Abstract
Background
The physiological benefit of parent–infant skin-to-skin contact (SSC) is uncertain for preterm infants with ventilatory support. We aimed to investigate whether SSC stabilizes the respiration compared to incubator care in mechanically ventilated preterm infants.
Methods
The prospective observational study was performed in Turku University Hospital, Finland. Preterm infants were eligible if they were born before 36 weeks gestation and received respiratory support with either invasive or non-invasive neurally adjusted ventilatory assist (NAVA). SSC was applied as soon as possible after birth. Respiratory variables were collected from the ventilator log data, and SSC episodes were compared with matched control periods during incubator care.
Results
A total of 167 episodes of SSC were recorded from 17 preterm infants: 138 episodes during invasive NAVA and 29 episodes during non-invasive NAVA. During invasive NAVA, peak electrical activity of the diaphragm (Edi), minimum Edi, respiratory rate, time on backup ventilation, peak inspiratory pressure, and mean airway pressure were significantly lower in SSC than in incubator care. During non-invasive NAVA, peak Edi, minimum Edi, time on backup ventilation, and peak inspiratory pressure were significantly lower in SSC than in incubator care.
Conclusions
SSC stabilized and improved the respiratory physiology in mechanically ventilated preterm infants.
Impact
-
Skin-to-skin contact reduced work of breathing compared to incubator care in mechanically ventilated preterm infants.
-
Skin-to-skin contact reduced the need for backup ventilation during neurally adjusted ventilatory assist in preterm infants.
-
Skin-to-skin contact among ventilated preterm infants was not only safe but also stabilized and improved their respiratory physiology.
Similar content being viewed by others
Introduction
Parent–infant skin-to-skin contact (SSC) not only promotes breast feeding and parent–infant bonding but also decreases the risk of sepsis and death in premature infants.1,2,3 In terms of the physiological benefits of SSC, it has been shown that SSC stabilizes heart rate (HR), respiratory rate (RR), and body temperature when compared to standard care (incubator, radiant warmer, or open crib) in clinically stable preterm infants.4,5,6,7 However, several studies have failed to show significant physiological benefits in preterm infants who are critically ill or on mechanical ventilatory support.8,9,10,11,12 Other studies report that SSC increases HR, RR, and transcutaneous CO2 pressure as well as irregular breathing in preterm infants on respiratory support.13,14,15,16 Uncertainty regarding the physiological risks or benefits may be a barrier to the wider implementation of SSC in preterm infants receiving ventilatory support.1,2,16,17,18
Neurally adjusted ventilatory assist (NAVA) is a ventilatory mode that allows the patient to synchronize the ventilatory support with his/her spontaneous respiratory effort by detecting the electrical activity of the diaphragm (Edi). The Edi signal can be used to study the breathing effort. The Edi values also reflect the patient’s work of breathing and enable the estimation of diaphragmatic energy expenditure.19,20
We compared the neural pattern of breathing during SSC and during incubator care in preterm infants who were supported by NAVA. We hypothesized that the breathing pattern would be more stable during SSC than in incubator care.
Methods
This prospective observational cohort study took place from March 2020 to December 2020 in the level III neonatal intensive care unit of Turku University Hospital, where all infants were cared in single-family rooms. Preterm infants were eligible if they were born before 36 weeks of gestation and received ventilatory support with either invasive or non-invasive NAVA using a Servo-i or Servo-n ventilator (Getinge, Gothenburg, Sweden). SSC was initiated as soon as possible after birth, regardless of the type of ventilatory support chosen. SSC was mainly provided during the day, lasting one feeding interval (2–3 h) at a time, but could also be provided for longer periods, including the feeding time. A reclining chair was prepared at the side of the incubator in which the infant was cared. When the parent reclined on the chair, one nurse gathered all the infant’s lines and tubes with disconnection of the ventilator tube for a short time. Simultaneously, another nurse transferred the infant and placed him or her prone on the parent’s chest. The ventilator tube was reconnected and secured over the parent’s shoulder. During SSC, infants were held in a head-tilt prone position, naked except for a nappy, lying on the chest of their mother or father, who was resting in a semi-reclining position. The infants’ heads were covered by a woollen hood and their bodies by a cotton blanket.
