Abstract
Background
Staphylococcus aureus is the leading cause of skin and soft tissue infections (SSTIs). To develop interventions to prevent recurrent infections, household attributes and individual practices influencing S. aureus colonization must be discerned.
Methods
Households of healthy children with methicillin-resistant S. aureus (MRSA) SSTI (n = 150; 671 participants) were interviewed regarding health history, activities, and hygiene practices. S. aureus colonization was assessed in household members, and recovered isolates were typed by repetitive sequence-based PCR.
Results
The number of unique strain types in a household (median 1, range 0–7) correlated with the number of colonized individuals (p < 0.001). The MRSA infecting strain type colonized a household member in 57% of 91 households with an available infecting strain, and was the most common strain type recovered in 45% of these households. In multivariable models, household MRSA colonization burden (p < 0.001), sharing a bedroom with MRSA-colonized individuals (p = 0.03), renting dwelling (p = 0.048), and warmer seasons (p = 0.02) were associated with increased MRSA colonization. Increasing age (p = 0.02), bathing at least daily (p = 0.01), and antibacterial soap use (p = 0.03) correlated with reduced MRSA colonization.
Conclusions
This study identified practices that correlate with MRSA colonization, which will inform physician counseling and multifaceted interventions among MRSA-affected households to mitigate MRSA in the community.
Similar content being viewed by others
Introduction
Staphylococcus aureus poses a threat to the health of individuals in the community and those requiring hospitalization. Methicillin-resistant S. aureus (MRSA), and particularly the USA300 clone, has become the predominant etiology of skin and soft tissue infections (SSTIs) in the United States.1,2,3,4,5 The high incidence of recurrent skin infections,6 as well as increasing antibiotic resistance,7 demands novel strategies to curtail the epidemic.
Asymptomatic human carriage is a critical reservoir for S. aureus infection.4,8,9 Overall, half of all individuals are colonized at least intermittently with S. aureus.10,11,12 Multiple members of the same household frequently experience MRSA infections, and a high proportion of household contacts of patients with MRSA infection are colonized.13,14,15,16 Measures to reduce the incidence of MRSA colonization and recurrent SSTI in these households, including decolonization strategies (i.e., “the use of antimicrobial or antiseptic agents to suppress or eliminate S. aureus carriage”17 such as mupirocin topical antibiotic or body washes with chlorhexidine or dilute bleach water), have yielded modest success.6,18 To date, factors associated with MRSA SSTI and colonization have included prior skin infections, antibiotic history, and the burden of colonization among household members.13,15,16,19,20 However, these studies were limited by examining a subset of household members, discounting hygiene practices and proximity to other household members, or incomplete molecular resolution of the strains in each household, especially the presence and distribution of the strain responsible for the initial SSTI.
In the present study, we measured S. aureus colonization in 150 households of children (index patients) presenting with MRSA infection. We observed how the household distribution of S. aureus, household demographics, health history, and individual hygiene practices influence overall S. aureus and MRSA colonization. Through molecular typing of available infecting isolates from the initial SSTI and all colonizing isolates collected from index patients and their household contacts, we determined the prevalence of carriage of infecting strains compared to other colonizing strains as well as strain concordance across household members. We sought to identify practices that correlate with colonization with S. aureus in general, and MRSA specifically (especially the infecting strain within households), to inform clinical practice guidelines and ultimately to mitigate the incidence of S. aureus infections in the community.
Methods
Participants
Index patients with a community-associated (CA)-MRSA infection (149 SSTI, 1 bacteremia/myositis/septic pulmonary emboli) were recruited from pediatric practices affiliated with the Washington University Pediatric and Adolescent Ambulatory Research Consortium, St. Louis Children’s Hospital, and Cardinal Glennon Children’s Hospital. Exclusion criteria included healthcare-associated infection, inability to confirm MRSA culture from SSTI, duration of >100 days from infection to enrollment, and home distance >80 miles from medical center. Of 247 eligible patients, 150 index patients and their household contacts (individuals sleeping at the household ≥4 nights/week) were enrolled in the HOME: Household Observation of MRSA in the Environment study. Enrollment visits were conducted between January 2012 and October 2015 within 20 days (median; range 3–95) of acute infection. The Washington University Human Research Protection Office approved study methods and written, informed consent was obtained for each participant.
Data collection
At enrollment, the research team visited participants’ homes to conduct an interview and assess the colonization status of household members. The interview consisted of questions concerning health history, S. aureus and other skin infection history, demographics, activities outside of the house, personal and environmental hygiene practices, daily proximity to other household members, and sharing of personal hygiene items. Study personnel assigned each home a cleanliness score accounting for odor, clutter, and grime, ranging from 1 to 4 (above average, average, below average, very dirty), modified from the established Environmental Cleanliness and Clutter Scale21 to account for participant bias. To measure S. aureus colonization, swabs (Eswab, Becton Dickinson, Franklin Lakes, NJ) were collected6 from the anterior nares, axillae, and inguinal folds of all household members.
