Abstract
Background
Cognitive appraisal of stress can influence performance. Increased awareness could facilitate titration to optimal stress levels. This study’s primary aim was to investigate whether physiologic variables change with increasingly stressful simulations. Secondary aims include effect of stress on procedural competency and whether individuals recognize their experienced stress.
Methods
This was a single-center, mixed-method, simulation-based study. Participants completed three scenarios requiring resuscitation under increasingly stressful conditions. Wearable biometric devices recorded physiologic parameters. Subjects completed surveys assessing knowledge and perceived stress. Intubation success or failure was noted. Heart rate variability (HRV) analysis was used as a proxy for stress.
Results
Twelve participants completed the study. Survey analysis revealed progressive amplification of endorsement of affective states associated with stress. Median low frequency (LF)/high frequency (HF) ratio from scenario 1 (median = 2.29, IQR = 1.97, 3.91) was significantly lower than scenario 2 (median = 4.7, IQR = 2.32, 8.35, p = 0.04) and scenario 3 (median = 4.63, IQR = 2.2, 7.43, p = 0.04). Changes in HRV were noted during all scenarios irrespective of subjective self-assessment of stress. Procedural proficiency suffered during more stressful scenarios.
Conclusions
This study demonstrates alterations in subjective assessment and objective physiologic data in simulations with increasing stress. HRV is useful as a proxy for stress response and does not always correlate with perception.
Similar content being viewed by others
Introduction
Stress can be a tool, or stress can be a toxin. Harnessed for good, the improved physical and mental prowess associated with stress can aid in performance. Misdirected, the physical and mental effects of distress can cripple proficiency. Modern individuals are under pressure to perform optimally in most aspects of their lives. The stakes for performing to the best of one’s abilities are high,1 especially in fields where decisions change lives, like the military or medicine. While investigations of human responses to stress have been ongoing since the term “fight-or-flight” was first coined in the late 1920s2,3 and a discussion of the general adaptation syndrome—alarm, resistance, exhaustion—was elucidated in the 1950s,4 the search continues for ways of maximizing positive performance under stressful mental and physical conditions. Stress was introduced as a concept in the context of adaptation or maladaptation to situations, with a focus on nonspecific features of acute and chronic disease.5 One framework differentiates “stressors,” physical or psychological experiences which may serve as potential obstacles to major goals, and “distress,” a state that results from individual interpretation of stressors leading to states like bewilderment.6
Little is published about how physicians qualitatively and quantitatively experience, differentiate, and manage aspects of stress. Cognitive appraisal is inextricable from individual stress/distress response.7 Different people can respond to the same stimulus in different ways and the same person can respond to the same stimulus in different ways at different times.8 Appraisal of a situation is enough to change the condition itself9 and the quality of, though not necessarily the degree of, autonomic nervous system (ANS) response.6 When a person encounters a stressful experience, what determines her approach is the juxtaposition of the stressor’s inherent characteristics with individual traits like personality, coping style, memories, and relationships.6,8 While little can be done to modify the intensity of real-life resuscitations with requisite technical skills and interpersonal interactions in critical care settings, training can prepare for these inevitabilities.10 Adding stressors related to the overarching educational goal in the context of training helps to cement these skills.11
Medical simulation represents an emerging modality for investigating associated stress encountered during clinical situations. Expert consensus suggests that procedural proficiency should be achieved in a simulated environment prior to attempts on patients12; however, aspects of the simulation environment may be inherently unrealistic. In addition, individuals participating in simulation may be unaware of the distress they experience. Analysis of heart rate variability (HRV) provides a window into competing mechanisms regulating an individual’s heart rate (HR). Branches of the ANS (parasympathetic and sympathetic), baroreceptors, chemoreceptors, and inherent respiratory sinus arrhythmia all play into HRV, which has been a marker of an individual’s health.13 Wearable technology is one way researchers are able to obtain this physiologic data for analysis.
After a comprehensive review of the literature, we believe that this is the first study to integrate subjective and objective measures of stress in simulated neonatal scenarios. Our primary aim was to evaluate whether individuals participating in a series of increasingly stressful simulation-based scenarios would exhibit alterations in physiologic variables like HR and HRV. We hypothesized that individuals exhibiting evidence of progressive distress may perform less well procedurally during neonatal resuscitations. We additionally postulated that individuals were likely unaware of the full extent of the stress they experienced during simulation.
