Abstract
Background
Oral propranolol has become first-line treatment for infantile hemangiomas (IHs). This study focused on identifying cytokines related to the biology of IH and early regression indicators of IH after propranolol treatment.
Methods
For inclusion, the patients had to be aged less than 1 year and have an IH with a largest diameter ≥2 cm. Patients were scheduled to receive 1 year of propranolol treatment. Serum cytokines involved in angiogenesis, vasculogenesis, and/or chronic inflammation were analyzed at 0, 1, and/or 12 months after treatment using Multiplex Luminex assays.
Results
Among the 49 evaluable patients, 33 completed the 1-year treatment: 16 showed excellent response and 12 had good response to propranolol. Significant decreases in serum MMP-2, bFGF, VEGF-α, and MCP-1 levels were observed after 1 year of treatment compared to pretreatment values. The maximal diameters of the lesions significantly correlated with pretreatment serum VEGF-α, bFGF, and MMP-9. Patients with higher bFGF and VEGF levels showed better response to propranolol at 1 year.
Conclusion
MMP-2, VEGF-α, bFGF, and MCP-1 may involve in the biology of IH and their downregulation may be associated with involution processes of IH. Pretreatment bFGF and VEGF could be novel biomarkers for predicting response to propranolol.
Impact
-
We found that decreases in the concentrations of MMP-2, bFGF, VEGF, and MCP-1 were associated with regression of the hemangioma, which indicates that one of the mechanisms of propranolol in the treatment of proliferative hemangiomas may involve downregulation of those cytokines.
-
Patients with higher bFGF and VEGF levels showed better response to propranolol at 1 year. Importantly, serum bFGF higher than 37.07 pg/mL may predict an excellent response to propranolol. Therefore, along with the patient’s age and the size and visual characteristics of the lesion, bFGF levels could help determine the viability of propranolol use in the treatment of IHs.
-
Our study represented extensive serum profiling in IH, reporting the indicators and molecules clearly related to IH regression with propranolol treatment. The authors believe that monitoring serum cytokines, including MMP-2, bFGF, VEGF, and MCP-1, in IH patients could be important, in addition to clinical follow-up, for determining when to start and end propranolol treatment.
Similar content being viewed by others
Introduction
Infantile hemangiomas (IHs) are the most common benign childhood soft tissue tumor associated with the abnormal proliferation of vascular endothelial cells. IH affects 4−10% of infants with a predilection for female, low birth weight, and premature infants.1,2,3 The unique feature of IH is its natural development, which includes a phase of intensive growth (proliferation) lasting up to 18 months and a phase of slow disappearance (involution).4 Unfortunately, both the onset of the involution phase and its duration are unpredictable. Occasionally, IHs grow rapidly to a significant size around the first 1–2 months of life, which can be problematic and even destroy normal tissue. Although some researchers suggest that disruptions occurring during the angiogenesis stage play an important role in the pathogenesis, we still do not understand the complex biology of its rapid proliferation and spontaneous regression.
Clinical practice in recent years has shown that propranolol exerts a rapid, curative effect in the treatment of IHs with few adverse reactions.5,6 While the mechanisms of vasoconstriction by this drug have been described in detail, the mechanisms behind the spectacular IH involution after propranolol treatment remain unclear. Recently, there has been strong evidence of the overexpression of numerous angiogenic factors in IH tissues, and propranolol has been reported to influence their pathways. Vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) are known to be consistently expressed in IH tissues, and both have been shown to play an important role in IH biology.7 Recently, the presence of matrix metalloproteinase (MMP)-2, -9 was confirmed in the urine of IH patients, and MMP-2 was found in hemangioma tissue.8,9 The role of MMPs, which not only can promote the release of the angiogenic factors VEGF and bFGF to induce angiogenesis, but can also degrade the extracellular matrix and promote the migration of endothelial cells, has scarcely been investigated in IH.10
Currently, early molecular markers to predict responses to propranolol in patients with IH are lacking, and no accepted clinical marker is available that can monitor the progression of IH or the success of systemic treatment, which directly informs the therapeutic plan. Therefore, we analyzed cytokines involved in angiogenesis, vasculogenesis, and inflammation such as VEGF, bFGF, platelet-derived growth factor-BB (PDGF-BB), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-1 beta (MIP-1β), MMP-2, MMP-9, tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), interleukin-1 beta (IL-1β), IL-2, and IL-4 in serum samples from IH patients before treatment and at 1 and 12 months after propranolol treatment. This study focused on identifying the possible therapeutic mechanisms of propranolol and early indicators of IH regression after propranolol treatment. In addition, analyses of the clinical efficacy and safety of propranolol in IH patients were also performed.