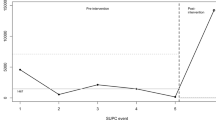
The data on ventilator settings and respiratory variables were collected from the ventilators every day and exported into a specific computer using the Servo Record Viewer version 1.0 (Maquet Critical Care AB, Getinge, Gothenburg, Sweden). From the 24-h data, we identified the SSC episode by using the nursing records and the ventilator event logs. An equally length control period without handling or procedures was selected from the following night, between 11 p.m. and 5 a.m., while the infant was placed in the incubator. We excluded the first 10 min of data to have a washout period for each recording. The beginning of the control period was matched with SSC in terms of the time since the previous feeding: for example, if the SSC began 30 min after a feeding, the control period also began 30 min after a feeding (Fig. 1).
The skin-to-skin contact (SSC) intervention was selected and first 10 min of data was excluded to secure a washout period. An equally length control period without handling or procedures was selected from the following night, between 11 p.m. and 5 a.m., while the infant was placed in the incubator. The beginning of the control period was matched with SSC in terms of the time since the previous feeding.
The following clinical characteristics were collected from medical records: gestational age at birth, birth weight, the time and amount of feeding, medications during the study days, desaturation events, bradycardia events, and any procedures. Postmenstrual age (PMA) and day of life at the time of SSC were calculated. If there was any use of analgesics or sedatives, we excluded this period from the analysis for both SSC and control. The oxygen saturation target ranged from 90 to 95% during the entire study period. Desaturation and bradycardia events were defined as SpO2 < 80% and HR < 80 bpm, respectively. The following respiratory data were collected from the ventilator: peak Edi, minimum Edi, measured RR, neural RR (nRR) and the percentage of time on backup breath, supplied oxygen fraction, peak inspiratory pressure, peak end-expiratory pressure, mean airway pressure, and expiratory tidal volume for each minute. All ventilator data were inspected and compared with the event logs recorded automatically from the ventilator, which include all information about alarm notifications, mode and setting changes, cable connections, and disconnections. Data collected during the disconnection of the Edi cable or the malfunction or dislocation of the Edi catheter were excluded. The analyses were performed separately for the days on invasive and non-invasive NAVA.
The study was approved by the Ethics Committee of the Hospital District of Southwest Finland, as well as by the Scientific Research Committee of the Pediatric Department of Turku University Hospital, Finland. Written informed consent was obtained from both parents according to the guidelines of the Research and Ethics Board before the patient was enrolled in this study.
Categorical variables were analyzed using Fisher’s exact test. Respiratory parameters were compared between SSC and incubator care using the paired T test or the Wilcoxon signed-rank test, as appropriate. A P value < 0.05 was considered to be statistically significant. Statistical analyses were performed using SPSS v. 27.0 (IBM, Armonk, NY, USA).
Results
Seventeen preterm infants, born at a median (range) 27+4 (23+4–33+5) weeks of gestation with a median (range) birth weight of 1000 g (460–2820), were included in the study. Eight (47%) infants had bronchopulmonary dysplasia (BPD), defined as a need for supplemental oxygen at PMA 36 weeks. The included number of SSC episodes per each infant was median (range) 5 (1–31). A total of 167 episodes of SSC were selected and compared to matched controls during incubator care; 138 episodes took place during invasive NAVA and 29 during non-invasive NAVA. The proportion of SSC performed in infants having BPD were 91% (126/138) and 48% (14/29), respectively. The duration of SSC was median (range) 166 min (63–392) per episode. Clinical details and ventilator settings at the time of SSC are described in Table 1.
During invasive NAVA, peak Edi, minimum Edi, measured RR, nRR, time on backup ventilation, peak inspiratory pressure, and mean airway pressure were significantly lower in SSC than in incubator care (Table 2). Expiratory tidal volume and dynamic compliance were significantly higher in SSC than in incubator care. There was no difference in the supplied oxygen fraction and positive end-expiratory pressure. During non-invasive NAVA, peak Edi, minimum Edi, time on backup ventilation, and peak inspiratory pressure were significantly lower in SSC than in incubator care (Table 2). Other respiratory parameters did not differ between SSC and incubator care during non-invasive NAVA.