Methods
Study design
This was a single-center, mixed-method, simulation-based study. It was approved by Yale’s Human Investigation Committee prior to recruitment.
Setting
The study took place at a simulation center affiliated with a large U.S. academic medical institution (Yale School of Medicine) between March 2018 and June 2018.
Participants
Study participants were Yale-New Haven Hospital Emergency Medicine (EM) resident physicians in their first and second postgraduate years. Following informed consent, each participant was assigned a study identification number accessible only to one person with no clinical or supervisory relationship to any participant.
Variables, data source, and measurement
EM resident physicians were invited to participate in a neonatal airway training day, which included a series of three simulated scenarios related to neonatal management and resuscitation. Participants were individually fitted with a wearable biometric device, a HexoskinTM smart shirt (Carre Technologies Inc, Montreal, Canada), which was used to collect continuous physiologic data from the time period immediately prior to filling out the first survey to after the final debriefing in the study. HexoskinTM was chosen because it provided continuous electrocardiogram (ECG) cardiac monitoring over time necessary for HRV analysis, the technology was presumed to be acceptable to study participants, and accuracy had been validated in previous studies.14,15,16,17 Because participants wore a biometric device throughout the time they were engaged in the study, baseline HR data specific to individuals was obtained, allowing each person to be used as their own control. This factor enabled individual and interparticipant HRV analysis, critical for achieving statistical significance with a smaller number of study participants.
Participants spent approximately 3 h completing the study. An initial assessment contained questions on demographics (Supplementary Material), general state-of-being (i.e., anxious, excited, etc.), pre-test knowledge, and derivative questions from the Perceived Stress Scale (PSS)18 and the Positive and Negative Affect Schedule (PANAS).19 Other questions addressed sleep, exercise, diet, work schedule, major life events, and medications. Each resident viewed an instructional video on neonatal intubation at the start of the study.20
Following each simulation, a brief, real-time, post-scenario survey was completed via Yale Qualtrics, a secure, web-based data collection and survey tool. Responses were given on a Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree). Questions were derived from the PSS18 and included whether the participant felt nervous/scared/stressed, whether they felt that their stress response negatively impacted performance, whether the participant felt in control, whether the participant felt things were going his or her way, and whether the participant objectively felt they had successfully managed the case and completed the intubation. Additional questions from the PANAS asked individuals to rate on a Likert scale whether they experienced a variety of affective states (e.g., ashamed, excited, distressed, interested, hostile, scared, etc.)19 after completing a scenario.
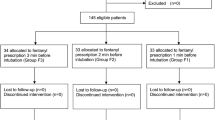
Next, subjects participated in a structured debriefing, with facilitators utilizing TeamGAINS21 framework. After the final scenario and completion of the real-time post-scenario survey, one additional survey was administered to reassess knowledge, state, and stress, similar to those on the initial survey. Figure 1 depicts an individual’s work flow during the study.
Participant orientation
Participants were oriented to the standardized simulation environment in the Yale Center for Medical Simulation at the Yale University School of Medicine. In addition to discussing the ground rules of simulation and providing specific information about the layout of the room and the equipment, individuals were also given time to become comfortable with the low- and high-fidelity infant mannequins (Newborn AnneTM and SimNewB®, Laerdal Medical, Stavanger, Norway).
Simulation environment
The room included an infant warmer, printed Neonatal Resuscitation Program (NRP) algorithm, blankets, bulb and wall suction, an infant bag valve mask for positive pressure ventilation, laryngoscope with Miller 00, 0, 1 blades and MacIntosh 00, 0, 1 blades, cuffed and uncuffed endotracheal tubes (2.5–4.0), ETT stylets, a Broselow Pediatric Emergency Tape (Armstrong Medical Industries Inc, Lincolnshire, IL), Pediatric Advanced Life Support (PALS) card, medications, intravenous (IV) supplies, and an umbilical venous catheter tray with all of the tools and equipment necessary for emergent umbilical venous catheter placement. A videolaryngoscope (Storz C-MAC Karl Storz Endoscopy, Berkshire, UK) was used instead of direct laryngoscopy, allowing the facilitator to assess the success or failure of intubation in real time.