Materials and methods
Patient recruitment
This was a multicenter prospective study conducted on behalf of the Korean Pediatric Hematology Oncology Group (K-PHOG) of the Korean Society of Pediatric Hematology-Oncology. Eleven medical centers participated in this study between May 2015 and December 2018. For inclusion, the patient had to be aged less than 1 year and have an evaluated IH lesion with a largest diameter at least 2 cm or bigger showing steady growth. For IHs with deep-seated component, Doppler US and/or MRI was recommended to assess the lesion. Patients with cardiovascular disorders that contraindicated propranolol use, a history of hypoglycemic episodes, recent outbreaks of wheezing, hypersensitivity to propranolol, PHACE syndrome (posterior fossa brain malformations, hemangioma, arterial lesions, cardiac abnormalities, and eye abnormalities), Kasabach−Meritt syndrome, and a prior history of hemangioma treatment were excluded from the study. This study was approved by the IRB of each participating center. Written informed consents were signed by the guardians of the children enrolled.
Propranolol treatment
Once the relevant examinations were performed to confirm the absence of any contraindications, the propranolol treatment was started. The recommended treatment scheme was as follows: patients were started on oral propranolol at 0.5 mg/kg/day in two divided doses and monitored for any cardiovascular (e.g., symptomatic bradycardia or hypotension) and metabolic side effects (e.g., hypoglycemia) over 24 h. If the patient showed no adverse events, the dosage was increased every 24 h up to 2–3 mg/kg/day (day 1, 0.5 mg/kg/day; day 2, 1 mg/kg/day; day 3, 2 mg/kg/day; day 4, 3 mg/kg/day). The dose of propranolol was adjusted according to the child’s body weight during follow-up visits. Propranolol was administered for 12 months and stopped with or without tapering at the physician’s discretion.
Clinical efficacy criteria
The clinical response to propranolol was evaluated at 1 and 12 months after treatment. Response to treatment was evaluated for each lesion with a largest diameter ≥2 cm and mainly assessed using the visual analog scale (VAS) (Table 1).5 The VAS score ranges from 0 (representing no improvement) to 9 (representing complete resolution), and was evaluated by one designated reviewer at each medical center after reviewing all clinical photographs of the IHs at baseline and after the full course of treatment. In case of multiple lesions, the score was determined based on the average improvement of each lesion. Therapeutic responses were graded as follows: excellent response (VAS score ranging from 7 to 9), good response (VAS score ranging from 4 to 6), poor response (VAS score ranging from 1 to 3), and no response (VAS score 0).
Blood collection and serum cytokine profiling
Blood samples were collected from the patients pretreatment and at 1 and 12 months after initiation of propranolol treatment. The 1- and 12-month samples were collected at a median of 35 and 404 days after propranolol treatment, respectively. The samples were placed in a serum separating tube (SST), kept static at room temperature for 30 min, and then subjected to centrifugation at 2000 × g to isolate the serum. The serum was transferred to an Eppendorf (EP) tube and preserved below −20 °C for subsequent testing. Following collection of the samples, the serum concentrations of VEGF, bFGF, PDGF-BB, MCP-1, MIP-1β, MMP-2, MMP-9, TNF-α, IFN-γ, IL-1β, IL-2, and IL-4 were detected using Multiplex Luminex assay using xPONENT 3.1 software.