Microbiological methods
S. aureus was detected using broth-enrichment culture-based methods; identification and antibiotic susceptibility testing were conducted in accordance with established techniques.22,23 All S. aureus colonizing isolates (n = 389) and the index patients’ MRSA infection isolates prompting enrollment (n = 150) were subjected to antibiotic susceptibility testing. Ninety-one infection isolates were available for molecular typing. Thus, 480 isolates were subjected to staphylococcal cassette chromosome mec (SCCmec) typing using multiplex PCR.24 Strain-level uniqueness was assessed through repetitive sequence-based PCR (repPCR).25,26 Strain relatedness was assigned within each household; strains with ≥95% similarity were considered identical (Supplementary Figure S1).
Statistical summaries
Colonization proportions across individuals and households were compared using Fisher’s exact test in R.27 The number of unique strains between observed groups (e.g., frequent vs. infrequent bathers) was calculated with the nonparametric Mann–Whitney U and median Kruskal–Wallis tests for two and more than two groups, respectively. Correlation between variables was quantified via Spearman’s ⍴ in R. For univariate analyses, categorical and continuous covariates were tested for significance through Fisher’s exact test and Kruskal–Wallis one-way ANOVA, respectively. Multiple test correction was performed using the Bonferroni method. Figures were developed through Python using the package ‘Seaborn’.28
Anatomical site colonization pressure (ACP) within each household was calculated via the following, adapted from:20
Three anatomical sites were sampled per individual (axillae, nares, and inguinal folds). Household strain richness was also measured as the number of unique strain types by repPCR present among all household members across these sites. In cases where ACP or household strain richness were considered in individual colonization models (i.e., models evaluating factors associated with personal colonization), colonization data for the individual being modeled was excluded from calculations.
Models to identify factors associated with colonization, strain concordance, and infecting strain prevalence
To explore factors associated with various colonization phenotypes, the following multivariable models were constructed: “Colonization Pressure” to define the burden of S. aureus in households, “Colonization Proximity” to determine how relative proximity to colonized individuals modulates colonization risk, “Colonization Activity” to understand how hygiene behaviors influence colonization, “Colonization Concordance” to observe how proximity leads to pairs of individuals sharing a specific S. aureus strain, and “Infecting Strain Prevalence’ to measure which factors led to the prevalence of the strain isolated from the index patient’s infection prompting study enrollment (infecting strain). All colonization models were constructed as generalized linear regression models and fit using the R libraries “lme4” and “MCMCglmm.” See Supplementary Methods for detailed descriptions of each colonization model, model selection, and model references. See Supplementary Tables S1-S4 for the specific list of covariates used in model selection for each model type. See Supplementary R Code for Model Selection and Parameter Estimation for further details.
Household-level preventability measures the extent to which colonization patterns can be attributed to individuals living in the same household, and accordingly indicates how altering individual vs. household behaviors may modify S. aureus colonization. Household-level preventability (p2H) was estimated as the fraction of total variance in the model explained by the household-level random effect from the models fitted in ‘MCMCglmm’:29
where VH represents the household-level variance estimate and VT the total measured variation. A household preventability of 90%, for example, indicates that interventions targeting household-level behaviors, such as frequency of washing bedding or towels, may be more effective than interventions targeted to specific individuals, such as hand washing or bathing frequency.
Results
Participant demographics
A cohort of 150 pediatric patients (median age 3.0 years, range 0.1–18.6) with an MRSA infection from 150 distinct households and their household contacts (n = 521, ranging from 1 to 12 contacts per household; median age 26.6 years, range 0.1–82.2) were enrolled. Index patients were primarily Caucasian (102, 68%) and African American (37, 25%). The groin/buttock was the most common site of enrollment infection (69, 46%). Notably, 33% (49) of index patients had eczema, and 58% (87) reported an SSTI in the year prior to the enrollment SSTI. Median household size was four (range 2–13) (Table 1).
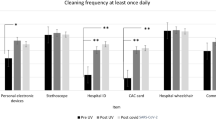
Hygiene practices and physical activities
Index patients and household contacts were administered a comprehensive survey regarding personal hygiene, laundering practices, and activities inside and outside of the home (Table 1). Many (58%) individuals engaged in bathing daily, while the remainder (42%) reported bathing at least 3-4 times per week; 3 reported bathing less than once per week. Nearly half of the participants (40%) reported washing their bedding weekly or more, while 22% washed bedding once a month or less. Most participants (63%) reported reusing bath towels before laundering them; 18% used their towel ≥5 times between washings. While towels were most often washed in hot (56%) or warm (29%) water, participants less often reported washing underwear, undershirts, pants, and outer shirts with hot water (26%, 24%, 16%, and 16%, respectively). On a 4-point cleanliness scale, interviewers found that 27% of households were very dirty or below average, 45% were average cleanliness, and 27% were rated above average.