Simulation scenario
Three simulated scenarios with increasing stress levels (Table 1) were created for this study. Each scenario required successful intubation and implementation of neonatal resuscitative efforts per the NRP algorithm. Authors with expertise in neonatology initially drafted the low-, medium-, and high-stress scenarios. Feedback was elicited from five additional faculty and trainees in neonatology and EM to ensure that the content was appropriate and that the targeted stress level was achieved. At the beginning of each case, the facilitator read a script with the background information for the case. A standardized confederate (acting as either a bedside nurse or family member) was present.
Instructional design
Individual simulations (detailed in Table 1) were predetermined to last no longer than 15 min. If a case did not come to a natural conclusion with completion of the stated goals, the facilitator was instructed to end simulation after the allotted time. The scenarios were videotaped from two angles using SimCapture (B-Line Medical, Washington, DC), and intubation attempts with airway view were recorded via memory card in the C-MAC. Video footage was linked to unique participant number. Special attention was given to the airway view obtained by the participant, the timing of intubation, and the success or failure of the procedure. Other key time points, including specific actions taken by the participant (e.g., talking directly to family member or taking over chest compressions) and directions given (e.g., requesting IV placement) during the cases were also recorded.
Statistical analysis
Self-reported outcomes
For the comparison of self-reported outcomes measured on the Likert scale, we estimated that a sample size of 12 would achieve 84–97% power at an alpha of 0.05, using a two-sided Wilcoxon Signed-Rank test, to detect a mean of paired differences of 1.0 with an estimated standard deviation of differences of 0.8 for the within-person correlation ranging from 0.15 to 0.5. We did not adjust for multiple comparisons due to the multiple questions that elucidated stress level, for example, because we believe that the individual questions tapped into different domains of stress and, as such, form different testable hypotheses.
Responses to individual questions were summarized using means (with SD). The pretest and posttest answers about knowledge, as well differences among the three real-time post-scenario survey responses, were compared using Wilcoxon Signed-Rank test. Significant results (p < 0.05) were summarized using bar graphs. Data were analyzed using SAS 9.4 (Cary, NC).
Physiological outcomes
Analysis of physiological data focused on differences in HR and HRV among the three simulation scenarios. Changes in HR alone are interesting but insufficient for identifying influences of stress.22 The branches of the ANS vie for instantaneous cardiovascular control, and HRV analysis helps elucidate which branch dominates over time. Owing to the difference in time it takes for sympathetic and parasympathetic activities to affect HR, HRV frequency domain analysis was conducted. HRV summary outcomes were obtained at very low frequency (<0.03 Hertz), low frequency (LF: 0.03–0.15 Hz), and high frequency (HF: 0.15–0.4 Hz). The parasympathetic system is somewhat faster than the sympathetic system, and as a result, when reviewing data peaks in the medium frequency and HF range, it has almost exclusive control. LF peaks can represent involvement from either system.20 There were no time periods in the data with >30 s of missing data points, making noninterpolated HR useable. An example of noninterpolated instantaneous HR trajectory, as well as power bands of HRV at different frequencies and LF/HF ratio, is presented visually for one subject using a time-series plot (Figs. 2 and 3).
Wavelet analysis was selected over Fourier transform for power band analysis due to the short periods of time analyzed. Wavelet “d4” of the external phase Daubaechies was selected for improved temporal discrimination.20 The analysis was completed in the R-HRV package23 (v4.2.3) in R (v3.4.2).24 The LF/HF ratio was chosen because it is considered a measure of sympathetic system dominance, which can be extrapolated to an individual’s physiologic response to stress. The LF/HF ratios were compared between scenarios using Wilcoxon Signed-Rank test. Between-subject variability in the LF/HF ratios across the three scenarios was summarized using an intra-class correlation. Spearman correlation (ρ) was used to examine the association between one of the self-reported markers of stress (from the following real-time post-scenario survey question: “I felt nervous, scared, or stressed”) and the LF/HF ratio estimated from each scenario.
For all analyses, statistical significance was established at alpha = 0.05, but association was also noted when alpha = 0.1.
Results
Fourteen of the 30 eligible residents (15 residents per postgraduate year) were approached for participation, 14 participants consented to participate, and 12 were able to complete the study. Two participants dropped out of the study because of scheduling conflicts. Of the 12 participants in the study, all had experience with intubation in older children or adults either in simulation or in clinical contexts, but few had prior simulation-based or clinical exposure to neonatal intubation and resuscitation. All but one had exposure to video laryngoscopy [GlideScope Video Laryngoscope (Verathon, Bothell, WA, USA)] but none had used a C-MAC prior to the study day. Only one participant had completed training through the American Academy of Pediatrics NRP, although 80% had been certified in PALS allowing for a homogenous neonatal resuscitation experience level. Half of individuals were on a clinical service block, with the remainder on elective.