Statistical analysis
Paired sample comparisons were performed using the paired t test. Analysis of variance (ANOVA) was used for comparison of multiple groups. Correlations between each cytokine concentration and the lesion size, VAS score, and age were analyzed using the nonparametric Spearman’s correlation coefficient (r). Receiver operating characteristic (ROC) analysis was carried out to verify whether values were able to significantly discriminate the predictor of an excellent treatment response from the samples of all patients, accounting for sensitivity and specificity. Two-sided p < 0.05 was considered statistically significant. Data were expressed as mean ± standard deviation. All statistical analyses were performed using SPSS software, version 19.0 (SPSS Inc. Chicago, IL).
Results
Among 63 recruited patients, four who did not meet the inclusion criteria were excluded. Six patients were lost to follow-up and four patients were withdrawn due to their guardians’ request after 1 month of treatment. Among the 49 evaluable patients, 33 completed the 1-year treatment with timely blood samples. The remaining 16 patients were still receiving propranolol at the time of data cut-off; therefore, they were evaluable only at the time points pretreatment and after 1 month of treatment.
Clinical characteristics and the efficacy of propranolol
Baseline characteristics of the patients are presented in Table 2. Patients received oral propranolol at a median age of 87 days, ranging between 27 days and 301 days. There were 26 boys and 23 girls. Hemangiomas were isolated in 37 patients (75.5%), while multifocal lesions were found in the remaining 12 (24.5%). Sixty IHs were found in 49 patients. More than half of the patients had a lesion of the head. The localization sites included (number of lesions in parentheses): scalp,6 periorbital,5 perioral,4 nose,6 other face area,10 neck,6 trunk,12 arm,6 hand,2 foot,1 and others.2 Of these, we only evaluated the clinical response of lesions with a largest diameter of ≥2 cm.
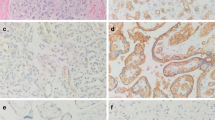
Patients were receiving propranolol at a dose of 2.31 ± 0.52 mg/kg/day and 2.32 ± 0.56 mg/kg/day at 1 month and 12 months of treatment, respectively. At 1 month of propranolol treatment, the clinical response to propranolol was assessed in 49 patients: the results showed the curative effect to be excellent in 1 patient (2%), good in 19 patients (38.8%), and poor in 23 patients (46.9%). Six patients (12.2%) showed no response to propranolol at 1 month of treatment. At 1 year of oral propranolol treatment, the clinical response to propranolol was assessed in 33 patients. All patients showed a response to propranolol to varying degrees: excellent VAS scores were recorded in 16 patients (48.5%), including 8 patients showing complete involution; 12 patients (36.4%) showed good VAS scores, and 5 patients (15.2%) showed poor VAS scores (Fig. 1).
The 1-year VAS score was not associated with the age at treatment initiation (p = 0.115), maximal diameter (p = 0.237), or 1-month VAS score (p = 0.096). Among 37 patients with single lesion, 19 patients showed IHs with deep-seated component. The 1-year VAS score was significantly higher in patients with deep-seated component compared to those without (6.9 ± 4.8 vs. 4.8 ± 2.6, p = 0.04).
During treatment, four cases of adverse events were recorded, all of which occurred within 1 month after treatment initiation: asymptomatic hypotension ± bradycardia occurred in three patients during the dose-adjustment phase, and one patient showed transaminase elevation. All events were classified as mild or moderate in severity, and none led to treatment discontinuation.
Changes in the serum cytokines
Serum cytokines before and after 1 month of treatment were evaluated in 49 patients and 1-year follow-up study was performed in 33 patients. Among 12 cytokines examined by the Multiplex Luminex assay, the values of five cytokines, including PDGF-BB, TNF-α, IFN-γ, IL-1β, IL-2, and IL-4 were mostly out of measurable range and therefore could not be analyzed in this study. Most of the result of PDGF-BB showed >3140 pg/mL, which exceeded the scale, while most of the results for TNF-α, IFN-γ, IL-1 β, IL-2 and IL-4 were below the measurable range at <9.3, <50.74, <19.79, <36.95, and <15.06 pg/mL, respectively. Hence, the data of VEGF, bFGF, MCP-1, MIP-1 β, MMP-2, and MMP-9 were conclusively analyzed in this study.