Activities outside of the home included exercising at a gym (20%), sports participation (29%; 4% in a contact sport such as football, lacrosse, or wrestling), and public pool attendance (36%) (Table 1, Supplementary Table S5). Over half (57%, 124/218) of children 6 years of age or younger were enrolled in daycare; 48% (72/149) of index patients attended daycare.
Colonization overview
Of 671 participants, 275 (41%) were colonized with S. aureus at one or more body site(s) (24% specifically with MRSA, Table 1). Index patients were equally likely as household contacts to be colonized with S. aureus and MRSA (p = 0.45 and p = 0.06, respectively). Overall, MRSA colonization was significantly higher in children <12 years of age (odds ratio [OR] = 1.6, 95% confidence interval [CI] 1.1–2.3) compared to older participants, and lower in Caucasians (OR = 0.7, 95% CI 0.4–1.0) than in other racial groups (Supplementary Table S6). At the household level, 125 (83%) and 89 (59%) households had at least one household member colonized with S. aureus and MRSA, respectively (Supplementary Table S7).
By anatomic site, 190 (28%), 72 (11%), and 127 (19%) participants were colonized by S. aureus in the nares, axillae, and inguinal folds, respectively (15%, 6%, and 11% with MRSA, respectively). Eighty-eight (13%) participants were colonized with S. aureus at multiple body sites (7% with MRSA at multiple sites). Of 481 participants not colonized with S. aureus in the nares, 85 (18%) were colonized with S. aureus at an extranasal site (7% with MRSA).
Antibiotic susceptibility and molecular strain typing
Of 389 colonizing isolates, 56% (218) were MRSA, the majority of which were SCCmec type IV (98%, 214), typical of US epidemic CA-MRSA (Supplementary Table S8). Of 171 colonizing MSSA isolates, 40% (69) possessed the SCCmec element, with 25% (42) harboring a residual type III element and 12% (20) harboring a type I element. All infecting isolates available for molecular typing were MRSA SCCmec type IV. All infecting MRSA isolates were susceptible to trimethoprim-sulfamethoxazole, rifampin, linezolid, and ceftaroline, while 93%, 15%, and 46% were clindamycin, erythromycin, and ciprofloxacin-susceptible, respectively.
Household strain richness
Up to three strain types were found to colonize a single participant (of those colonized, median = 1). Of 150 households, 59% (89) harbored at least one colonizing MRSA strain type; 47% (70) had at least one colonizing MSSA strain type. Only 23% (34) of households harbored both MRSA and MSSA strains. The median number of S. aureus strain types recovered per household was one (range 0–7), with an average of 0.37 unique strain types per person (Supplementary Table S9). Of 81 households with ≥2 members colonized, 75% (61) harbored ≥2 unique strain types (mean 2.3 ± 1.2). Sampling season, household cleanliness rating, living in a house (vs. apartment/condominium/trailer), and home ownership (vs. renting) were not significantly associated with strain richness (p > 0.05 by the Kruskal–Wallis test). However, households with ≥5 individuals exhibited a significantly increased number of strain types compared to smaller households (mean 1.8 vs. 1.2 strains, p < 0.001, Wilcoxon signed-rank test). The number of individuals correlated with the number of unique strains (Spearman’s ⍴ = 0.35, p < 0.001), and was even more significant when considering only colonized individuals (Spearman’s ⍴ = 0.77, p < 0.001).
Colonization with the index patient infecting strain type across household members
Ninety-one (61%) isolates from the infection prompting enrollment (infecting strain) were acquired from the hospital laboratory and subjected to molecular typing. At enrollment (median 20 days from SSTI), 27 (30%) of these index patients were colonized with their infecting strain (Fig. 1). Of 298 household contacts of index patients with an available infecting isolate, 62 (21%) were colonized with the infecting strain. Parents had the lowest prevalence of colonization with the infecting strain (22% for mothers, 19% for fathers), while siblings were more commonly colonized (28%) with the infecting strain. Fifty-two (57%) households had at least one individual colonized with the infecting strain. In 41 (45%) households, the infecting strain was the most common strain type recovered from household members. Of the 64 (70%) households in which the index patient was not colonized with the infecting strain, at least one household contact was colonized with this strain in 22 (34%) households.