More than half of the participants (7/12) reported a major life stressor within the last year, including but not limited to the birth of a child, marriage, or divorce; death of a close friend or family member; or recent move. The majority of subjects slept an average of 5–7 h per night. Two participants said they never exercised, and the rest reported 15–30 min daily. Two-thirds of respondents described their diet as “unhealthy” or inconsistent, although qualifying descriptions varied. Most subjects denied the use of prescription medications, although one was on Celexa and another on Wellbutrin. No participants reported taking benzodiazepines or beta blockers. The survey did not ask about caffeine, illicit drugs, marijuana, tobacco in any form, or alcohol, although all participants were subject to drug testing as a condition of their employment through Yale-New Haven Hospital.
Self-report survey results
Analysis demonstrated significant self-report of stress with progression through each of the scenarios (Fig. 4). This was particularly true for the comparison of the first to the third scenario, with participants reporting increased subjective stress across multiple questions. For example, more participants strongly agreed with the statement “During the simulated resuscitation I felt nervous, scared, or ‘stressed’” as the study day progressed; and fewer subjects agreed with the statement, “During the simulated resuscitation, I felt things were going my way”, as they moved from the first simulation to the last.
There was an increase in the affect expressions (PANAS) in individuals endorsing the following states from scenario 1 to scenario 3: distressed (p = 0.05), hostile (p = 0.02), and determined (p = 0.03). “Attentive” approached but did not cross the threshold of statistical significance.
Analysis of pretest and posttest data showed significant increase in knowledge about the timing, equipment, and mechanics of intubation in addition to appropriate interventions required for successful neonatal resuscitation (data not shown). After participation in the study, all participants were able to correctly identify the appropriate-size Miller blade to use for intubating a term neonate (Miller 1), and the correct amount of time it should take to complete the procedure (30 s).25 On the posttest, all respondents successfully identified airway anatomy, and they selected the correct view that proper use of the laryngoscope should produce.
Simulation facilitators noted two participants, one during the second scenario and one during the third, were unable to successfully intubate the mannequin on the first or subsequent attempts (i.e., an endotracheal tube was placed in the esophagus). This was confirmed on video laryngoscopy footage. Another participant was reticent to pronounce the infant dead in the final scenario, and the facilitator needed to end simulation after the predetermined time had elapsed.
Physiologic data analysis
Among participants as a group, the LF/HF ratio from scenario 1 (median = 2.29, interquartile range (IQR) = 1.97, 3.91) was significantly lower than from scenario 2 (median = 4.7, IQR = 2.32, 8.35, p = 0.04) and from scenario 3 (median = 4.63, IQR = 2.2, 7.43, p = 0.04). The difference between scenarios 2 and 3 was not significant (p = 0.83). We also observed significant between-person variability in the magnitude of HRV as a response variable, so that, while there was an average increase in the LF/HF ratio across the three scenarios, individual subjects tended to generate on average higher or lower values across all scenarios. There was no significant association between participants’ self-report on how they felt during a scenario and their LF/HF ratio (scenario 1: ρ = −0.12, p = 0.71; scenario 2: ρ = 0.39, p = 0.21; scenario 3: ρ = −0.05, p = 0.87).
Discussion
This study demonstrates an association between participation in increasingly stressful simulation scenarios and changes in physiologic variables consistent with a stress response. This is a novel finding, as other groups26 working with similar biometric devices within simulation have not shown significant physiologic disruption. Sometimes physicians were aware of their response to significant stressors, but in other instances, they seemed to lack insight into the effects of stress. Participants’ self-efficacy, measured by reported confidence in their ability to successfully intubate a term baby, improved following participation in the study. Self-report about stress specific to intubation and resuscitation showed individuals perceived increased stress during the latter cases, which were developed to include increasing stressors. This provides further support for titrating stress in simulation training over time so as to prepare the participant for increasing stress in the clinical environment. Because some participants experienced the most distress in the third scenario, this study lends support for the critical nature of addressing infant death in simulation given its prevalence in clinical contexts.27,28 Furthermore, because some participants had difficulty performing intubation while experiencing distress, titrating stress in simulation may be helpful in optimizing technical performance.