When we compared SSC and incubator care performed at under 28 weeks of PMA, peak Edi and minimum Edi were significantly lower in SSC than in incubator care. Other respiratory values did not differ between SSC and incubator care (Table 3). For episodes at ≥28 weeks of PMA, peak Edi, minimum Edi, measured RR, nRR, time on backup ventilation, peak inspiratory pressure, and mean airway pressure were significantly lower in SSC than in incubator care. Expiratory tidal volume was significantly higher in SSC than in incubator care. There was no difference in the supplied oxygen fraction and positive end-expiratory pressure.
There was no difference in the number of desaturations or bradycardias between SSC and incubator care during either invasive or non-invasive NAVA (Table 4). No accidental extubation or loss of venous access occurred during SSC. None of the infants needed to discontinue SSC due to physiological instability.
Discussion
This study showed that preterm infants receiving ventilatory support exerted less breathing effort and their neural breathing was more stable during SSC than in incubator care. These beneficial effects related to SSC were more evident after 28 weeks GA and during invasive ventilation than non-invasive ventilation. Ventilatory support is often regarded as a barrier to the implementation of SSC with sick preterm infants,16,17,18 and SSC is currently recommended as the standard of care for low birth weight infants after stabilization as earlier and as continuously as possible.2,19 Our results not only support the safety of SSC but also provide evidence about the physiological benefits of SSC in ventilated preterm infants.
As peak Edi reflects the respiratory work of patients,20,21 lower peak Edi indicated that the infants exerted less breathing effort during SSC. Minimum Edi, reflecting the tonic activity of the diaphragm,22 was also lower during SSC than during incubator care, which is in line with our previous results.13 This indicated better relaxation of the diaphragm between respiratory cycles during SSC, which further decreased work of breathing.
There are several explanations for why SSC contributes to respiratory unloading. Intimate skin contact has been shown to have a buffering effect on pain and stress reactivity, mediated by increased oxytocin and decreased cortisol release during SSC.1,17,23 Our previous study showed that pain score changes were similar to the changes in peak Edi during NAVA.24 Therefore, decreased pain and stress may explain lower peak Edi values during SSC. In addition, the respiratory unloading effect of SSC may be related to the prone position of the infant on the parent’s chest. It has been reported that, in preterm infants, the prone position improves oxygenation and lung ventilation,25,26,27 as well as induces more sleep and less stress responses than the supine position.28,29,30 Additionally, sleep and behavioral states have been shown to influence breathing in premature infants.26,31
Decreased pain and stress may also explain the reduced RR during SSC among invasively ventilated infants, as we have shown in this study. Similarly, a recent meta-analysis demonstrated that SSC was associated with a lower RR than conventional care.1 Previous studies reporting the effects of SSC on apnea have been contradictory; however, most of the studies included non-intubated infants.1,14,32,33 In our study, though RR was lower during SSC, SSC seemed to promote spontaneous breathing, detected as a decrease in time spent on backup ventilation (Tables 2 and 3). This result suggests that SSC can stabilize breathing and enhance spontaneous breathing in sick preterm infants under stressful ventilatory support.
We showed that, together with decreased peak inspiratory pressures and mean airway pressures during invasive NAVA, SSC improved dynamic compliance and resulted in higher tidal volumes with the same ventilator settings. Even if reduced peak Edi during SSC lead to a reduction in inspiratory pressures,21 the tidal volumes increased. This indicates that SSC affected the lung dynamics, allowing the lungs to expand more easily. In this study, most of the study recordings were collected from infants who had evolving or established BPD. There have been no studies directly aiming to show that SSC could decrease BPD. A recent study reported that single-family room care lowered the risk for BPD (adjusted odds ratio 0.72, 95% confidence interval 0.61–0.86).34 Our results can be a potential explanation for the mechanism behind this association, because single-family room care is related to more frequent and longer SSC.35
Our study has limitations. First, we did not specifically address the effect of position. Infants mostly lie in a prone and upward-tilted position during SSC. Meanwhile, infants may lie in either prone or supine positions, and upward tilting is rarely chosen during incubator care. Nevertheless, because the position is one part of SSC, our comparison included all elements of SSC. Second, SSC episodes were measured repeatedly from each infant and the majority of study recordings were from infants having BPD. It could emphasize the effect of SSC on infants who received prolonged respiratory support and influences on the lung physiology may not be the same at an individual infant level. However, our results rather demonstrate beneficial effects of SSC especially in preterm infants with BPD who need lengthy mechanical ventilation.