As the infecting strain was commonly present within households, we constructed a generalized linear-Poisson model examining the degree of anatomical site colonization (nares, axillae, inguinal folds) with the infecting strain across households with an infecting isolate available for typing, the “Infecting Strain Prevalence” model (Supplementary Table S10). Seasonality (as measured by monthly low temperature at time of enrollment)30, specifically warmer months, was significantly associated with presence of the infecting strain (rate ratio per unit increase 1.6, 95% credible interval [CrI] 1.1–2.2). The proportion of household members reporting bathing at least daily was significantly associated with a reduced household burden of the infecting strain (rate ratio for daily bathing 0.3, 95% CrI 0.1–0.8). Time between index patient SSTI and enrollment (colonization sampling) and the number of household members reporting recent SSTI were not associated with increased infecting strain burden.
Factors associated with individual colonization
To determine the relative impact of collective household vs. individual behaviors upon individual colonization, three models measuring “household preventability” (proportion of variance explained through a household-level random effect) were constructed.29 Household preventability was lowest for S. aureus colonization (21%, 95% CrI 10–33%), moderate for MRSA colonization (38%, 95% CrI 24–52%), and highest for infecting strain colonization (51%, 95% CrI 34–66%). These models indicate that individual attributes and behaviors primarily determined S. aureus colonization, while MRSA colonization and particularly colonization with the infecting strain type were equally driven by individual attributes (e.g., health status, age, hygiene) and household attributes (e.g., overall cleanliness, distribution, and number of individuals).
Observing that individual practices governed a significant degree of individual S. aureus colonization, a univariate analysis of all individual covariates was conducted for index patients and household contacts (Table 2; see Supplementary Table S11 for all measured covariates). Measures of proximity were most significantly associated with colonization across household members, with S. aureus- or MRSA-colonized individuals significantly more likely to share a personal hygiene item or bedroom with another S. aureus- or MRSA-colonized individual, respectively. Frequent bathing (≥1× per day) was significantly associated with decreased MRSA colonization. Anatomic site colonization pressure, measured as the proportion of sites (nares, axillae, inguinal folds) colonized across household members (excluding the person of interest), was significantly associated with increased individual colonization for both S. aureus and MRSA colonization. Household strain richness per person (i.e., the number of unique strains measured by repPCR normalized to the number of individuals in the household) was significantly associated with individual S. aureus, but not MRSA, colonization.
Colonization pressure model
We sought to understand the extent to which colonization pressure and strain richness, defined as the number of unique strain types by repPCR per person in the household, predict colonization risk. Increasing anatomical site S. aureus colonization pressure of household contacts (OR 1.4, 95% CrI 1.2–1.5) and renting (vs. owning) dwelling (OR 1.2, 95% CrI 1.0–1.5) were significantly associated with individual S. aureus colonization (Table 3). Higher household contact anatomical site MRSA colonization pressure (OR 1.8, 95% CrI 1.6–2.1) was also predictive of MRSA colonization. Antibacterial soap usage (OR 0.8, 95% CrI 0.6–0.97), increasing age (OR 0.9, 95% CrI 0.8–0.98), and increasing strain richness (OR 0.5, 95% CrI 0.3–0.9) were significantly associated with a lower incidence of individual MRSA colonization.
Colonization proximity model
We next assessed colonization in terms of “proximity models” to understand how sharing household spaces, such as a bedroom or bed, and objects, such as towels or personal hygiene items, with colonized individuals increases colonization risk. In these models, renting (vs. owning) dwelling (OR 1.5, 95% CrI 1.1–1.9) was significantly associated with S. aureus colonization. Sharing a bedroom with an MRSA colonized individual (OR 1.5, 95% CrI 1.1–2.2) and seasonality (as measured by monthly low temperature at enrollment; OR 1.2, 95% CrI 1.01–1.4 per unit increase)30 were significantly associated with MRSA colonization (Table 3). Frequent bathing was associated with decreased likelihood of MRSA colonization (OR 0.7, 95% CrI 0.6–0.98). Although considered, sharing hygiene items or a bed with colonized individuals were not selected in the final models.