We found an increase in LF/HF ratio across scenarios, as well as significant between-subject variability in the ratio. Across all scenarios, some subjects responded to the scenarios on average with higher ratio values, and other subjects responded on average with lower ratio values. Change from scenario to scenario was seen in all subjects. We found large between-person variability in the magnitude of HRV, but the scale of the self-reported questions related to stress was limited to 1–5 on the Likert scale. The allowable range of LF/HF ratios was inherently broad, whereas the range of responses to survey questions was constrained by the scale. Had we expanded the self-reported scales to include a broader range, there may have been greater variability in the responses to the self-reported stress-related questions, and an association between subjective and objective measures of stress might have been detected.
Previous authors have demonstrated an increase in subjective stress related to simulation29 and observation.30 The change in magnitude of the stress response in each scenario, especially from the first to the second, sets this study apart from prior investigations. The degree of stress participants experienced is likely multifactorial and potentially related to participation in simulation, observation of performance, lack of familiarity with subject matter, and embedded stressors in the cases, in addition to other individualized sources of stress. Neonatal resuscitation and stress are inextricably linked; as such, ensuring that participants experience stress during training is likely beneficial, but only up to a point. For some participants, the stress response exhibited may indicate that capacity for long-term skill acquisition is impaired because distress may undermine learning.11
Significant variability existed with respect to whether individual participants felt their performance suffered as a result of stress, including inconsistencies between self-reported confidence in procedural performance and objective evaluation by the facilitator. For example, one participant was confident they had intubated the mannequin, but the facilitator confirmed placement of the endotracheal tube in the esophagus. Because participants were oriented to the equipment and the mannequin, with time to make clarifications prior to beginning the scenarios, it seems unlikely that this failure of airway management is related to lack of understanding of the appropriate view and therefore is potentially attributable to participant stress.
Procedural training and education may overcome gaps related to performance.11,31 Aspects of performance cemented in long-term motor memory are no longer subject to forces that can act on working memory and, as such, are more likely to be preserved even in highly stressful contexts. Mental training through visualization can reinforce procedural capability and facilitate strengthening of motor memory.32 Decreasing cognitive load in stressful situations can be achieved through outsourcing knowledge that needs to be readily available in working memory (i.e., use of cognitive aids) and may reduce stress.25 Individuals can learn to modify physiologic manifestations of stress via teachable tools,33 which could lead to better outcomes clinically.
Potential interventions for stress management include education—both about the topic causing distress and the stress itself. If a stressor is viewed as a threat, in which demands seem disproportionately high relative to resources, a situation can lead to activation of the sympathetic nervous system (SNS), resulting in increased cardiac output, increased peripheral resistance, and increased blood pressure. If the same situation were viewed as a challenge, in which resources match or exceed perceived demands, SNS is activated with increased HR, but without alteration in blood pressure, similar to the body’s response to aerobic exercise.6
Biofeedback, in which an individual seeks awareness of and modification to aspects of the nervous system usually unconsciously controlled by the brainstem, like respiratory rate and HR, enables individuals to use techniques to interrupt neural pathways potentiating different arms of the ANS. The spectrum of techniques considered biofeedback ranges from monastic mastery of body temperature and blood pressure34 to simple strategies35 such as taking long measured breaths during busy or stressful situations. Intentional pauses or short breaks, positive self-talk, and other reframing techniques are also effective in reducing distress.36 Cultivating mindfulness and consciously practicing techniques that enhance resilience are invaluable in buffering the toxic effects of stress, given the potential negative effects on performance as well as long-term health consequences.37
Limitations
The most significant limitation of this study is its small sample size. Given the nature of the study, time spent in preparation, execution, and analysis of multiple data sets was extensive. Individual clinical schedules prevented all eligible and interested parties from participating, and two of the participants were unable to complete all three scenarios due to clinical or personal commitments. An additional limitation is the presence of incomplete data due to technologic malfunction and time limitations for three individuals, but these aspects were controlled for in statistical analysis. Short gaps in ECG data likely resulted from brief periods of lost sensor contact with an individual’s skin. Body habitus and inherent characteristics (e.g., whether an individual is more likely to perspire) impacted electrode contact, although the data contained embedded quality and reliability information.
