven ratios may become useful markers of systemic low-grade inflammation, located rather in the circulation than in any particular organ, and independent of the HTN origin. Another interesting finding was the connection between NLR and BPV parameters, restricted to dippers with pHTN. Negative correlations with SD and CV of mean DBP and MAP have shown the tendency of increasing NLR together with decreasing BPV. Whether this could suggest a shift from a dipping to a non-dipping pattern, is yet to be elucidated in the course of future investigation.
Meanwhile, the problem is of paramount importance because recent investigation suggests that a non-dipping pattern in adults is associated with aggravated target-organ damage, increased cardiovascular risk, and mortality. Indeed, adult hypertensive non-dippers presented with higher values of NLR and PLR than dippers.13 A similar analysis in children with secondary rHTN gave contradictory results of dipper – non-dipper difference in the case of PLR.26 There was no such distinction in our analysis. However, the number of non-dippers in our study did not exceed 20 subjects in any of the subgroups, which could make the results of the statistical analysis irrelevant. Moreover, the proportion of non-dippers (27% of pHTN patients, 22% of rHTN patients) was reversed to that in adulthood, where they dominated, mainly because of a high prevalence of diabetes. In pediatric reports, the frequency of non-dipping patterns varied from 40% in pHTN to 68% in rHTN children.18,26 So far, there was no investigation on NLR usefulness as a predictor of diminishing beat-to-beat BPV and this perspective should be verified in the course of a prospective trial.
PLR analysis also revealed discrepant results. In our study, PLR demonstrated increased values in children with pHTN and unchanged in rHTN. Similarly, Cetin et al., who analyzed the population of children with secondary rHTN, observed unchanged PLR in non-dippers, but decreased PLR in dippers.26 However, the correlations between platelet count and ABPM parameters (24 h mean SBP and PP) concerned all our patients with HTN, similarly to other reports.18 These results could imply the unique role of platelets in the pathogenesis of HTN-related inflammation, strengthened by the fact that CRP correlated with platelet count and PLR in children with pHTN. Indeed, PLR is an established marker of systemic inflammation.10,11,12 Moreover, adult studies stress the role of PLR in the prediction of target-organ damage and cardiovascular events. The finding of negative correlations between DBP, MAP SD, and CV gave surge to the search of predictive potential of increasing PLR vs. decreasing BPV, but verification of this hypothesis requires a larger group of patients observed in a prospective way. Yet, the interpretation of PLR values requires taking into account specific methodological restrictions, e.g., the EDTA-dependent pseudothrombocytopenia.10 Thus, a comparison of the values in hypertensive patients with those gained under the same conditions in controls makes the obtained results more reliable.
LMR was the least investigated ratio in the literature among the three examined inflammatory markers, and has not been tested so far in patients with HTN. It was also the only ratio, out of the three analyzed, taking into account the monocyte count. The complex role of monocytes in the pathogenesis of HTN results from their pleiotropic functions.27 Their most evident features are migratory activity, accumulation in the organs, in situ chemokine/cytokine secretion, ROS production, and transformation into macrophages. Monocyte migration into vascular endothelium triggers inflammation and arterial wall remodeling due to connective tissue proliferation. No doubt, these phenomena lead to increased systemic vascular resistance—a hallmark of HTN. Moreover, a recent investigation revealed monocyte/neutrophil tight connections with coagulation processes. In detail, tissue factor, a key element of the coagulation cascade, is expressed on both monocytes and neutrophils.28 Such functional versatility of monocytes suggests their potential as markers of HTN-driven complications. Surprisingly, LMR has not been tested so far in hypertensive conditions. However, its value as a predictor of bad prognosis and poor survival has been described in oncological patients, including those with non-metastatic renal cell carcinoma.29,30
In our study, the significance of monocyte and lymphocyte counts was evident even in the whole cohort of children with HTN and its importance systematically increased together with the specification of subgroups. Like NLR and PLR, LMR correlated with BPV indexes in dippers with pHTN. Contrary to other parameters, such connections were also revealed in the case of rHTN dippers. This bond between BPV and LMR, independent of the type of HTN, holds a promise of LMR as a universal marker, connecting subclinical inflammation with features characterizing the risk of target-organ damage in the course of HTN and bad prognosis. Unfortunately, these correlations failed to reveal their predictive value on multivariate logistic regression, probably because of the insufficient number of patients. Thus, our preliminary results require verification in the course of a prospective study performed on a larger group of patients, securing better differential analysis between dippers and non-dippers, as well as in-detail evaluation of subgroups with various underlying causes of secondary rHTN.
Finally, we have to acknowledge the limitations of our study. The values of BCC-derived inflammatory markers are variable and strongly dependent on unstable conditions like chronic inflammation or volemia. Moreover, sample preparation may trigger method-related bias. The retrospective design could create another bias, similarly to the overall small number of patients, the aggravation of this problem with the additional subdivision of patients into dippers and non-dippers, and the reverse proportion of the latter when compared to adults. Moreover, this was the first attempt to compare the values of inflammatory ratios between the homogenous population of children with pHTN and the heterogenous group of patients with HTN secondary to kidney disease. All above-mentioned limitations urge the continuation of this investigation in a larger group of patients, looked at from a broader perspective.
Conclusions
Our preliminary results suggest that BCC-driven markers carry information about the inflammatory status of children with HTN, irrespective of its origin. Special attention should be paid to LMR that seems a potential tool in the assessment of BPV parameters in both primary and secondary HTN. Whether analyzed ratios become useful in the evaluation of BPV evolution toward non-dipping patterns in children with HTN, is yet to be established in the course of a larger prospective study.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Song, P. et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. 173, 1154–1163 (2019).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180 (2008).