Colonization activity model
While previous models focused primarily upon how the degree and distribution of S. aureus influences colonization, household demographics and individual activities may influence colonization. “Activity models” assessed modifiable practices that may reduce S. aureus colonization risk in the community while accounting for socioeconomic status (SES) and demographics. In these models, renting dwelling (vs. owning) was significantly associated with both S. aureus colonization (OR 1.5, 95% CrI 1.1–2.0) and MRSA colonization (OR 1.4, 95% CrI 1.01–2.1) (Table 3). Of note, home ownership was significantly associated with other measures of SES including private health insurance and a college-educated mother (Supplementary Table S12). Antibacterial soap usage was associated with a significant reduction in S. aureus colonization (OR 0.8, 95% CrI 0.6–0.95), while antibacterial soap usage and bathing at least daily each were significantly associated with a reduction in MRSA colonization (OR 0.7, 95% CrI 0.5–0.97 and OR 0.7, 95% CrI 0.5–0.9, respectively). Seasonality was again associated with MRSA colonization (OR 1.2, 95% CrI 1.03–1.5 per unit increase), while it was not associated with overall S. aureus colonization in the activity model (Table 3).
Concordance of colonization strain types among household members
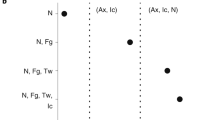
Concordance of S. aureus colonization strain types between household members was considered in the context of shared environments and hygiene items. Figure 2 depicts the frequency at which various pairs of immediate family members were colonized with at least one concordant strain type. Overall, colonization with concordant strains occurred in 12% of all pairs of individuals living within the same household; siblings (excluding the index patient) exhibited the highest strain concordance (17%), closely followed by sibling–parent pairs (15%). Of the 284 pairs of individuals both colonized with S. aureus, 64% (168) were colonized with concordant strain types. Colonized siblings exhibited the highest concordance with another colonized household member, followed by parents and then index patients at 62% (62), 61% (66), and 56% (32), respectively (all pairwise comparisons not significant). History of SSTI was not associated with strain concordance.
Colonization concordance between immediate family members. Concordance defined as two individuals colonized with ≥1 of the same S. aureus strains by repPCR. Listed is percentage concordance (number of concordant pairs over total observed pairs). Overall concordance across all family members was 15% (156/1074). Symbols: (M)ale parent, (F)emale parent, (S)ibling, (I)ndex patient. Sex of index patients and siblings could be either male or female. Parents and siblings could be biologically related or step-parents/step-siblings
Factors that contributed to strain concordance were measured through considering pairs of individuals within households in a generalized linear mixed logistic regression model accounting for a household-level random effect (Supplementary Table S13; see Supplementary Table S3 for covariates used). Strain concordance between immediate family members was significantly higher than pairs of unrelated individuals (OR 3.4, 95% CrI 1.1–10.5). Although sharing bath towels, bedrooms, beds, and personal hygiene items (e.g., razor, cosmetics) were considered in the models, only considering all of these objects in aggregate was significantly associated with colonization with concordant strains (OR 2.7, 95% CrI 1.2–6.6). Household preventability in this model was high at 71% (95% CrI 53–85%), meaning that household-level activities and properties (such as overall cleanliness and crowding), rather than behaviors or attributes shared by the two individuals (such as sharing a bed), may have heavily influenced whether two individuals were colonized by the same strain.
Discussion
S. aureus SSTIs are difficult to prevent and treat, both in terms of primary and recurrent infection, due to the pathogen’s capacity to both stably colonize and reinfect the host over time. The development of future prevention strategies must address both the eradication of extant colonization as well as the prevention of recolonization and recurrent infection. The present study illuminates household S. aureus and MRSA colonization in terms of strain richness, strain concordance between household contacts, and critically, prevalence of the infecting strain in the household following index patient treatment.
Proximity to colonized individuals is a primary risk factor for S. aureus colonization, although it is unclear to what extent physical contact vs. interaction with common fomites contributes to such risk. Previously, S. aureus colonization pressure was shown to be associated with increased risk for colonization,20 and while recapitulated in the present models, colonization pressure does not specify the routes contributing to colonization. Here, we have demonstrated that proximity to colonized individuals, through sharing a bedroom, was critical in predicting MRSA colonization. As only 42% of the individuals reporting sharing a bedroom also shared a bed, simply sharing a bedroom (even without sharing a bed) with a colonized individual may be sufficient to increase MRSA colonization risk. Our models have also highlighted that household members who share personal hygiene items have an increased likelihood of colonization with concordant S. aureus strains. Intervention strategies that promote discrete items (e.g., towels) for each household member may therefore decrease household contact colonization and augment the efficacy of household decolonization strategies.
Atmospheric temperature (modeled as monthly average low temperature) was associated with a significantly increased prevalence of the infecting strain in the household as well as individual MRSA colonization risk. In a recent study across 20 geographically diverse regions in the United States, higher relative humidity, but not temperature, was significantly correlated with MRSA colonization of ICU patients.31 However, two other studies evaluating the impact of meteorological factors upon MRSA SSTIs in outpatients in India and the southwest US found significant correlation between higher temperature and incidence of MRSA SSTIs.32,33 Rather than climate directly increasing incidence of MRSA colonization and infection, it may be that increased physical activity and other behaviors associated with warmer months influence this phenomenon.