There are limitations in surveys relying on self-report, as some participants may be more aware of their objective performance, or influenced by their emotions, than others. State-of-being questions are particularly vulnerable to interpretation. Given the potential to subtly and overtly alter physiologic parameters, not asking about caffeine and drug use was a missed opportunity. One expects tolerance from chronic caffeine consumers such that their data should still reflect acute responses to conditions, but not having any information about other drug use may have been a confounder.
While a five-point Likert scale was utilized in the study, in large part because the sources from which the questions were derived utilized a scale from 1 to 5, we unintentionally limited the nuances of the subjective stress report. This may explain the lack of association between objective measurement of stress and the self-reported scales. If the self-report Likert scales had been expanded to be 1–10, greater variability in the responses might have allowed an association to be detected. Specifically, the inability to detect subtleties in degrees of stress between scenarios 2 and 3 may have resulted from this study design decision, and it would be interesting to repeat the assessment with expanded scales.
Future work
One way to counteract some of the findings above would be to recruit individuals to undergo a series of stressful simulations with similar subjective and objective measures but to incorporate interventions known to change the ANS output, with a goal of assessing whether decreased markers of distress were observed. Additional work is needed to investigate the applicability of understanding an individual’s level of distress during simulation and whether modifying scenarios in real-time improves learning.
Translating these findings into the clinical realm may assist in expanding understanding of how physicians respond internally to neonatal resuscitations and assessing subjective and objective measures of stress surrounding those events. Such work could potentially generate a body of knowledge directly related to physician health, stress management, and long-term consequences of repeated exposure, including vulnerability to burn-out, as well as cultivation of resilience.
Conclusion
Changes in physiologic responses, such as HRV, can be utilized as a proxy for stress response. In this study, participants were noted to have alterations in these parameters when participating in simulation-based training sessions of increasing levels of stress. Awareness of how the ANS responds, reappraisal of threats into challenges, and proportional countermeasures for distress could prove invaluable to improving performance and decreasing the impact of long-standing stress on healthcare providers.
References
Mitchell, M. S., Greenbaum, R. L., Vogel, R. M., Mawritz, M. B. & Keating, D. J. Can you handle the pressure? The effect of performance pressure on stress appraisals, self-regulation, and behavior. Acad. Manag. J. 62, 531–552 (2019).
Angell, J. R. Bodily changes in pain, hunger, fear and rage; an account of recent researches into the function of emotional excitement. Science 42, 696–700 (2006).
Cannon, W. B. Bodily Changes in Pain, Hunger, Fear and Rage. An Account of Recent Researches into the Function of Emotional Excitement (D Appleton and Company, New York, London, 1929).
Selye, H. The Physiology and Pathology of Exposure to Stress (Acta Endoerinologica Inc., Montreal, 1950).
Selye, H. The evolution of the stress concept. Am. Sci. 61, 692–699 (1973).
Kemeny, M. E. The psychobiology of stress. Curr. Directions Psychol. Sci. 12, 124–129 (2003).
Lazarus, R. S. & Alfert, E. Short-circuiting of threat by experimentally altering cognitive appraisal. J. Abnorm. Soc. Psychol. 69, 195–205 (1964).
Teigen, K. H. Yerkes-Dodson: a law for all seasons. Theory Psychol. 4, 525–547 (1994).
Tomaka, J., Kibler, J., Blascovich, J. & Ernst, J. M. Cognitive and physiological antecedents of threat and challenge appraisal. J. Personal. Soc. Psychol. 73, 63–72 (1997).
Georgiou, K., Larentzakis, A. & Papavassiliou, A. Surgeons’ and surgical trainees’ acute stress in real operations or simulation: a systematic review. Surgeon 15, 355–365 (2017).
Leblanc, V. R. The effects of stress on performance: implications for health professions education. Acad. Med. 84, S25–S33 (2009).
Sawyer, T. et al. Improving neonatal intubation safety: a journey of a thousand miles. J. Neonatal Perinat. Med. 10, 125–131 (2017).
Iwase, S., Hayano, J. & Orimo, S. Clinical Assessment of the Autonomic Nervous System (Springer Japan, 2016).
Abdellah, S. J. et al. Validation of hexoskin biometric technology to monitor ventilatory responses at rest and during exercise in COPD. Eur. Respir. J. 50, PA1359 (2017).
Al Sayed, C. et al. Validation of a wearable biometric system’s ability to monitor heart rate in two different climates under variable physical activities. E-Health Telecommun. Syst. Netw. 6, 19–30 (2017).