The serum MMP-2 levels were 503,827 ± 162,614 pg/mL before starting the treatment, 455,058 ± 134,505 pg/mL after 1 month of treatment, and 354,945 ± 127,891 pg/mL after 1 year of treatment. The mean pretreatment MMP-2 values differed significantly from the 1-month and 1-year follow-up values (p = 0.001 and p < 0.001, respectively) (Fig. 2). Although there were no significant differences between the pretreatment serum bFGF, VEGF and MCP-1 levels and those after 1 month of treatment, there were significant decreases in the serum bFGF, VEGF, and MCP-1 levels after 1 year of propranolol treatment compared to the pretreatment values (32.6 ± 33.1 to 14.8 ± 15.6 pg/mL, p < 0.001; 190.9 ± 142.9 to 126.8 ± 80.4 pg/mL, p = 0.001; and 4422.8 ± 8748.8 to 352.8 ± 347.3 pg/mL, p = 0.008, respectively) (Fig. 3).
The maximal diameters of the lesions showed significantly positive correlations with serum VEGF (r = 0.552, p < 0.01), bFGF (r = 0.525, p < 0.01), and MMP-9 (r = 0.33, p = 0.025) at pretreatment (Fig. 4). There were no correlations between age and those three cytokines before propranolol treatment. We could not find significant difference in levels of cytokines between IH with and without deep-seated component.
There were statistically significant correlations between the outcomes of propranolol treatment and the pretreatment levels of bFGF and VEGF. Patients with higher bFGF and VEGF levels showed higher VAS scores at 1 year (p = 0.001 and p = 0.048, respectively). ROC analysis demonstrated that serum bFGF could predict the response to propranolol, with an area under the curve (AUC) of 0.767 (p = 0.01); bFGF levels higher than 37.07 pg/mL suggested an excellent response at 1 year after treatment with 73.3% sensitivity and 82.4% specificity (Fig. 5). There was no correlation between the degree of changes in the bFGF or VEGF values during treatment and the clinical improvement of IH.
Discussion
Propranolol, the well-known nonselective β-blocker, has become the standard treatment for IH since its incidental discovery in 2008.11 All patients included in the present study showed a clinical response to propranolol at a mean dosage of 2.3 mg/kg/day, with a reduction in the size of the hemangimas and obvious fading. No serious adverse effects were observed during 1-year follow-up. Short-time hypotension and bradycardia were reported in a few cases and they were clinically asymptomatic and modifiable. Our results are consistent with those of many previous clinical reports and support the role of propranolol as a first-line treatment in IH.5,12
In in vitro studies, propranolol was found to inhibit the proliferation of hemangioma endothelial cells and induce apoptosis.13,14,15 A few theories have postulated that these actions are attributable to the promotion of apoptosis of endothelial cells via β-adrenergic receptors and the caspase pathway and inhibition of angiogenesis via regulation of vascular growth factor.13,16,17 Some research showed the serum levels of VEGF, bFGF and MMP-9 fell significantly during the course of propranolol therapy.18 In this study, we found significant decreases in serum MMP-2, bFGF, VEGF, and MCP-1 after the course of propranolol therapy, which may be associated with involution process and suggests the possible mechanisms of propranolol in the treatment of IH. Conversely, these could be the potentially useful signs to monitor vascular growth during and/or after propranolol treatment.