In conclusion, this is the first study showing that SSC stabilizes and improves respiratory physiology in mechanically ventilated preterm infants. Our results provide evidence about the advantages of SSC during ventilatory support, especially in preterm infants with BPD. In addition, better tidal volumes with lower pressures could even suggest that SSC could be helpful in reducing the severity of BPD in this vulnerable population. The effects of SSC on breathing and long-term respiratory morbidities deserve more research in the future.
References
Boundy, E. O. et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics 137, e20152238 (2016).
Conde-Agudelo, A. & Díaz-Rossello, J. L. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst. Rev. 8, CD002771 (2016).
Nyqvist, K. H. et al. Towards universal kangaroo mother care: recommendations and report from the first European Conference and Seventh International Workshop on Kangaroo Mother Care. Acta Paediatr. 99, 820–826 (2010).
Bergman, N. J., Linley, L. L. & Fawcus, S. R. Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for physiological stabilization in 1200- to 2199-gram newborns. Acta Paediatr. 93, 779–785 (2004).
Kommers, D. R. et al. Features of heart rate variability capture regulatory changes during kangaroo care in preterm Infants. J. Pediatr. 182, 92–98.e1 (2017).
Kommers, D. R. et al. Changes in autonomic regulation due to Kangaroo care remain unaffected by using a swaddling device. Acta Paediatr. 108, 258–265 (2019).
Lorenz, L. et al. Cerebral oxygenation during skin-to-skin care in preterm infants not receiving respiratory support. Arch. Dis. Child. Fetal Neonatal Ed. 103, F137–F142 (2018).
Bloch-Salisbury, E., Zuzarte, I., Indic, P., Bednarek, F. & Paydarfar, D. Kangaroo care: cardio-respiratory relationships between the infant and caregiver. Early Hum. Dev. 90, 843–850 (2014).
Heimann, K. et al. Impact of skin to skin care, prone and supine positioning on cardiorespiratory parameters and thermoregulation in premature infants. Neonatology 97, 311–317 (2010).
Lorenz, L. et al. Skin-to-skin care in preterm infants receiving respiratory support does not lead to physiological instability. Arch. Dis. Child. Fetal Neonatal Ed. 102, F339–F344 (2017).
Maastrup, R. & Greisen, G. Extremely preterm infants tolerate skin-to-skin contact during the first weeks of life. Acta Paediatr. 99, 1145–1149 (2010).
Soukka, H., Grönroos, L., Leppäsalo, J. & Lehtonen, L. The effects of skin-to-skin care on the diaphragmatic electrical activity in preterm infants. Early Hum. Dev. 90, 531–534 (2014).
Carbasse, A. et al. Safety and effectiveness of skin-to-skin contact in the NICU to support neurodevelopment in vulnerable preterm infants. J. Perinat. Neonatal Nurs. 27, 255–262 (2013).
Bohnhorst, B., Heyne, T., Peter, C. S. & Poets, C. F. Skin-to-skin (kangaroo) care, respiratory control, and thermoregulation. J. Pediatr. 138, 193–197 (2001).
Begum, E. A. et al. Cerebral oxygenation responses during kangaroo care in low birth weight infants. BMC Pediatr. 8, 51 (2008).
Bisanalli, S., Nesargi, S., Govindu, R. M. & Rao, S. P. Kangaroo mother care in hospitalized low birth-weight infants on respiratory support: a feasibility and safety study. Adv. Neonatal Care 19, E21–E25 (2019).
Pados, B. F. & Hess, F. Systematic review of the effects of skin-to-skin care on short-term physiologic stress outcomes in preterm infants in the neonatal intensive care unit. Adv. Neonatal Care 20, 48–58 (2020).
Smith, E. R., Bergelson, I., Constantian, S., Valsangkar, B. & Chan, G. J. Barriers and enablers of health system adoption of kangaroo mother care: a systematic review of caregiver perspectives. BMC Pediatr. 17, 35 (2017).
Bergman, N. J. et al. European Standards of Care for Newborn Health: very early and continuous skin-to-skin contact. https://newborn-health-standards.org/skin-to-skin-contact/ (2018).