MRSA infecting strains were pervasive among household members following index patient treatment, representing the predominant strain in 45% of households. Overall, 57% of households had at least one person colonized with the infecting strain, and 34% of households had at least one person other than the index patient colonized with the infecting strain. A study in New York also found 37% of household contacts colonized with the infecting strain (determined by spa typing).13 When considering family relationships, siblings of the index patient were most likely to harbor the infecting strain (30%), followed by parents (21%), reflecting individuals most likely to be in close proximity to the index patient. A study from Chicago and Los Angeles examining S. aureus skin infection in children and adults observed only 14% of household members colonized with the infecting strain over a similar timeframe between infection and colonization sampling.16 The present study provides evidence that, rather than a transient invader of the index patient, the infecting strain is capable of persistence and colonization of multiple individuals within the household after SSTI treatment.
Across a wide range of personal hygiene practices, health history, and household behaviors, only primary measures of hygiene (bathing frequency) and seasonality were highly significant in predicting colonization burden of the infecting strain across household members. A meta-analysis by Knox et al. found that the number of household contacts colonized by the infecting strain was positively associated with the number of children present in the household and negatively associated with the number of days from index patient SSTI to collection of household contact colonization cultures.34 In our models, both of these covariates were examined and neither were found significant; of note, neither of the covariates found significant in our study (bathing frequency and seasonality) were examined in the meta-analysis. Further, this meta-analysis examined studies that only sampled nares colonization, classified the infecting strain through spa typing, and surveyed households after a longer time from initial infection (33–114 days vs. 3–95 days in the present study). This discrepancy highlights the need to study the longitudinal colonization patterns of the infecting strain when considering measures to reduce colonization and SSTIs.
Modifiable behaviors to reduce MRSA colonization (specifically infecting strain persistence and transmission) within the household are especially important to clinicians and patients to mitigate the burden of recurrent SSTI. Of the many hygiene behaviors examined in the present study, bathing frequency and using antibacterial soap (of note, several active ingredients of these agents have recently been banned by the FDA35) were significantly associated with lower colonization prevalence across multiple models, while sharing a bedroom correlated with higher prevalence of colonization. Nerby et al. reported a similar reduction in MRSA colonization with antibacterial soap usage.36 In a laboratory study by Honisch et al., laundering S. aureus-contaminated test swatches in colder temperatures resulted in low staphylococcal clearance (<4 logs) and more frequent cross-contamination of sterile swatches.37 In our study, the reported water temperature used to launder clothing and linens was not significantly associated with individual S. aureus or MRSA colonization. These contrary results could reflect a high correlation of hygiene behaviors; for example, bathing at least daily could be an indicator of other healthy hygiene practices or antibacterial soap usage may indicate a desire for decolonization, which could ultimately reduce MRSA burden.
Strengths and Limitations
While our study evaluated strain-level resolution of individual S. aureus colonization within households, this is only a cross-sectional snapshot into what may be a highly variable, random system. Ongoing studies of longitudinal strain-level persistence and transmission will be informative. As each household was enrolled only after the index patient presented with an MRSA infection, determining the directionality of transmission of the infecting strain was not feasible. Given that enrollment relied on at least one child presenting with an MRSA infection, our results must be considered within the context of households that include children. While specific hygiene practices have been correlated with colonization, randomized controlled trials are necessary to verify the efficacy of such practices prior to their widespread implementation. Crucial strengths of our study are the large sample size of 150 households (671 participants) in a geographically (urban and rural) and sociodemographically diverse region across metropolitan St. Louis, comprehensively surveyed for behavioral, hygiene, and health history combined with molecular identification of all available S. aureus isolates. These data allow for measures of strain richness, concordance, and infecting strain prevalence in households, as well as the delineation of possible intervention strategies to reduce MRSA colonization within the community.
Conclusions
Combining strain-level molecular typing with a comprehensive survey of personal hygiene, proximity, and physical activity measures provides a thorough analysis of both strain colonization and concordance across a large cohort while distilling key preventive measures to reduce MRSA colonization burden. We have found that the MRSA strain recovered from the index patient infection commonly persists among household members past initial treatment. These findings can inform the guidance provided by clinicians regarding bathing frequency and avoiding sharing personal hygiene items. As seasonality has also been associated with MRSA colonization across multiple studies, clinicians may want to emphasize preventive efforts, including decolonization, during the summertime in patients prone to recurrent SSTI. Future studies are necessary to understand how infectious strains persist in light of such hygiene practices and decolonization strategies in order to reduce the incidence of infection in the community setting.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Agency for Healthcare Research and Quality.