Currently, one of the most highly investigated area of IH biology is the VEGF pathway, and VEGF is the most potent angiogenic factor in the growth of hemangioma. It improves vascular permeability, stimulates endothelial cell proliferation, and prevents apoptosis.19,20 In this study, we found significant changes in the serum levels of VEGF between pre- and post-treatment. Furthermore, higher VEGF was associated with a better clinical outcome after propranolol treatment. There were some studies investigating the effect of propranolol on VEGF in hemangioma. Tu et al.21 previously reported that exposure of hemangioma endothelial cells to 50−100 μmol/L of propranolol in culture media caused significant reduction of VEGF concentration. Chim et al.13 suggested that decreased VEGF activity by propranolol was mediated through the hypoxia inducible factor (HIF)-1α. Recent studies suggest that the VEGF-mediated mechanism of endothelial progenitor cell proliferation, together with mobilization through MMPs, plays a key role in the formation of hemangiomas.22,23 It is likely that propranolol has widespread activity through multiple signaling pathways: β-adrenoreceptor agonists can increase the expression of MMP-2 and MMP-9. This is consistent with our findings of higher VEGF and MMP-9 levels in IHs with larger diameters. Furthermore, we found that MMP-2 levels, but not MMP-9 levels, were found to fall after treatment. Taran et al.24 previously confirmed the activation of MMP-2 pathways in IH tissue and highlighted the influence of propranolol therapy on their expression. They suggested that the serum evaluation of MMP-2 could be a valuable complement to that measured in IH tissue. In our study, at 1 month after treatment, a significant change was found in the serum MMP-2 only, which may represent a suitable early biomarker reflecting the action of propranolol.
In a previous study,25 it was suggested that by downregulating the expression of the Raf/MAPK pathway, propranolol could decrease the expression of VEGF and bFGF during treatment. bFGF is a strong angiogenetic and mitotic polypeptide with a protein structure that stimulates the formation and proliferation of new blood vessels. There are only a few studies on bFGF,20,26,27 though it is an important marker in the pathogenesis of hemangioma. In this study, we found higher bFGF levels in larger hemangiomas, which suggests that bFGF may play a role in IH pathogenesis. Recently, Babiak-Choroszczak et al.27 reported a significant decrease in bFGF during and after treatment compared to the pretreatment values. Moreover, there was a correlation between the outcome of the Doppler ultrasonography and the changes in bFGF during and after propranolol treatment. Our results confirm the correlation between high levels of bFGF and the proliferative phase of IH. Furthermore, we found that pretreatment bFGF was predictive of the response to propranolol; bFGF higher than 37.07 pg/mL was associated with a VAS score ≥7 with 73.3% of sensitivity and 82.4% of specificity. These results suggest that bFGF could be a feasible biological marker for IH and that its expression level may predict the degree of lesion improvement after propranolol treatment. Therefore, along with the patient’s age and the size and visual characteristics of the lesion, bFGF levels could help determine the viability of propranolol use in the treatment of IHs.
Chemokines in general, and MCP-1 in particular, are known to control vessel distribution and branching points; their direct targets such as monocytes and macrophages have been called the “architects” of vessel development.28 MCP-1 mRNA has been previously shown to be elevated in hemangioma issues and related to hemangioma onset.29 D’Arcangelo et al.30 found that MCP-1 levels significantly discriminate IH in the proliferating phase from IH in the regressing phase; 466.5 pg/mL in infants ≤12 months of age vs. 238.3 pg/mL in infants >24 months of age, p = 0.0016. In our study, a greater than 90% reduction in serum MCP-1 at 1 year of treatment was observed throughout the group compared to the pretreatment values. These data may represent strong evidence of the involvement of MCP-1 in the mechanism of propranolol treatment in IH.
The results presented in the current study demonstrate strong statistical significance, and represent extensive serum profiling in IH, reporting the indicators and molecules clearly related to IH regression with propranolol treatment. However, there are some limitations in this study. We included a small number of patients and had no control group, as the very low age made it difficult to recruit a larger number of patients. Currently, in light of medical ethics, and the well-documented beneficial effects of propranolol therapy in IH, it would be impossible to design a study that included a control group of children with IH not receiving any treatment. VAS score was subjectively assessed by one designated physician in each medical center; therefore, there could be some bias depending on the physician. Additionally, we could not analyze PDGF-BB, TNF-α, IFN-γ, IL-1β, IL-2, or IL-4 because they were either below or above the reference range for each result in the Multiplex Luminex assay; our future study will be specifically designed to address this limitation.