Brander, L. et al. Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest 135, 695–703 (2009).
Beck, J. et al. Characterization of neural breathing pattern in spontaneously breathing preterm infants. Pediatr. Res. 70, 607–613 (2011).
Emeriaud, G., Beck, J., Tucci, M., Lacroix, J. & Sinderby, C. Diaphragm electrical activity during expiration in mechanically ventilated infants. Pediatr. Res. 59, 705–710 (2006).
Bhat, R. Y. et al. Effect of posture on oxygenation, lung volume, and respiratory mechanics in premature infants studied before discharge. Pediatrics 112, 29–32 (2003).
Elder, D. E., Larsen, P. D., Galletly, D. C. & Campbell, A. J. Cardioventilatory coupling in preterm and term infants: effect of position and sleep state. Respir. Physiol. Neurobiol. 174, 128–134 (2010).
Shepherd, K. L. et al. When does prone sleeping improve cardiorespiratory status in preterm infants in the NICU? Sleep 43, zsz256 (2020).
Peng, N.-H. et al. The effect of positioning on preterm infants’ sleep-wake states and stress behaviours during exposure to environmental stressors. J. Child Health Care 18, 314–325 (2014).
Jarus, T. et al. Effects of prone and supine positions on sleep state and stress responses in preterm infants. Infant Behav. Dev. 34, 257–263 (2011).
Bastani, F., Rajai, N., Farsi, Z. & Als, H. The effects of kangaroo care on the sleep and wake states of preterm infants. J. Nurs. Res. 25, 231–239 (2017).
Mörelius, E., Örtenstrand, A., Theodorsson, E. & Frostell, A. A randomised trial of continuous skin-to-skin contact after preterm birth and the effects on salivary cortisol, parental stress, depression, and breastfeeding. Early Hum. Dev. 91, 63–70 (2015).
Nam, S. K., Lee, J. & Jun, Y. H. Neural feedback is insufficient in preterm infants during neurally adjusted ventilatory assist. Pediatr. Pulmonol. 54, 1277–1283 (2019).
Lehtonen, L. & Martin, R. J. Ontogeny of sleep and awake states in relation to breathing in preterm infants. Semin. Neonatol. 9, 229–238 (2004).
Charpak, N., Ruiz-Peláez, J. G., Figueroa de C., Z. & Charpak, Y. A randomized, controlled trial of kangaroo mother care: results of follow-up at 1 year of corrected age. Pediatrics 108, 1072–1079 (2001).
Suman Rao, P. N., Udani, R. & Nanavati, R. Kangaroo mother care for low birth weight infants: a randomized controlled trial. Indian Pediatr. 45, 17–23 (2008).
Lehtonen, L. et al. Family rooms in neonatal intensive care units and neonatal outcomes: an international survey and linked cohort study. J. Pediatr. 226, 112–117.e4 (2020).
Raiskila, S. et al. Parents’ presence and parent–infant closeness in 11 neonatal intensive care units in six European countries vary between and within the countries. Acta Paediatr. 106, 878–888 (2017).
Acknowledgements
The authors would like to thank the Baby Friendly Ventilation Study Group. We are also grateful to all the parents, nurses, and medical staff of the neonatal intensive care unit of Turku University Hospital for their willingness to assist with the study. This study was supported by the Inha University Hospital research grant.
Author information
Authors and Affiliations
Contributions
J.L. conceptualized and designed the study, collected data, carried out analyses, and drafted the manuscript. V.P. collected data and reviewed and revised the manuscript. L.L. reviewed and revised the manuscript for important intellectual content. H.S. participated in the design of the study, collected data, and reviewed and revised the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Informed parental consents were obtained prior to study participation and the study was approved by the Ethics Committee of Hospital District of Southwest Finland (Approval number TO8/004/20).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J., Parikka, V., Lehtonen, L. et al. Parent–infant skin-to-skin contact reduces the electrical activity of the diaphragm and stabilizes respiratory function in preterm infants. Pediatr Res 91, 1163–1167 (2022). https://doi.org/10.1038/s41390-021-01607-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01607-2
This article is cited by
-
A pivotal moment in the evolution of neonatal care
Journal of Perinatology (2023)