References
Dukic, V. M., Lauderdale, D. S., Wilder, J., Daum, R. S. & David, M. Z. Epidemics of community-associated methicillin-resistant Staphylococcus aureus in the United States: a meta-analysis. PloS ONE 8, e52722 (2013).
Moran, G. J. et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N. Engl. J. Med. 355, 666–674 (2006).
Otto, M. Community-associated MRSA: a dangerous epidemic. Future Microbiol. 2, 457–459 (2007).
Knox, J., Uhlemann, A.-C. & Lowy, F. D. Staphylococcus aureus infections: transmission within households and the community. Trends Microbiol. 23, 437–444 (2015).
Alam, M. T. et al. Transmission and microevolution of USA300 MRSA in U.S. households: evidence from whole-genome sequencing. mBio 6, e00054–15 (2015).
Fritz, S. A. et al. Household versus individual approaches to eradication of community-associated Staphylococcus aureus in children: a randomized trial. Clin. Infect. Dis. 54, 743–751 (2012).
Diep, B. A. et al. Emergence of multidrug-resistant, community-associated, methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men. Ann. Intern Med. 148, 249–257 (2008).
Wertheim, H. F. L. et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 5, 751–762 (2005).
Fritz, S. A., Epplin, E. K., Garbutt, J. & Storch, G. A. Skin infection in children colonized with community-associated methicillin-resistant Staphylococcus aureus. J. Infect. 59, 394–401 (2009).
Nouwen, J. L. et al. Predicting the Staphylococcus aureus nasal carrier state: derivation and validation of a “culture rule." Clin. Infect. Dis. 39, 806–811 (2004).
Costello, E. K. et al. Bacterial community variation in human body habitats across space and time. Science 326, 1694–1697 (2009).
Kluytmans, J., van Belkum, A. & Verbrugh, H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin. Microbiol Rev. 10, 505–520 (1997).
Knox, J. et al. Environmental contamination as a risk factor for intra-household Staphylococcus aureus transmission. PloS ONE 7, e49900 (2012).
Uhlemann, A.-C. et al. The environment as an unrecognized reservoir for community-associated methicillin resistant Staphylococcus aureus USA300: a case-control study. PloS ONE 6, e22407 (2011).
Fritz, S. A. et al. Staphylococcus aureus colonization in children with community-associated Staphylococcus aureus skin infections and their household contacts. Arch. Pediatr. Adolesc. Med. 166, 551–557 (2012).
Miller, L. G. et al. Staphylococcus aureus colonization among household contacts of patients with skin infections: risk factors, strain discordance, and complex ecology. Clin. Infect. Dis. 54, 1523–1535 (2012).
Liu, C. et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin. Infect. Dis. 52, 285–292 (2011).
Kaplan, S. L. et al. Randomized trial of “bleach baths” plus routine hygienic measures vs. routine hygienic measures alone for prevention of recurrent infections. Clin. Infect. Dis. 58, 679–682 (2014).
Fritz, S. A., Garbutt, J., Elward, A., Shannon, W. & Storch, G. A. Prevalence of and risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network. Pediatrics 121, 1090–1098 (2008).
Rodriguez, M., Hogan, P. G., Krauss, M., Warren, D. K. & Fritz, S. A. Measurement and impact of Staphylococcus aureus colonization pressure in households. J. Pediatr. Infect. Dis. Soc. 2, 147–154 (2013).
Halliday, G. & Snowdon, J. The Environmental Cleanliness and Clutter Scale (ECCS). Int Psychogeriatr. 21, 1041–1050 (2009).
Fritz, S. A. et al. Contamination of environmental surfaces with Staphylococcus aureus in households with children infected with methicillin-resistant S aureus. JAMA Pediatr. 168, 1030–1038 (2014).
Cockerill, F. R. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-third Informational Supplement; M100 - S23 (CLSI, Wayne, PA, 2013).
Boye, K., Bartels, M. D., Andersen, I. S., Møller, J. A. & Westh, H. A new multiplex PCR for easy screening of methicillin-resistant Staphylococcus aureus SCCmec types I-V. Clin. Microbiol Infect. 13, 725–727 (2007).
Rodriguez, M. et al. Discriminatory indices of typing methods for epidemiologic analysis of contemporary Staphylococcus aureus strains. Medicine 94, e1534 (2015).
Del Vecchio, V. G. et al. Molecular genotyping of methicillin-resistant Staphylococcus aureus via fluorophore-enhanced repetitive-sequence PCR. J. Clin. Microbiol. 33, 2141–2144 (1995).
R Core Team. R: A Language and Environment for Statistical Computing. [Internet] (R Foundation for Statistical Computing, Vienna, Austria; 2016). Available at https://www.R-project.org/
Waskom, M., et al. Seaborn: V0.8.0 (Zenodo, 2017).