In conclusion, oral propranolol showed a good curative effect in the treatment of IH. Decreases in the concentrations of MMP-2, bFGF, VEGF, and MCP-1 are associated with regression of the hemangioma, which indicates that one of the mechanisms of propranolol in the treatment of proliferative hemangiomas may involve downregulation of those cytokines; however, the exact mechanisms remain to be elucidated. Patients with higher bFGF and VEGF levels showed higher VAS scores at 1 year. Pretreatment bFGF and VEGF could be novel biomarkers for predicting response to propranolol. Importantly, serum bFGF higher than 37.07 pg/mL may predict an excellent response to propranolol. Further studies including MMP-2, bFGF, VEGF, and MCP-1 are needed to determine their role in IH biology and clinical evaluation of these cytokines as potential markers for the individual approach in IH are warranted.
References
Chiller, K. G., Passaro, D. & Frieden, I. J. Hemangiomas of infancy: clinical characteristics, morphologic subtypes, and their relationship to race, ethnicity, and sex. Arch. Dermatol. 138, 1567–1576 (2002).
Tan, S. T., Velickovic, M., Ruger, B. M. & Davis, P. F. Cellular and extracellular markers of hemangioma. Plast. Reconstr. Surg. 10, 529–538 (2000).
Amir, J., Metzker, A., Krikler, R. & Reisner, S. H. Strawberry hemangioma in preterm infants. Pediatr. Dermatol. 3, 331–332 (1986).
Itinteang, T., Withers, A. H., Davis, P. F. & Tan, S. T. Biology of infantile hemangioma. Front. Surg. 1, 38 (2014).
Yun, Y. J. et al. A prospective study to assess the efficacy and safety of oral propranolol as first-line treatment for infantile superficial hemangioma. Korean J. Pediatr. 58, 484–490 (2015).
Chung, S. H. et al. Successful and safe treatment of hemangioma with oral propranolol in a single institution. Korean J. Pediatr. 55, 164–170 (2012).
Zhang, L. et al. Circulating level of vascular endothelial growth factor in differentiating hemangioma from vascular malformation patients. Plast. Reconstr. Surg. 116, 200–204 (2005).
Kleber, C. J. et al. Urinary matrix metalloproteinases-2/9 in healthy infants and haemangioma patients prior to and during propranolol therapy. Eur. J. Pediatr. 171, 941–946 (2012).
Zhong, S., Yang, G., Xia, C., Duanlian, Z. & Shan, S. Expression of matrix metalloproteinase and its tissue inhibitor in haemangioma. J. Huazhong Univ. Sci. Technol. Med. Sci. 29, 614–619 (2009).
Tallant, C., Marrero, A. & Gomis-Ruth, F. X. Matrix metalloproteinases: fold and function of their catalytic domains. Biochim. Biophys. Acta 1803, 20–28 (2010).
Leaute-Labreze, C. et al. Propranolol for severe hemangiomas of infancy. N. Engl. J. Med. 358, 2649–2651 (2008).
Leaute-Labreze, C. et al. A randomized, controlled trial of oral propranolol in infantile hemangioma. N. Engl. J. Med. 372, 735–746 (2015).
Chim, H. et al. Propranolol induces regression of hemangioma cells through HIF-1alpha-mediated inhibition of VEGF-A. Ann. Surg. 256, 146–156 (2012).
Ji, Y. et al. Effects of propranolol on the proliferation and apoptosis of hemangioma-derived endothelial cells. J. Pediatr. Surg. 47, 2216–2223 (2012).
Lamy, S., Lachambre, M. P., Lord-Dufour, S. & Beliveau, R. Propranolol suppresses angiogenesis in vitro: inhibition of proliferation, migration, and differentiation of endothelial cells. Vasc. Pharm. 53, 200–208 (2010).
Zhang, L. et al. Propranolol inhibits angiogenesis via down-regulating the expression of vascular endothelial growth factor in hemangioma derived stem cell. Int J. Clin. Exp. Pathol. 7, 48–55 (2014).
Pan, W. K., Li, P., Guo, Z. T., Huang, Q. & Gao, Y. Propranolol induces regression of hemangioma cells via the down-regulation of the PI3K/Akt/eNOS/VEGF pathway. Pediatr. Blood Cancer 62, 1414–1420 (2015).