Sarganas, G., Schaffrath, R. A., Niessner, C., Woll, A. & Neuhauser, H. K. Tracking of blood pressure in children and adolescents in Germany in the context of risk factors for hypertension. Int J. Hypertens. 2018, 8429891 (2018).
Theodore, R. F. et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension 66, 1108–1115 (2015).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Rao, G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics 138, e20153616 (2016).
Flyn, J. T. et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension 63, 1116–1135 (2014).
Wenzel, U. O., Ehmke, H. & Bode, M. Immune mechanisms in arterial hypertension. Recent advances. Cell Tissue Res. 385, 393–404 (2021).
Balta, S. et al. The relation between atherosclerosis and the neutrophil-lymphocyte ratio. Clin. Appl Thromb. Hemost. 22, 405–411 (2016).
Balta, S. & Ozturk, C. The platelet-lymphocyte ratio: a simple, inexpensive and rapid prognostic marker for cardiovascular events. Platelets 26, 680–681 (2015).
Kurtul, A. & Ornek, E. Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology 70, 802–818 (2019).
Zamora, C., Cantó, E. & Vidal, S. The dual role of platelets in the cardiovascular risk of chronic inflammation. Front Immunol. 12, 625181 (2021).
Sunbul, M. et al. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin. Exp. Hypertens. 36, 217–221 (2014).
Kılıçaslan, B. et al. The relationship between neutrophil to lymphocyte ratio and blood pressure variability in hypertensive and normotensive subjecs. Turk. Kardiyol. Dern. Ars. 43, 18–24 (2015).
Liu, X. et al. Blood neutrophil to lymphocyte ratio as a predictor of hypertension. Am. J. Hypertens. 28, 1339–1346 (2015).
Hou, M. et al. Neutrophil to lymphocyte ratio is increased and associated with left ventricular diastolic function in newly diagnosed essential hypertension children. Front Pediatr. 9, 576005 (2021).
Litwin, M. et al. Inflammatory activation in children with primary hypertension. Pediatr. Nephrol. 25, 1711–1718 (2010).
Skrzypczyk, P. et al. Complete blood count-derived inflammatory markers in adolescents with primary arterial hypertension: a preliminary report. Cent. Eur. J. Immunol. 43, 434–441 (2018).
Hutterer, G. C. et al. Pretreatment lymphocyte-monocyte ratio as a potential prognostic factor in a cohort of patients with upper tract urothelial carcinoma. J. Clin. Pathol. 68, 351–355 (2015).
Balta, S., Demırer, Z., Aparci, M., Yildirim, A. O. & Ozturk, C. The lymphocyte-monocyte ratio in clinical practice. J. Clin. Pathol. 69, 88–89 (2016).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Boubouchairopoulou, N., Ntineri, A., Kollias, A., Destounis, A., & Stergiou, G. S. Blood pressure variability assessed by office, home, and ambulatory measurements: comparison, agreement, and determinants. Hypertens Res. 44, 1617–1624. https://doi.org/10.1038/s41440-021-00736-9 (2021).
Araos, P., Figueroa, S. & Amador, C. A. The role of neutrophils in hypertension. Int J. Mol. Sci. 21, 8536 (2020).
Belen, E., Sungur, A., Sungur, M. A. & Erdoğan, G. Increased neutrophil to lymphocyte ratio in patients with resistant hypertension. J. Clin. Hypertens. (Greenwich) 17, 532–537 (2015).
Karaman, M. et al. The comparative effects of valsartan and amlodipine on vWf levels and N/L ratio in patients with newly diagnosed hypertension. Clin. Exp. Hypertens. 35, 516–522 (2013).
Cetin, N. & Tufan, A. K. Platelet activation and inflammation in hypertensive children with non-dipper and dipper status. Int J. Kidney Dis. 13, 105–112 (2019).
Wenzel, P. Monocytes as immune targets in arterial hypertension. Br. J. Pharmacol. 176, 1966–1977 (2019).
Rothmeier, A. S. et al. Caspase-1-mediated pathway promotes generation of thromboinflammatory microparticles. J. Clin. Invest 125, 1471–1484 (2015).
Gu, L. et al. Prognostic role of lymphocyte to monocyte ratio for patients with cancer: evidence from a systematic review and meta-analysis. Oncotarget 7, 31926–31942 (2016).
Garcia-Rojo, D. et al. Prognostic value of lymphocyte-to-monocyte ratio previously determined to surgery in patients with non-metastatic renal cel carcinoma. Medicine 100, e24152 (2021).
Author information
Authors and Affiliations
Contributions
Conceptualization: K.M., A.B.-G., P.M.; investigation: K.M., A.B.-G., P.M., M.G., S.G.; resources: P.M., M.G., S.G.; formal analysis: K.M., P.M., M.G.; writing—original draft: K.M., A.B.-G., P.M.; writing—review and editing: K.M., D.Z.; visualization: K.M., P.M., M.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures were performed in accordance with the 1964 Helsinki Declaration and its further amendments. Retrospective informed consent was obtained from all available subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Musiał, K., Bargenda-Lange, A., Mazurkiewicz, P. et al. Lymphocyte to monocyte ratio and blood pressure variability in childhood hypertension—a pilot study. Pediatr Res 93, 137–142 (2023). https://doi.org/10.1038/s41390-022-02056-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02056-1
This article is cited by
-
Systemic inflammation markers and the prevalence of hypertension: A NHANES cross-sectional study
Hypertension Research (2023)