Wang, K., Gaitsch, H., Poon, H., Cox, N. J. & Rzhetsky, A. Classification of common human diseases derived from shared genetic and environmental determinants. Nat. Genet. 49, 1319–1325 (2017).
Arguez, A. et al. NOAA’s 1981–2010 U.S. climate normals: an overview. Bull. Am. Meteorol. Soc. 93, 1687–1697 (2012).
Blanco, N. et al. Effect of meteorological factors and geographic location on methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci colonization in the US. PloS One 12, e0178254 (2017).
Wang, X., Towers, S., Panchanathan, S. & Chowell, G. A population based study of seasonality of skin and soft tissue infections: implications for the spread of CA-MRSA. PloS ONE 8, e60872 (2013).
Sahoo, K. C. et al. Climatic factors and community-associated methicillin-resistant Staphylococcus aureus skin and soft-tissue infections - a time-series analysis study. Int J. Environ. Res Public Health 11, 8996–9007 (2014).
Knox, J. et al. Community-associated methicillin-resistant Staphylococcus aureus transmission in households of infected cases: a pooled analysis of primary data from three studies across international settings. Epidemiol. Infect. 143, 354–365 (2015).
Food and Drug Administration. Fischer, A. Press Announcements - FDA issues final rule on safety and effectiveness of antibacterial soaps (2016) https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm517478.htm.
Nerby, J. M. et al. Risk factors for household transmission of community-associated methicillin-resistant Staphylococcus aureus. Pediatr. Infect. Dis. J. 30, 927–932 (2011).
Honisch, M., Stamminger, R. & Bockmühl, D. P. Impact of wash cycle time, temperature and detergent formulation on the hygiene effectiveness of domestic laundering. J. Appl. Microbiol. 117, 1787–1797 (2014).
Acknowledgements
We thank Meghan Wallace and Angela Shupe for their assistance with molecular strain typing. For their assistance in patient referral, we acknowledge Mary Bixby, RN, Cardinal Glennon Children’s Hospital; Rachel Orscheln, MD, Washington University; Jennifer Seigel, RN, PNP, and the St. Louis Children’s Hospital Pediatric Ambulatory Wound Service staff; and Jane Garbutt, MB, ChB, Sherry Dodd, and the physicians and staff of participating Washington University Pediatric and Adolescent Ambulatory Research Consortium practices, including Mercy Clinic Pediatrics – Union and Washington, Johnson Pediatric Center, Heartland Pediatrics, Forest Park Pediatrics, Tots Thru Teens, Pediatric Healthcare Unlimited, Northwest Pediatrics, Esse Health Pediatric & Adolescent Medicine – Watson Road, Fenton Pediatrics, Blue Fish Pediatrics, and Southwest Pediatrics. We appreciate the thoughtful review of this manuscript by David Hunstad, MD. This work was supported by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital [to S.A.F.]; National Institutes of Health/National Institute of Allergy and Infectious Diseases [grant number K23-AI091690 to S.A.F.]; the National Center for Advancing Translational Sciences at the National Institutes of Health [grant number UL1-TR002345 to S.A.F.]; the Agency for Healthcare Research and Quality [grant numbers R01-HS021736, R01-HS024269 to S.A.F.]; and the Burroughs Wellcome Foundation Investigators in the Pathogenesis of Infectious Disease Award [to J.B.W.]. The computational analysis was partially funded by DARPA Big Mechanism program under ARO contract W911NF1410333 [to A.R.]; by NIH grants R01HL122712, 1P50MH094267, U01HL108634 [to A.R.]; and a gift from Liz and Kent Dauten [to A.R.]. These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mork, R.L., Hogan, P.G., Muenks, C.E. et al. Comprehensive modeling reveals proximity, seasonality, and hygiene practices as key determinants of MRSA colonization in exposed households. Pediatr Res 84, 668–676 (2018). https://doi.org/10.1038/s41390-018-0113-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0113-x
This article is cited by
-
Transmission routes of antibiotic resistant bacteria: a systematic review
BMC Infectious Diseases (2022)
-
Effect of climate on surgical site infections and anticipated increases in the United States
Scientific Reports (2022)
-
Early development of the skin microbiome: therapeutic opportunities
Pediatric Research (2021)
-
Changing epidemiology of methicillin-resistant Staphylococcus aureus in a low endemicity area—new challenges for MRSA control
European Journal of Clinical Microbiology & Infectious Diseases (2020)
-
Prevention Strategies for Recurrent Community-Associated Staphylococcus aureus Skin and Soft Tissue Infections
Current Infectious Disease Reports (2019)