Wu, S. et al. Clinical efficacy of propranolol in the treatment of hemangioma and changes in serum VEGF, bFGF and MMP-9. Exp. Ther. Med. 10, 1079–1083 (2015).
Przewratil, P. et al. Serum and tissue profile of VEGF and its receptors VGFR1/R2 in children with infantile hemangiomas on systemic propranolol treatment. Immunol. Lett. 175, 44–49 (2016).
Przewratil, P., Sitkiewicz, A. & Andrzejewska, E. Local serum levels of vascular endothelial growth factor in infantile hemangioma: intriguing mechanism of endothelial growth. Cytokine 49, 141–147 (2010).
Tu, J. B. et al. Induction of apoptosis in infantile hemangioma endothelial cells by propranolol. Exp. Ther. Med. 6, 574–578 (2013).
Kleinman, M. E. et al. Hypoxia-induced mediators of stem/progenitor cell trafficking are increased in children with hemangioma. Arterioscler. Thromb. Vasc. Biol. 27, 2664–2670 (2007).
Zhang, G. Y. et al. Proliferation hemangiomas formation through dual mechanism of vascular endothelial growth factor mediated endothelial progenitor cells proliferation and mobilization through matrix metalloproteinases 9. Med. Hypotheses 70, 815–818 (2008).
Taran, K., Wnek, A., Kobos, J., Andrzejewska, E. & Przewratil, P. Tissue and serum mRNA profile of MMPs-2/9 as a potential novel biomarker for the most individual approach in infantile hemangiomas and cancer disease. Immunobiology 222, 1035–1042 (2017).
Gelmetti, C., Frasin, A. & Restano, L. Innovative therapeutics in pediatric dermatology. Dermatol. Clin. 28, 619–629 (2010).
Tanyildiz, H. G. et al. Serum basic fibroblastic growth factor levels in children with infantile hemangioma. Indian J. Pediatr. 83, 937–940 (2016).
Babiak-Choroszczak, L. et al. Serum concentrations of VEGF and bFGF in the course of propranolol therapy of infantile hemangioma in children: Are we closer to understand the mechanism of action of propranolol on hemangiomas? Adv. Clin. Exp. Med. 27, 703–710 (2018).
Anghelina, M., Krishnan, P., Moldovan, L. & Moldovan, N. I. Monocytes and macrophages form branched cell columns in matrigel: implications for a role in neovascularization. Stem Cells Dev. 13, 665–676 (2004).
Gordillo, G. M., Atalay, M., Roy, S. & Sen, C. K. Hemangioma model for in vivo angiogenesis: inducible oxidative stress and MCP-1 expression in EOMA cells. Methods Enzymol. 352, 422–432 (2002).
D’Arcangelo, D. et al. Identification of serum regression signs in infantile hemangioma. PLoS ONE 9, e88545 (2014).
Acknowledgements
This study was supported by the KACLC Childhood Cancer Research Grant 2016.
Author information
Authors and Affiliations
Contributions
M.P. performed the study, analyzed the data, and wrote the manuscript; H.L.J. designed the study and reviewed the manuscript; Y.J.S., H.S.K., H.S.Y., S.K.P., H.W.C., M.J.L., J.M.L., E.S.P., J.H.L., Y.-J.L. and Y.B.C. contributed to collection of clinical data, patients’ blood sample and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Written informed consents were signed by the guardians of the children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, M., Jung, H.L., Shim, Y.J. et al. Serum cytokine profiles in infants with infantile hemangiomas on oral propranolol treatment: VEGF and bFGF, potential biomarkers predicting clinical outcomes. Pediatr Res 88, 749–755 (2020). https://doi.org/10.1038/s41390-020-0862-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0862-1
This article is cited by
-
Infantile hemangiomas β3-adrenoceptor overexpression is associated with nonresponse to propranolol
Pediatric Research (2022)
-
Propranolol inhibits the angiogenic capacity of hemangioma endothelia via blocking β-adrenoceptor in mast cell
Pediatric Research (2022)