Bläsing, D. et al. Effect of cardiac coherence training on real-life stressors. In 63rd Spring Congress of the Society for Ergonomics at the University of Applied Psychology (Society for Ergonomics, 2017).
Cherif, N. H. et al. Physiological data validation of the Hexoskin smart textile. In Proc. 11th International Joint Conference on Biomedical Engineering Systems and Technologies, BIOSTEC 2018 - Vol. 1 150–156 (Biodevices, 2018).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396 (1983).
Watson, D., Clark, L. A. & Tellegen, A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol. 54, 1063–1070 (1988).
OPENPediatrics. Neonatal tracheal intubation. https://www.openpediatrics.org/assets/video/neonatal-tracheal-intubation (2016).
Kolbe, M. et al. TeamGAINS: a tool for structured debriefings for simulation-based team trainings. Br. Med. J. Qual. Saf. 22, 541–553 (2013).
García Martínez, C. A. et al. Heart Rate Variability Analysis with the R Package RHRV. (Springer International Publishing, Basel, 2017).
Leandro, R.-L., et al. RHRV: heart rate variability analysis of ECG data. R package version 4.2.3. https://CRAN.R-project.org/package=RHRV (2017).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, 2017).
American Academy of Pediatrics, American Heart Association. Textbook of Neonatal Resuscitation, 7th edition (American Heart Association, Dallas, TX, 2016).
Parker, R. A Prospective Study Investigating Measurement of Biometric Parameters of Critical Care Practitioners during Simulation Events using the Wearable Performance Tracking Device known as Hexoskin™. INSPIRE Annual Report 2017–2018 (Pediatric Critical Care, DuPont Children’s Hospital, 2020). Manuscript in process.
Lizotte, M.-H. et al. The impact of neonatal simulations on trainees’ stress and performance. Pediatr. Crit. Care Med. 18, 434–441 (2017).
Hollingsworth, C. et al. Impact of child death on pediatric trainees. Arch. Dis. Child. 103, 14–18 (2018).
Bong, C. L., Lightdale, J. R., Fredette, M. E. & Weinstock, P. Effects of simulation versus traditional tutorial-based training on physiologic stress levels among clinicians: a pilot study. Simul. Healthc. 5, 272–278 (2010).
Bensouda, B. et al. Effect of an audience on trainee stress and performance during simulated neonatal intubation: a randomized crossover trial. BMC Med. Educ. 18, 230 (2018).
Goldberg, M. B. et al. Optimizing performance through stress training—an educational strategy for surgical residents. Am. J. Surg. 216, 618–623 (2018).
Rao, A., Tait, I. & Alijani, A. Systematic review and meta-analysis of the role of mental training in the acquisition of technical skills in surgery. Am. J. Surg. 210, 545–553 (2015).
Meichenbaum, D. & Deffenbacher, J. Stress inoculation training. Counseling Psychologist 16, 69–90 (1988).
Benson, H., Beary, J. F. & Carol, M. P. The relaxation response. Psychiatry 37, 37–46 (1974).
Varvogli, L. & Darviri, C. Stress management techniques: evidence-based procedures that reduce stress and promote health. Health Sci. J. 5, 74–89 (2011).
Anton, N. E., Montero, P. N., Howley, L. D., Brown, C. & Stefanidis, D. What stress coping strategies are surgeons relying upon during surgery? Am. J. Surg. 210, 846–851 (2015).
Stanford University, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) & Duke University. ClinicalTrials.gov. identifier NCT02603133. Web-based implementation for the science of enhancing resilience study (WISER). https://clinicaltrials.gov/ct2/show/NCT02603133 (2015).
Acknowledgements
We thank Joy Grabow, Luis Cruz, Jeffrey Hoffman, and Dr. Ambika Bhatnagar, MD for their support as staff in the simulation center.
Author information
Authors and Affiliations
Contributions
B.R. and I.T.G. conceptualized the article and drafted the initial manuscript. B.R., I.T.G., M.J., J.R., C.B., V.S., J.M., M.A., and L.J. participated in project planning process, data collection, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Redmond, B., Joseph, M., Ray, J. et al. Stress as tool or toxin: physiologic markers and subjective report in neonatal simulation. Pediatr Res 88, 784–791 (2020). https://doi.org/10.1038/s41390-020-0806-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0806-9